By some estimates, up to 70 percent of patients with Alzheimer’s disease (AD) will experience agitation associated with the illness. Currently there is no FDA-approved drug therapy to alleviate this problem, but two high-quality studies and accumulating data appear to be closing in on effective treatment options.
Second-generation antipsychotics and antidepressants have been widely used off-label despite their serious risks to frail elderly patients who already have compromised organ functions. In particular, all antipsychotic drugs carry a boxed warning in package inserts stating that “elderly patients with dementia-related psychosis” are at increased risk of death.
One of the most notable studies on agitation is the CitAD trial, a randomized, placebo-controlled, double-blind clinical trial
published February 19, 2014, in
JAMA. Anton Porsteinsson, M.D., director of the University of Rochester Alzheimer’s Disease Care Research and Education Program, and colleagues compared 186 elderly patients with probable AD and clinically significant agitation who took citalopram (30 mg) or placebo daily for nine weeks. Patients on citalopram showed greater reduction in agitation symptoms than those on placebo, as measured by the Neurobehavioral Rating Scale agitation subscale. The between-group difference was statistically significant.
While the study was being carried out, the FDA
released an advisory on an increased risk of cardiac abnormality associated with citalopram use. Elderly patients are recommended to limit the dose to 20 mg daily. In the
JAMA study, the authors acknowledged in the study that the efficacy of 20 mg citalopram is unclear. At 30 mg, the researchers did observe a prolongation of QT interval averaging 18.1 ms, which suggests that a cardiac risk should be considered. The study also raised the possibility of reduced cognitive function in patients receiving citalopram compared with placebo, although the difference was very small.
More recently,
JAMA published the results of a randomized, placebo-controlled, double-blind trial that suggests dextromethorphan/quinidine (DM/Q) may offer another option for AD patients for agitation.
The combination formulation of dextromethorphan hydrobromide (20 mg) and quinidine sulfate (10 mg) is already approved for the treatment of pseudobulbar affect, a neurological disorder marked by involuntary or uncontrollable episodes of laughing and crying. The trial was funded by Avanir Pharmaceuticals, a southern California-based company marketing DM/Q and pursuing an additional indication for agitation in AD.
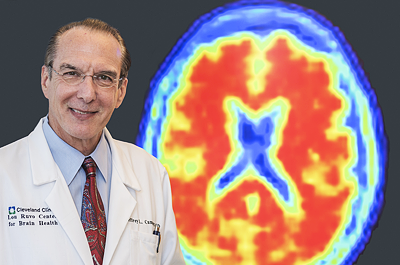
In the study, researchers led by Jeffrey Cummings, M.D., director of the Cleveland Clinic Lou Ruvo Center for Brain Health, compared DM/Q with placebo in 220 patients with probable AD and clinically significant agitation. After treatment with DM/Q (dextromethorphan hydrobromide [20 mg] and quinidine sulfate [10 mg]) daily for up to 10 weeks, DM/Q led to a greater reduction of symptoms, as measured by the Neuropsychiatric Inventory (NPI) Agitation/Aggression score, compared with placebo. Patients on DM/Q had higher risks of falls, diarrhea, and urinary tract infection than those on placebo, but there were no apparent signs of cognitive impairment or QT prolongation.
Several other drugs have been reported in case reports and small studies as treatment options for agitation in AD, including opioids, carbamazepine, and prazosin, but none has been tested in large, randomized, placebo-controlled clinical trials. Otsuka Pharmaceuticals and Lundbeck are conducting a phase 3 trial of brexpiprazole to treat agitation associated with AD.
“Agitation is common; it occurs eventually in 70 percent of patients with AD,” Cummings told Psychiatric News. While the neurobiology of agitation in AD is still unknown, new evidence implicates pathology in the frontal lobe.
Experts advise that nonpharmacological interventions—such as increasing social interactions and pleasant activities, managing discomfort and pain, and minimizing stressful situations or triggers—remain the best first-line approach to managing agitation.
Nevertheless, “a majority of patients with agitation need pharmacotherapy,” said Cummings. He cautioned that physicians should be wary of off-label use of medications, particularly antipsychotics. Despite the promise of new studies, he said, “we are exactly where we were,” because there is still no FDA-approved drug for agitation.
When treating patients for agitation in AD, Cummings advised that clinicians also “appreciate the impact of agitation on the caregiver.” Both of the placebo-controlled studies comparing pharmacotherapies with placebo in patients with agitation revealed a significant placebo effect, he noted, which indicates that patients as well as caregivers had substantial benefits from the psychosocial support provided in the studies.
“We need a full armamentarium of drug therapies,” Cummings said. Even if one or two drugs get approved, “it would be a beginning, but far from the end.” ■