Alterations in markers of cortical gamma-aminobutyric acid (GABA) signaling are among the most widely replicated findings in postmortem brain studies of schizophrenia (
1,
2). In the dorsolateral prefrontal cortex (DLPFC), consistent findings of lower levels of gene products related to GABA neuron signaling converge on the notion that inhibitory neurotransmission signaling is weaker in people with schizophrenia (
1). Lower tissue levels of GABA-related transcripts could be a consequence of lower levels of these transcripts per neuron, fewer neurons that contain these transcripts, or both. Discriminating among these possibilities has major implications both for understanding the pathogenesis of GABA neuron dysfunction in schizophrenia and for developing novel treatment strategies. For example, the possibility of missing neurons in the DLPFC in schizophrenia, due to either incomplete neural migration or excessive neuronal death (
3–
5), has motivated interest in transplantation of embryonic GABA neurons as a therapeutic strategy (
6,
7). In contrast, the alternative view that cortical GABA neurons are present but functionally altered in schizophrenia has motivated efforts to develop therapeutics that augment the function of the affected GABA neuron subtypes (
8,
9). Moreover, this distinction has important implications for the development of animal models useful for the study of schizophrenia, as these model systems should recapitulate the nature of GABA neuron alterations observed in the postmortem brains of people with schizophrenia (
10–
12).
All published studies to date, whether using markers of all GABA neurons or of specific subsets of GABA neurons, have not been able to definitively determine whether lower levels of GABA-related transcripts reflect deficits in expression levels per neuron or in neuron number. Indeed, the first study of the mRNA encoding the 67-kDa isoform of glutamic acid decarboxylase (GAD67) mRNA, a principal GABA-synthesizing enzyme in the cortex, illustrates this challenge (
13). The authors found markedly fewer neurons that were detectable by single-label in situ hybridization for GAD67 mRNA in the DLPFC of people with schizophrenia, findings interpreted as lower expression per neuron given that the density of all Nissl-stained neurons was not altered in the same individuals (
13). However, other investigators reported that the density of small Nissl-stained neurons, presumably GABA neurons, was lower in the DLPFC of people with schizophrenia (
14).
Studies of the subset of GABA neurons that contain the calcium-binding protein parvalbumin (PV) have produced similar interpretive challenges. Although lower levels of PV mRNA in schizophrenia have been confirmed in multiple studies of DLPFC tissue homogenates (
15–
20), the nature of this deficit remains a matter of debate (
1,
5). Studies that measured PV mRNA at a cellular level of resolution reported lower levels of PV mRNA per neuron without a deficit in PV mRNA-positive neuron density (
21,
22), whereas some (
23–
25), but not all (
26–
29), studies of PV protein reported a lower density of PV-immunoreactive neurons in schizophrenia. Interpretive uncertainty also exists for studies of somatostatin (SST), a neuropeptide present in a different subpopulation of cortical GABA neurons. SST mRNA levels are markedly lower in DLPFC tissue homogenates from people with schizophrenia (
15,
17,
18,
30), and the only single-label in situ study reported both fewer SST mRNA-positive neurons and lower SST mRNA levels per positive neuron in schizophrenia (
20).
One possible explanation for these apparently disparate findings is that the levels of the identifying gene products, SST and PV, are lower in many of these GABA neurons in schizophrenia, with levels in some neurons falling below the detectability threshold for the methods employed (
31). In particular, using SST or PV—the levels of which are markedly lower in schizophrenia—as the sole label to identify the neurons of interest, and then quantifying the relative densities of neurons containing each label, conflates the independent and dependent variables and clouds interpretive clarity. Indeed, all previous studies that used single-label methods could not dissociate the presence of SST or PV neurons from the detectability of the identifying transcripts. Thus, counting neurons based on the detectability of a transcript in the presence of lower tissue levels of that transcript means that some neurons could be “missed” even if they are not “missing.”
In this study, we sought to address the challenge of determining whether lower tissue levels of SST and PV mRNAs in schizophrenia are due to lower levels of these transcripts per neuron, fewer neurons that contain these transcripts, or both. To do so, we used a novel multiplex fluorescent in situ hybridization approach to label four mRNA targets simultaneously with cellular resolution. This approach, which has not previously been used in postmortem human brain studies, permits the independent determination of transcript levels per neuron and of neuron density without conflating the two measures. Specifically, proxy markers (i.e., transcripts that are expressed in SST and PV neurons but whose expression in the DLPFC is not altered in schizophrenia [
32–
34]) were used to independently identify SST and PV neurons, and then levels of SST and PV in those neurons were quantified. We focused our analysis on layers 2 and 4 of the human DLPFC, as these layers exhibit the highest density of GABA neurons (
13,
35,
36) and are differentially enriched for SST and PV neurons, respectively (
20,
21,
37). Because the goal of the study was to identify the basis for the SST and PV mRNA deficits, we selected a subset of subjects with schizophrenia known to have pronounced deficits of both transcripts relative to matched unaffected comparison subjects. Given that the only published stereological analysis of total neuron number found a normal complement of neurons in the frontal lobe of people with schizophrenia (
38), we predicted that levels of SST and PV mRNAs per neuron would be lower without a difference in neuron density in schizophrenia.
Methods
Human Postmortem Brain Tissue Specimens
Brain specimens (N=60) were obtained during routine autopsies conducted at the Allegheny County Office of the Medical Examiner (Pittsburgh; N=57) or the Davidson County Medical Examiner’s Office (Nashville; N=3) after consent was obtained from next of kin. An independent team of clinicians made consensus lifetime DSM-IV diagnoses for each subject using the results of an extensive psychological autopsy, including structured interviews with family members and review of medical records as well as toxicology and neuropathology reports (
39). Unaffected comparison individuals had no known history of psychiatric or neurological disorders except for psychiatric diagnoses in remission in one subject (see the footnotes in Table S1 in the
online supplement). The listed race and biological sex of the decedents (
Table 1; see also Table S1) reflect the concurrence of information available in the autopsy report and next of kin interviews. All procedures were approved by the University of Pittsburgh Committee for Oversight of Research and Clinical Training Involving Decedents and Institutional Review Board for Biomedical Research.
As discussed above, our goal in this study was to investigate the nature of DLPFC SST and PV mRNA deficits in schizophrenia. We therefore constructed a biased cohort of individuals with schizophrenia who had documented deficits in both SST and PV mRNAs. In a previous study (
15), SST and PV mRNA levels were measured using quantitative polymerase chain reaction (qPCR) in DLPFC total gray matter homogenates from 62 subject pairs of individuals with schizophrenia and matched unaffected comparison individuals. From that study, we selected a subset of 30 subject pairs in which the individuals with schizophrenia had the most pronounced deficits in both transcripts. In this cohort, the mean deficit in the schizophrenia group was 50.1% for SST mRNA levels and 36.7% for PV mRNA levels in the DLPFC. The paired design, in which each schizophrenia sample was matched to one unaffected comparison sample for sex and as closely as possible for age (see Table S1 in the
online supplement), was employed to reduce biological variance between groups and to control for experimental variance at every stage of the experiment. Mean age, postmortem interval, RNA integrity number, storage time at −80°C, or the distribution of race did not differ significantly between groups (
Table 1). Although brain pH significantly differed between groups, the mean difference was 0.2 pH units and is of uncertain biological significance.
Fluorescent In Situ Hybridization Tissue Labeling
For each subject, fresh-frozen coronal tissue blocks containing right DLPFC area 9 were mounted in a cryostat, and sections 20 μm in thickness were cut, thaw-mounted onto SuperFrost slides (ThermoFisher Scientific, Waltham, Mass.), and stored at −80°C until tissue labeling. mRNA probes were designed by Advanced Cell Diagnostics, Inc. (Hayward, Calif.) to detect mRNAs encoding SST (gene symbol
SST, HGNC ID:11329), PV (gene symbol
PVALB, HGNC ID:9704), SRY-box transcription factor 6 (SOX6; HGNC ID:16421), and the vesicular GABA transporter (VGAT; gene symbol
SLC32A1, HGNC ID:11018) (see Table S2 in the
online supplement). VGAT was used as a GABA neuron marker because it is expressed by all GABA neurons but no other cell types, and levels of VGAT mRNA are unaltered or only modestly lower in the DLPFC of people with schizophrenia (
33,
34). SOX6 (
40,
41), which is selectively expressed in SST and PV neurons as a result of their shared embryonic origin in the medial ganglionic eminence and which continues to be robustly expressed in the adult primate neocortex (
42), was used to distinguish SST and PV neurons from other GABA neurons. For details on probe fluorophore assignments and mRNA labeling protocols, see the Methods section in the
online supplement.
Sampling
Images were collected on a custom widefield Olympus IX83 inverted microscope (Olympus, Center Valley, Pa.) equipped with a six-line (350-, 405-, 488-, 568-, 647-, 750-nm) Spectra III light engine (Lumencor, Beaverton, Ore.). The present study focused sampling on layers 2 and 4 for imaging, as these layers are known to be differentially enriched for SST and PV neurons, respectively, in the primate neocortex (
20,
21,
37). Each imaging site was collected as a three-dimensional image stack (two-dimensional images successively captured at intervals separated by 0.25 μm in the z-dimension). Autofluorescence from lipofuscin was imaged in a separate channel, as previously described (
43,
44). See the Methods section in the
online supplement for details on imaging parameters.
Image Processing
For segmenting fluorescent grains, a Gaussian filter was applied for each channel (except the DAPI channel) by calculating a difference of Gaussians using sigma values of 0.7 and 2 in MATLAB, and an average z-projection algorithm was used to generate a two-dimensional representation of the three-dimensional image stack. Lipofuscin was subtracted from the resulting two-dimensional image (see the Methods section in the
online supplement for details). The average lipofuscin levels in both subject groups for VGAT-positive and SOX6-positive neurons in layers 2 and 4 are shown in Figure S1 in the
online supplement. DAPI-labeled nuclei were segmented using a deep learning algorithm, and fluorescent grains were counted within a cellular region of interest constituting the segmented nucleus and a 2-µm perimeter around the nucleus using CellProfiler, version 4.2.0 (
45). Cells were classified based on the specific expression of a given transcript above background levels, and relative transcript levels per cell were quantified as the average grain density per cell (grains/μm
2). See the Methods section in the
online supplement for details on cell segmentation and classification.
Statistical Analysis
Linear mixed models (
46,
47) were used to evaluate diagnostic differences between two dependent measures, the relative density of positive cells, and grain density per cell, for each cell type. These models included main effects of diagnosis, layer, and diagnosis-by-layer interaction. Covariates included age, sex, postmortem interval, pH, and RNA integrity number, with human subject included as a random factor. Tissue storage time at −80°C was not included as a covariate because it was previously shown not to be associated with SST or PV mRNA levels (
15,
33). Within each layer, post hoc testing was conducted using estimated marginal means derived from the mixed model (
48). We report an overall F test for the main effects of diagnosis, layer, and an interaction for each measure, and we report post hoc t tests for within-layer diagnosis effects derived from the main models. Statistical significance was set at an alpha of 0.05. Group differences in grain density per neuron were compared using the average grain density per neuron (grains/μm
2) in each layer per subject. Likewise, analyses of neuron density were conducted on values of neurons/mm
2 in each layer per subject. All statistical analyses and figure generation were conducted in R (
46–
51).
Effect sizes were computed for each dependent measure within a layer using the strategy described by Cohen (
52). Here, a negative effect size indicates a lower value in the schizophrenia group relative to the unaffected comparison group, with effect sizes of 0 to −0.2 defined as nominal, −0.2 to −0.4 defined as small, −0.4 to −0.6 defined as medium, and −0.6 and greater defined as large. Bayes factors were used to evaluate the strength of the evidence in favor of either the alternative or the null hypothesis (
53) and are reported relative to the alternative hypothesis notation, designated as BF
10. We use Jeffrey’s interpretation of Bayes factor values (
54): for evidence in favor of the alternative hypothesis, BF
10 values of 1–3 are considered weak, values of 3–10 are considered strong, values of 10–100 are considered very strong, and values >100 are considered decisive. For evidence in favor of the null hypothesis, BF
10 values of 0.34–0.99 are considered weak, values of 0.10–0.33 are considered strong, values of 0.01–0.10 are considered very strong, and values <0.01 are considered decisive. See the Methods section and tables in the
online supplement for details on Bayes factor analyses, selection of priors, analyses of comorbid factors in individuals with schizophrenia, and complete statistical information from the analysis.
Results
Laminar Distribution of DLPFC GABA Neurons in Unaffected Individuals
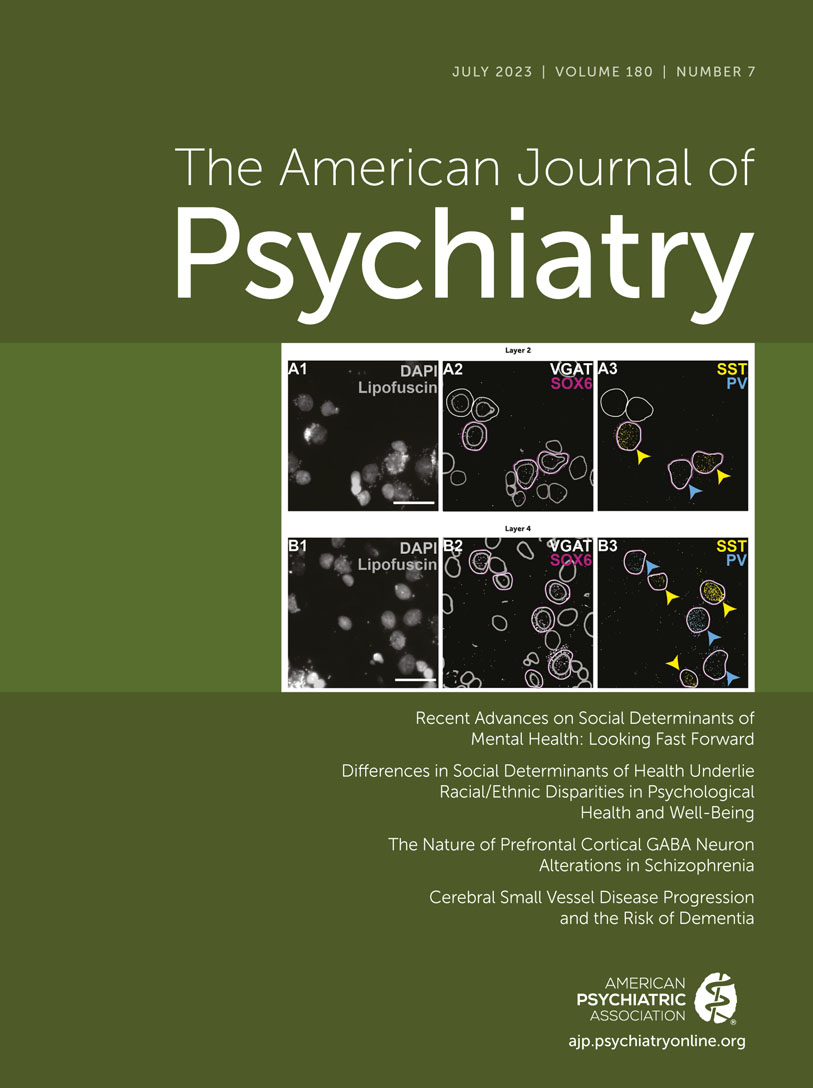
Fluorescent in situ hybridization revealed robust labeling of all four mRNA targets. Most neurons labeled for both VGAT and SOX6 mRNAs (referred to as VGAT+/SOX6+) were either SST or PV mRNA–positive (referred to as SST+ or PV+, respectively) (
Figure 1; see also Figure S2 in the
online supplement). Conversely, most SST+ and PV+ neurons were VGAT+/SOX6+, and, as expected, VGAT+/SOX6− neurons expressed neither SST nor PV (
Figure 1A). For the schizophrenia individual in pair 2 (see Table S1 in the
online supplement), labeling of all four target mRNAs was poor; data from this pair were removed from the analysis.
In the unaffected comparison individuals, the density of VGAT+/SOX6− neurons was greater in layer 2 (mean=56.6 neurons/mm
2, SD=13.9; 9.6% of all layer 2 nuclei) than in layer 4 (mean=28.0 neurons/mm
2, SD=6.8; 4.3% of all layer 4 nuclei), consistent with previous findings that caudal ganglionic eminence–derived interneurons (e.g., those containing calretinin and/or vasoactive intestinal polypeptide [
55]) are enriched in the superficial layers of the primate neocortex (
56). In contrast, the density of VGAT+/SOX6+ neurons was similar in layers 2 (mean=61.9 neurons/mm
2, SD=15.5; 10.5% of all layer 2 nuclei) and 4 (mean=59.9 neurons/mm
2, SD=9.9; 9.2% of all layer 4 nuclei). Among VGAT+/SOX6+ neurons, the density of SST+ neurons was greater in layer 2 (mean=36.0 neurons/mm
2, SD=11.5) than in layer 4 (mean=22.2 neurons/mm
2, SD=5.7), whereas the density of PV+ neurons was greater in layer 4 (mean=31.7 neurons/mm
2, SD=7.0) than in layer 2 (mean=13.4 neurons/mm
2, SD=6.1), findings consistent with previous studies of the differential laminar distribution of SST and PV neurons (
20,
21,
37).
Markedly Lower Levels of SST and PV mRNA per Neuron Without a Deficit in Neuron Density in Schizophrenia
In SST+ neurons, levels of SST mRNA per neuron were lower in individuals with schizophrenia relative to unaffected individuals (F=40.7, df=1,51, p<0.0001) in both layers 2 and 4 (t ratio>5.3, p<0.0001), with large effect sizes (layer 2 effect size=−1.48; layer 4 effect size=−1.64) (
Figure 2A). SST mRNA levels per neuron were lower in the individual with schizophrenia in 24 and 26 pairs in layers 2 and 4, respectively (
Figure 2B). Across all SST+ neurons, the distribution of SST levels per neuron in both layers was left-shifted in schizophrenia (see Figure S3A in the
online supplement). In contrast, the relative density of SST neurons did not differ significantly between subject groups (F=0.001, df=1,51, p=0.97) in either layer 2 or layer 4 (
Figure 2C,D). Bayes factor values strongly supported the evidence of there being no group difference in SST neuron density in either layer (both BF
10 values <0.27). In addition, SST levels per neuron averaged across both layers were positively correlated (r=0.86, p<0.0001) (see Figure S4A in the
online supplement) with SST transcript levels measured previously by qPCR in total tissue homogenates in these same subjects (
15), whereas the density of SST neurons was not (r=0.23, p=0.09) (see Figure S4B in the
online supplement); these comparisons further support the hypothesis that lower tissue levels of SST mRNA in schizophrenia solely reflect lower SST mRNA levels per neuron.
In PV+ neurons, levels of PV mRNA were markedly lower in schizophrenia (F=14.0, df=1,51, p=0.0005). The diagnosis-by-layer interaction was also significant (F=18.7, df=1,56, p<0.0001), reflecting the fact that PV levels were lower in layer 4, with a large effect size (effect size=−1.1), but not in layer 2 (effect size=−0.23), in schizophrenia relative to unaffected individuals (
Figure 3A). In layer 4, levels of PV mRNA per neuron were lower in schizophrenia in 24 of the pairs (
Figure 3B), and the distribution of PV levels per neuron appeared to be left-shifted in schizophrenia (see Figure S3B in the
online supplement). The relative density of PV neurons did not differ significantly between subject groups (F=0.05, df=1,51, p=0.83) in either layer 2 or 4 (
Figure 3C, 3D), and Bayes factor values strongly supported the evidence of no group difference in both layers (both BF
10 values <0.27). In addition, PV levels per neuron in layer 4 were highly correlated (r=0.55, p<0.0001; see Figure S4C in the
online supplement) with PV transcript levels measured previously by qPCR in total tissue homogenates in these same subjects (
15), whereas the density of PV neurons was not (r<0.01, p>0.99) (see Figure S4D in the
online supplement). These comparisons further support the hypothesis that lower tissue levels of PV mRNA in schizophrenia solely reflect lower PV mRNA levels per neuron in layer 4.
Unaltered Density of VGAT+/SOX6+ Neurons in Schizophrenia
To assess the robustness of the finding that the densities of SST and PV neurons were not altered in schizophrenia, we also quantified the density of VGAT+/SOX6+ in both layers, independent of the presence or absence of SST or PV mRNAs. The density of VGAT+/SOX6+ neurons did not differ between diagnostic groups (F=3.1, df=1,51, p=0.08) in either layer 2 (t ratio=−1.8, p=0.08) or layer 4 (t ratio=−1.0, p=0.32) (
Figure 4A,B). In fact, although not significant, the effect size of the group difference in the density of VGAT+/SOX6+ neurons was small but positive in both layers 2 and 4 (effect sizes, 0.37 and 0.23, respectively).
In addition, consistent with previous findings that VGAT and SOX6 mRNA levels in total DLPFC gray matter are not markedly altered in schizophrenia (
32–
34), we did not find evidence of lower VGAT (F=2.0, df=1,51, p=0.17) or SOX6 (F=2.1, df=1,51, p=0.15) mRNA levels per VGAT+/SOX6+ neuron in schizophrenia in either layer (see Figure S5 in the
online supplement).
Influence of Comorbid Factors on SST and PV Levels per Neuron in Schizophrenia
Levels of SST mRNA per neuron in layer 2 or 4, or levels of PV mRNA per neuron in layer 4, in individuals with schizophrenia did not appear to differ on the basis of death by suicide, a diagnosis of schizoaffective disorder, comorbid substance or alcohol use disorder at time of death, or nicotine, antipsychotic, antidepressant, or benzodiazepine/antiepileptic use at time of death (see Figures S6 and S7 in the
online supplement). Here, the comparison for antipsychotics is limited given the small number of individuals with schizophrenia who were not on antipsychotics at time of death. However, previous studies in larger cohorts of individuals with schizophrenia on and off antipsychotics (
15), in individuals with mood disorders taking antipsychotics at time of death (
57), and in monkeys chronically treated with antipsychotics (
16,
20,
21) did not show evidence of altered levels of either SST or PV mRNAs with antipsychotic exposure, strongly suggesting that the findings here do not reflect confounding from antipsychotic use.
Discussion
Deficits in DLPFC tissue levels of SST and PV mRNA have been reported in multiple cohorts of subjects with schizophrenia by several research groups using different quantitative methods (
15–
17,
20,
58–
60). However, the nature of those deficits has been unclear, with some reviews suggesting that schizophrenia is associated with fewer GABA neurons (
5,
61) and others suggesting that GABA neurons are functionally altered but not fewer in number in this illness (
2,
62). However, all of the studies on which these interpretations are based lacked the technical capacity to distinguish between these alternative views. This issue similarly extends to recent studies using new techniques. An analysis of the DLPFC transcriptome at the single-nucleus level of resolution led to the conclusion that there was a lower abundance of GABA neurons in the upper cortical layers, most notably in SST neurons (
63), yet similarly relied on markers of GABA neurons known to be altered in schizophrenia as the identifying features.
Here, using a multilabel fluorescent in situ technique that overcomes earlier technical limitations of brightfield in situ approaches, we demonstrate that schizophrenia is associated with lower SST and PV mRNA levels per neuron in the DLPFC, without any difference in the relative density of either neuron subtype. Even in individuals with schizophrenia who exhibit pronounced deficits in SST and PV mRNA levels in tissue homogenates, we found strong evidence that there are not fewer neurons in those individuals. Thus, the basis for lower tissue levels of SST and PV mRNAs in schizophrenia is lower gene expression per neuron and not fewer neurons. As discussed below, these findings have important implications both for understanding the pathogenesis of GABA neuron alterations in schizophrenia and for the design of therapeutic interventions targeting these alterations.
Novel Multiplex In Situ Hybridization Approaches Clarify the Nature of GABA Neuron Disturbances in Schizophrenia
Previous postmortem studies of SST+ and PV+ neurons have produced mixed findings as to whether the density of these neurons is lower in the DLPFC in schizophrenia. These mixed findings likely reflect multiple technical limitations of these studies (
1). Specifically, in all published studies to date of SST or PV neuron density in schizophrenia, lower gene expression per neuron could have rendered some SST or PV neurons undetectable using the single-label methods employed.
The approach used in the present study includes several important advances that provide a clear picture of the nature of SST and PV mRNA deficits in schizophrenia. First, relative to previous radiolabeled in situ hybridization assays, fluorescent in situ hybridization assays have markedly higher sensitivity and specificity, in part as a result of lower background grain density (
64,
65). For example, using single-label in situ hybridization for SST mRNA in schizophrenia, we previously reported a lower density of SST mRNA–positive neurons (
20); however, the high background labeling of mRNA grains in that study rendered low-expressing neurons difficult to detect. The findings of the present study demonstrate that neurons with low SST expression can be detected with the appropriate experimental design and more sensitive techniques.
We also found that the density of PV mRNA–expressing neurons was not altered in the illness. Thus, previous studies reporting lower densities of PV-immunoreactive neurons in schizophrenia (
5) may have been confounded by a limited ability to detect those neurons given the techniques employed. For example, in the same tissue sections from schizophrenia and unaffected comparison individuals, a deficit in PV neuron density that appeared to be present at lower magnification was clearly not present at higher magnification (
29). Similarly, previous studies that reported a deficit in PV-immunoreactive neuron density using paraffin-embedded sections (
66) were likely confounded by the reduced immunoreactivity associated with that approach (
31), an interpretation supported by findings of no schizophrenia-associated deficits in PV-immunoreactive neuron density in studies using immunohistochemical methods with more robust antigen detection (
27–
29).
Second, even with methodological advances that improve sensitivity for detecting labeled neurons, approaches that rely on visualizing SST or PV alone still conflate the expression level of the indexing transcript with the presence of the neuron. Here, simultaneously labeling for both SST and PV in concert with their colocalization with independent proxy markers of these neurons (VGAT and SOX6) has demonstrated that the densities of SST and PV neurons are not altered in schizophrenia. This interpretation is particularly robust given that we used a cohort of individuals with pronounced deficits in SST and PV mRNA levels in DLPFC total gray matter (
15), which would have maximized the likelihood of detecting a deficit in SST or PV neuron density in schizophrenia if either existed.
Finally, proper interpretation of null results requires more evidence than is available from p values generated by frequentist statistical tests (
53). Bayes factors (
67) provide a quantitative metric for evaluating the strength of the null hypothesis over the alternative. Here, for all findings of neuron density, the statistical null hypothesis was at least three times more likely than the alternative hypothesis, providing strong evidence for no difference in neuron density between subject groups. In contrast, the evidence for the findings of lower SST or PV mRNA per neuron can be considered decisive.
Together, the methods employed here provide multiple advances over previous methods to strongly support the conclusion that SST and PV mRNA expression is lower, but that SST and PV neurons are not missing, in the DLPFC of individuals with schizophrenia. We note that the present study only indexes neuron density, not absolute neuron number, which can only be assessed using stereological methods. However, consistent with the findings here, the only such study to date found no difference in total neuron number in the frontal lobe of people with schizophrenia (
38). Furthermore, we note that our study was not designed to estimate the true effect size of the SST or PV mRNA per neuron deficit, given that we deliberately selected subjects with schizophrenia known to have deficits of SST and PV mRNA levels in tissue homogenates.
Implications for Understanding the Etiology of GABA Neuron Dysfunction in Schizophrenia
Our finding of a normal complement of SST and PV neurons in DLPFC layers 2 and 4 strongly argues that neither excessive neuronal death nor aberrant migration of these GABA neurons is operative in the disease process of schizophrenia. In contrast, the presence of lower levels of both SST and PV mRNAs in schizophrenia is more likely to reflect upstream alterations in the cortical circuit shared by SST and PV neurons. The expression of both SST (
68–
72) and PV (
73,
74) transcripts appears to be influenced by neuronal activity, suggesting that deficient excitatory drive to these neurons in schizophrenia could account for lower SST and PV mRNA levels. In monkey DLPFC, ∼50% of local axon collaterals from layer 3 pyramidal neurons innervate GABA neurons (
75), with most of these synapses targeting PV neurons in layer 4 and most likely SST neurons in layer 2 (
76). In schizophrenia, convergent lines of evidence suggest that layer 3 pyramidal neurons are hypoactive in the DLPFC (
77–
79), suggesting that weaker excitatory drive from layer 3 pyramidal neurons might contribute to the activity-dependent downregulation of SST and PV mRNAs.
Alternatively, these alterations in SST and PV neurons might emerge in early development in individuals who are later diagnosed with schizophrenia. Early environmental insults, such as maternal immune activation, have been reported to alter the properties of SST (
80) and PV (
81) neurons in rodent models, including lower expression of both transcripts. Finally, altered gene expression in SST and PV neurons could reflect independent, cell type–specific alterations in schizophrenia. For example, altered alternative splicing of ErbB4 in PV neurons could lead to fewer excitatory synapses onto these cells and lower PV expression (
28,
82); consistent with this idea, ErbB4 splicing shifts are correlated with PV levels in schizophrenia (
82). Alterations to
N-methyl-
d-aspartate receptors (NMDARs) have been posited to principally affect SST neurons (reviewed in reference
83) and not PV neurons (
84), suggesting that hypofunction of NMDARs in SST neurons may contribute to lower activation of these cells and subsequent downregulation of activity-dependent SST expression.
Finally, it appears unlikely from these and other data that SST and PV mRNA deficits in schizophrenia are secondary to features frequently comorbid with schizophrenia, and thus it appears that they likely reflect the underlying disease process. First, the present study failed to find any significant associations between comorbid factors measured here and SST or PV levels per neuron among individuals diagnosed with schizophrenia. Second, previous studies failed to find evidence of altered SST or PV mRNA levels in monkeys chronically exposed to antipsychotic medications (
16,
21). Third, the levels of VGAT and SOX6 mRNAs were not significantly altered within these same neurons, arguing that the deficit in SST and PV mRNAs is due to the disease process of schizophrenia rather than to ante- or postmortem factors in schizophrenia that contribute to RNA degradation.
Implications for Therapeutic Strategies Targeting Cognitive Dysfunction in Schizophrenia
If deficient inhibitory signaling from DLPFC SST and PV neurons represents part of the neural substrate for cognitive dysfunction in schizophrenia (
85–
87), augmenting the excitability of these neurons could enhance inhibitory capacity and improve cognitive function in the disorder. Our findings of a normal complement of SST and PV neurons suggests that these neurons are viable targets for novel procognitive therapeutic interventions (
88–
91). Some preclinical models provide support for this strategy. For example, a recent study found that positive allosteric modulators acting at mGluR1 receptors preferentially target SST neurons and enhance performance on certain working memory tasks in rodents (
92). Alternatively, if SST and PV neuron alterations are a consequence of diminished excitatory drive from layer 3 pyramidal neurons (
77–
79), then augmentation of pyramidal neuron function, and in turn more robust engagement of inhibitory neurotransmission from SST and PV neurons, could restore normal circuitry activity in the DLPFC of individuals with schizophrenia.
Conclusions
Our study elucidates the nature of SST and PV neuron mRNA deficits in schizophrenia by finding robust evidence for lower gene expression per neuron of both transcripts without deficits in the density of either type of neuron in the DLPFC. These findings have important implications for understanding the schizophrenia-associated pathogenesis of GABA neuron dysfunction, designing and validating animal models useful for the study of the disorder (
10–
12), and informing novel strategies for procognitive therapeutic interventions. The finding that both SST and PV neurons are present in normal complement in schizophrenia encourages the use of methodological strategies employed in the present study to identify novel therapeutic targets that are shared between these cell types or specific to either cell type. The methodological strategies used in this study offer a road map for the conduct of such cell type–specific investigations in the context of schizophrenia.
Acknowledgments
Tissue from some subjects was obtained from the NIH NeuroBioBank at the University of Pittsburgh Brain Tissue Donation Program. The authors are thankful to the members of the Brain Tissue Donation Program at the University of Pittsburgh for their tremendous efforts. They are also grateful to Liban Dinka, Julia Vespoli, and Elizabeth Profozich for their outstanding technical assistance. Finally, the authors are indebted to the families who make this work possible through brain tissue donation.