In 1886, Emil Kraepelin described “pseudoreminiscences,” or hallucinations of memory, as images of the imagination as they arise spontaneously in the mind and appearing as reminiscences (
1,
2). In accordance with this description, such false recollections do not correspond to real events of personal history, are not deliberate deceptions, and appear to be distinct from other delusions and confabulations (
3). We evaluated a patient who developed pseudoreminiscences consistent with “fantastic thinking” after frontal strokes, predominantly in the right hemisphere. After the strokes, the patient experienced an ongoing “alternate world” in which he was highly successful and accomplished in many fields.
Case Report
An 81-year-old man was hospitalized because of a 2-year history of the overwhelming experience of an alternate world. His wife reported that he had developed “fantasies that [were] out of control,” and his primary care physician recorded that he traveled in a “parallel” universe. In his new, fantasy world, the patient reported running a successful nonprofit organization that had helped many people, creating a large and successful farm that fed the world, having trillions of dollars along with yachts, a plane, and a famous restaurant, becoming a sheriff who had captured many criminals, and working on a program to save all the wild horses. Previously, he reported being a general who had received two congressional medals, having been the “head” of the United States, and being able to fly like Superman. Perhaps most unusual was his self-report of founding a university specializing in communication between humans and dolphins and the eventual mating of the two species. In his alternate world, he had many extramarital affairs with many beautiful women, resulting in numerous offspring. The longer he talked, the more stories he reported. The patient’s wife stated that at the onset of his alternate world experience, he was confused and disoriented and that he had garbled speech with word-finding difficulty for a period of time.
The patient’s medical history included hypertension, heart failure, hyperlipidemia, polycystic kidney disease, hypothyroidism, lumbosacral spondylosis, and ulcerative colitis. He was hospitalized 1 year previously for confusion and unstable behavior and was found to be anemic as a result of gastric and duodenal ulcers with gastrointestinal bleeding. In addition, the patient had been followed by psychiatrists, with visits every 3–6 months over 9 years, for depression, which was treated with fluoxetine. During prior episodes of depression, he had significant suicidal ideation involving swimming out to sea. The patient’s psychiatrist and wife described him as always having a vivid imagination but no prior episodes of mania, hypomania, or experiences of all-consuming alternate worlds, to the point of frightening his wife.
On interview, the patient admitted to having been obsessed by his other world, which he created out of his dreams. He noted the dreams on awakening and continued to maintain them for hours afterward because he felt that they were “exciting.” At times, he described being semi-awake, blurring his dreams with reality. He expressed concerns that his dream-like state caused his wife significant stress. He denied depression, hallucinations, paranoia, and suicidal ideation. On examination, he was alert, attentive, calm, and cooperative, without evidence of delusions or hallucinations. His mood was normal with congruent affect, and he lacked press of speech or flight of ideas. He scored 26/30 on the Montreal Cognitive Assessment. His forward digit span was 8, and his vigilance was intact as measured using the “A” continuous performance task. Language examination revealed normal fluency and comprehension, and the patient generated 14 animal names in 1 minute. On an auditory verbal learning task, he could recall eight out of 10 words in 15 minutes, and his recognition was totally intact. His constructions, including clock drawing, were also intact, except for minor difficulty with three-dimensional perspective. His performance on frontal systems tasks, such as interpretation of similarities and proverbs, alternating programs, and the go/no-go test, was normal, but he had some difficulty on the Luria hand sequencing test. The patient’s vital signs and general physical examination were unremarkable, but a neurological examination revealed mildly increased tone and decreased fine finger movements in the right upper extremity.
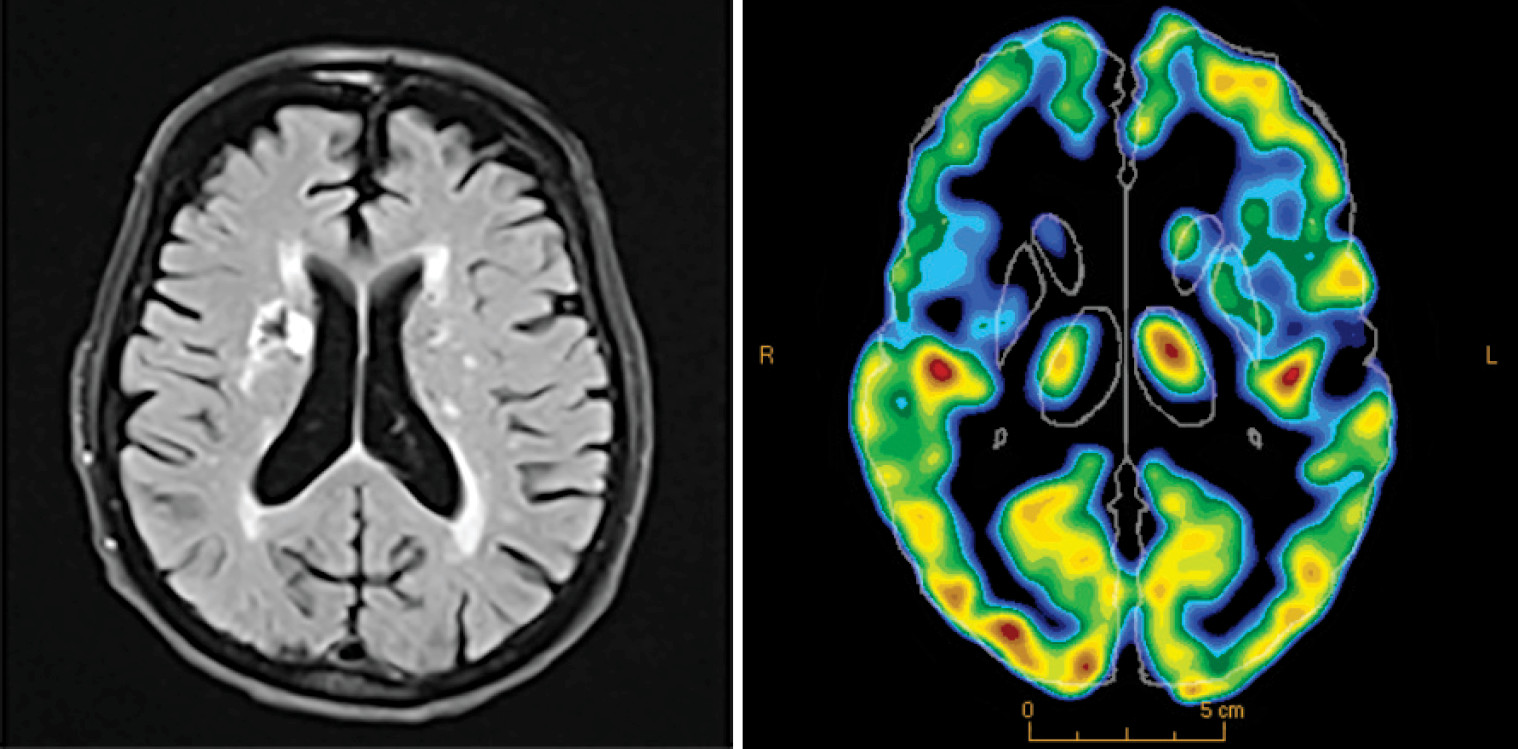
Inpatient diagnostic evaluation and management were initiated. The patient’s routine laboratory findings were normal, except for slight anemia, and a routine EEG was unremarkable. Neuroimaging, including MRI and [
18f]-fluorodeoxyglucose positron emission tomography, showed prior right frontal strokes, other microvascular disease, especially in frontal brain regions, and frontal hypometabolism (
Figure 1). The patient was switched to duloxetine (30 mg q.d.) and mirtazapine (15 mg q.h.s.) without clear change in his preoccupation with his alternate world. On outpatient reassessment 2 weeks later, his alternate world was not as frequently present.
Discussion
The above case suggests that frontal disease can release fantastic thinking, which is distinct from delusions or confabulations and compatible with Kraepelin’s pseudoreminiscences, or imagined pseudomemories (
1,
2). Our patient presented with false narratives with dream-like wish fulfillment associated with cerebrovascular disease and hypometabolism of his frontal lobes, especially in the right hemisphere. Frontal lobe disturbances may facilitate fantastic thinking, possibly from disturbances involving the ventromedial prefrontal cortex (VMPFC), an area involved in detecting false memories and determining real or imagined origin of experience (
5–
9).
Clinicians can distinguish fantastic thinking from delusions and confabulations (
4,
10). A delusion is a fixed belief that is false but firmly held with absolute conviction despite substantial evidence to the contrary (
11). Previous reports have associated delusions with frontal lobe abnormalities, particularly in the right hemisphere and involving the inferior and dorsolateral areas, the heads of the caudate nuclei, and the left temporal lobe (
12,
13). Our patient, however, consistently reported that his false beliefs were truly false, or just in his head, without the external world certainty and consistency seen in delusions.
In contrast, confabulations are false recollections enabling an individual to create a coherent self-narrative (
14). Although confabulations share similarities with delusions, such as external world attribution and associated frontal-executive deficits (
15–
17), they too are distinct (
18,
19). Simple, provoked—or momentary—confabulations are memory-related misstatements resulting from attempts to fill in memory gaps, often in response to questions (
10,
18,
20). They occur in amnestic disorders, such as Wernicke-Korsakoff syndrome and herpes or limbic encephalitis (
10,
21). Spontaneous, fantastic confabulations are rarer grandiose or impossible statements that are internally generated but persist as externally true, despite wavering of certainty when challenged (
17,
22,
23). In contrast to cases involving confabulations, our patient did not have memory impairment, and he acknowledged that his alternate world was imagined.
Our patient’s false narratives were more consistent with fantastic thinking. Investigators have described this phenomenon among patients with frontotemporal dementia (
4). Patients with fantastic thinking have unfettered imaginations, which may be likened to persistent dreaming (
23). Patients with frontotemporal dementia have described this as “thinking [something] may be as good as doing it” (
4). Similarly, our patient knew that his false narratives were internal and felt that they originated from prolonging dreams or daydreaming. In essence, fantastic thinking appears to be the product of creative imagination or vivid dreams that become prominent as a result of frontal disease. Indirect support for a specific association with the VMPFC, especially in the right hemisphere, has been demonstrated in studies showing involvement of this region in detecting false recollections (
7,
9), in determining the external versus internal source of experience (
5,
8), and in deciding whether imagined events are actually experienced (
6). VMPFC dysfunction may facilitate the emergence of imaginative, wish-fulfilling self-narratives in individuals who are prone to vivid imagination. The analysis of the above patient’s false narratives highlights the differences between fantastic thinking and delusions and confabulations, conditions that have corresponding differences in management.