Reducing access to highly lethal suicide methods has been associated with substantial declines in suicide deaths (
1). Because of their respiratory depression effects and narrow therapeutic window, opioids pose a greater risk than any other drug class of an intentional overdose proving to be lethal (
2), and approximately 40% of overdose suicide deaths in the United States involve opioids (
3). However, the relationship between opioid prescribing and suicide risk is complex. When people have their opioids tapered, they can become desperate if their pain becomes uncontrolled (
4) or if they experience serious withdrawal symptoms (
5), no matter why they received opioids. Long-term opioid exposure can also promote depression, which in turn increases the risk of suicide by any method. Given these complexities, uncertainty surrounds the connection between opioid prescribing and suicide risk, including opioid and non-opioid suicide deaths.
It is not known whether certain opioid prescribing patterns, such as high-dose or long-term prescriptions or having multiple opioid prescribers, are associated with particularly elevated suicide risk. A case-control study of veterans with chronic non-cancer pain found that opioid prescriptions had a significant dose-dependent relationship with risk of suicide, including suicide by overdose (
6). However, a population-based cohort study of adults in Denmark, which may have been inadequately powered, did not reveal a significant association between long-term use of prescription opioids and risk of suicide (
7).
Alongside concerns that some opioid prescribing patterns may directly contribute to suicide risk in susceptible individuals, there are competing concerns that tapering or discontinuing opioids in adults with chronic pain could increase their risk of suicidal behavior (
2). In a cohort study of patients with stable high-dose opioid prescriptions, tapering was associated with an increased risk of medically treated suicide attempts (
8). A second cohort study found that stopping opioid therapy for chronic pain, especially after longer periods of opioid therapy, was significantly associated with a composite measure that included death by suicide or any overdose (
9). Symptoms of depression may also emerge or worsen during tapering of long-term opioid therapy (
10). In the previously mentioned study of veterans, however, the suicide rate among patients who discontinued prescribed opioids was similar to the rate among patients who received low-dose opioids and was lower than that among patients who received high-dose opioids. These findings are not consistent with the hypothesis that opioid discontinuation contributes to suicide risk (
2).
In efforts to reduce opioid overdose deaths in the United States, several policies have been implemented to restrain prescription of opioids (
11–
13), and they have coincided with a decline in opioid prescribing (
14). Several (
15–
17) but not all (
18) population-level studies have reported that lower opioid prescribing is correlated with lower overdose deaths involving prescription opioids. This research has generally focused on unintentional overdoses. One study from Ontario, Canada, however, reported that the regional rate of opioid prescriptions was not significantly related to concurrent opioid-related suicide deaths for men and was only weakly associated for women (
14). Because regions vary in several factors that could contribute to suicide risk, the extent to which local opioid prescribing policies contribute to population-level suicide risk remains unclear.
Given uncertainties surrounding opioid prescribing and suicide risk, we evaluated changes in regional opioid prescribing in relation to changes in overall suicide deaths, including suicide deaths involving opioids. We also examined opioid prescribing in relation to unintentional and undetermined opioid-related overdose deaths. We used fixed-effects models in which geographic regions served as their own controls to evaluate regional changes in total suicide deaths and suicide deaths involving opioids in relation to changes in several measures of opioid prescribing. A greater understanding of these associations might help inform opioid prescription surveillance and clinical practice.
Results
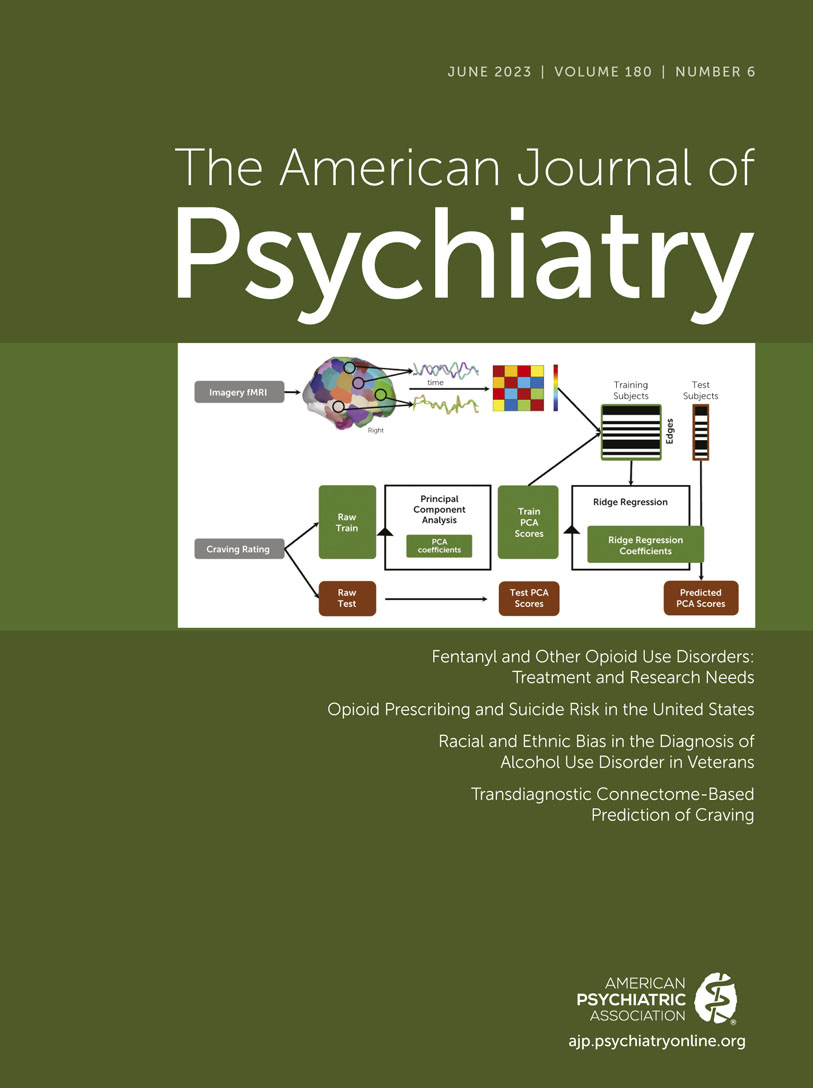
Trends in Opioid Prescribing
Each of the five opioid prescribing measures declined during the 2009–2017 period. Regional opioid prescriptions per 100 persons declined from 70.19 to 61.63; percentage with at least one opioid prescription, from 26.40 to 20.27; percentage filling high-dose prescriptions, from 2.01 to 1.60; percentage filling long-term prescriptions, from 1.24 to 0.96; and percentage filling prescriptions from three or more prescribers, from 3.18 to 2.26 (see Tables S1 and S2 and Figures S1–S3 in the online supplement).
Suicide Deaths
Between 2009 and 2017, the regional rate of total suicide deaths increased from 13.80 to 16.36 per 100,000 persons (difference=2.56, 95% CI=2.05, 3.07) (see Tables S1 and S2 in the
online supplement). Change in total regional suicide deaths was positively associated with change in all five opioid-prescribing measures (
Table 1; see also Figure S4 in the
online supplement). If there had been no decrease between 2009 and 2017 in opioid prescriptions per capita, we estimate that, ceteris paribus, there would have been 3.0% more suicide deaths in 2017. In addition, there would have been an estimated 8.2%, 1.5%, 0.5%, and 4.8% more suicide deaths in 2017, respectively, had there been no decrease in the percentage with at least one opioid prescription, high-dose prescriptions, long-term prescriptions, and three or more opioid prescribers.
For opioid prescriptions per capita, the association with change in suicide deaths was significantly stronger in the West than in the East or the Midwest. For percentage with at least one opioid prescription and with three or more opioid prescribers, the associations were stronger in the West than elsewhere and stronger in the South than in the Midwest or the East (see Table S3 in the online supplement).
For males and females, change in regional suicide deaths was also positively associated with change in each opioid-prescribing measure. For the two youngest and the oldest age groups, however, change in regional suicide deaths was not significantly related to change in any of the prescribing measures. Among individuals in the 45- to 64-year age group, change in regional suicide deaths was positively associated with change in regional opioid prescriptions per capita (β=0.054, p=0.0001) and change in percentage with at least one opioid prescription (β=0.061, p=0.0004).
Suicide Deaths Involving Opioids
During the study period, the annual regional rate did not significantly change for suicide deaths involving opioids (from 0.64 to 0.66 per 100,000 persons; difference=0.02, 95% CI=−0.04, 0.08) (see Tables S1 and S2 in the
online supplement). Similar to the associations with total suicide deaths, change in regional suicide deaths involving opioids was significantly related to change in each opioid-prescribing measure in the total population and separately among males and females (
Table 1; see also Figure S5 in the
online supplement). If opioid prescribing per capita had held constant from 2009 to 2017, there would have been an estimated 10.5% more suicide deaths involving opioids in 2017. The corresponding estimated percentage increases in opioid-related suicide deaths were 14.7%, 8.6%, 8.6%, and 18.8%, respectively, for percentage with at least one opioid prescription, high-dose prescriptions, long-term prescriptions, and three or more opioid prescribers. For each prescribing metric, the association with change in suicide deaths involving opioids was significantly stronger in the West than in the South or the Midwest. For percentage with at least one prescription and percentage with three or more prescribers, the associations were stronger in the West than in the East (see Table S3 in the
online supplement).
For all except the oldest age group, change in regional suicide deaths involving opioids was significantly associated with change in percentage with high-dose opioid prescriptions. Among individuals in the 25- to 44-year age group, change in regional suicide deaths was also positively associated with change in opioid prescriptions per capita (β=0.040, p=0.004). In addition, among individuals in the 45- to 64-year age group, change in suicide deaths involving opioids was positively associated with change in long-term opioid prescriptions (β=0.051, p=0.002). For the oldest age group, change in suicide deaths involving opioids was not related to any of the opioid-prescribing measures.
Unintentional Deaths Involving Opioids
Over the study period, the annual regional rate of unintentional overdose deaths involving opioids increased from 6.56 to 15.62 per 100,000 persons (difference=9.05, 95% CI=8.18, 9.92) (see Tables S1 and S2 in the
online supplement). Change in total unintentional deaths involving opioids was positively associated with change in opioid prescriptions per capita (β=0.074, p=0.007) and change in percentage with high-dose opioid prescriptions (β=0.050, p=0.007) (
Table 2). However, neither of these correlations was significant in analyses stratified by sex. Among individuals in the 10- to 24-year and 25- to 44-year age groups, the change in unintentional deaths involving opioids was negatively associated with opioid prescriptions per capita, percentage with at least one opioid prescription, and percentage with three or more opioid prescribers. Among individuals age 65 and older, the change in regional unintentional deaths involving opioids was positively correlated with change in percentage with high-dose opioid prescriptions (β=0.086, p=0.0001).
Undetermined Deaths Involving Opioids
The annual regional rate of opioid overdose deaths of undetermined intent was little changed, from 0.73 in 2009 to 0.93 per 100,000 persons in 2017 (difference=0.20, 95% CI=−0.14, 0.54) (see Tables S1 and S2 in the
online supplement). Change in total undetermined deaths involving opioids was significantly and positively associated with change in all of the prescribing measures except percentage with at least one opioid prescription (β=0.011, p=0.57) (
Table 3). Among females, change in undetermined deaths involving opioids was positively correlated with change in opioid prescriptions per capita and percentage with long-term opioid prescriptions. For individuals age 65 and older, change in undetermined deaths involving opioids was also positively associated with change in opioid prescriptions per capita as well as with percentage with at least one opioid prescription and percentage with three or more opioid prescribers.
Discussion
In the United States, geographic regions with the greatest declines in people filling opioid prescriptions also tended to have the greatest declines in total suicide deaths, including suicide overdoses involving opioids. These associations, which were robust across all five measures of opioid prescribing and tended to be strongest in the Western United States, provide population-level evidence linking opioid prescribing to suicide risk. We estimate that, other things being equal, had the national decline in per capita opioid prescriptions between 2009 and 2017 not occurred, there would have been 3.0% more suicide deaths overall in the United States in 2017, and 10.5% more suicide deaths involving opioids. These estimates may reflect not only the high lethality of opioid overdose events (
2) but also the exceptionally high risk of suicide by all methods among individuals with opioid use disorder (
29,
30). For four of five prescribing measures, decreasing regional opioid prescriptions were also related to declining total opioid-related overdose deaths of undetermined intent. Conversely, for three opioid prescription measures, regional declines in opioid prescribing were associated with significant increases in unintentional opioid-related overdose deaths in the two youngest age groups.
Regional associations connecting decreasing opioid prescriptions to declining suicide deaths are consistent with clinical research suggesting that opioid prescriptions can contribute to suicide risk in susceptible individuals (
3). In a postmortem study, people who died of intentional overdoses were more likely than those who died of unintentional drug overdoses to have had prescriptions for opioids prior to death (
31). In addition to the direct risks related to intentional overdoses involving opioids, longer durations of opioid prescriptions have been related to increased risk of new-onset and recurrent depression (
32,
33), which may mediate increased suicide risk. Although the present population-level research cannot establish that opioid prescriptions cause deaths by suicide, the results are consistent with the view that opioid prescription policies and practices should give careful attention to possible connections between prescription opioids and suicide risk.
While the results support consideration of local opioid prescribing practices in suicide prevention initiatives, these ecological-level analyses do not shed light on the clinical pathways connecting local opioid prescribing to individual opioid overdose suicide deaths. In order to assess the effects of opioid prescriptions on an individual’s risk of suicide, it is necessary to analyze prescription records that are linked to death records at the individual level. In line with our population-level results, a patient-level case-control study of veterans with chronic non-cancer pain conditions reported that higher-dose opioid prescriptions were associated with increased suicide risk (
6). Interestingly, the strength of the association of opioid dosage with overall suicide mortality was similar to its strength with suicide overdose deaths.
In evaluating the results of this panel analysis, it is important to consider the potential for confounding factors to bias the correlation coefficients. For example, overdose deaths have been related to several population-level variables, including poverty, unemployment, lower educational attainment, income inequality, and lower social capital (
34–
36), while similar regional factors have been correlated with rates of opioid prescribing (
37,
38). However, a key advantage of fixed-effects models is that they control for all variables that vary across regions but are constant over time.
The present findings contrast with a weak relationship of local opioid prescribing and prescription opioid suicide overdose deaths previously reported from an analysis of 89 local health areas in British Columbia (
15). Because the Canadian study and the present analysis differ in analytic design, power, location, and study period, it is not possible to determine the primary reason for the divergent findings.
For four of the five prescribing measures, there was a significant positive association of opioid prescribing with unintentional overdose deaths involving opioids. Because suicide overdose deaths are particularly prone to be misclassified as undetermined deaths (
39), it is possible that the observed correlation between opioid prescribing and undetermined opioid-related overdose deaths, which was most apparent among older adults, is partially attributable to misclassified suicide deaths. This hypothesis is supported by research with electronic health records indicating similarities between suicide and undetermined overdose deaths in their pattern of mental health diagnoses, toxicological data, and recent stressors (
40,
41). In a sample of inpatients in treatment for opioid use disorder, most (58.5%) of the inpatients reported at least some desire to die before their most recent overdose, and over one-third (35.8%) expressed a strong desire to die (
42).
For the two youngest age groups, significant negative associations were identified between three regional opioid prescribing measures and unintentional opioid-related overdose deaths. In regions with falling rates of opioid prescriptions, it is possible that some individuals, including younger adults with opioid dependence, turn to heroin and other illicitly obtained or manufactured opioids that pose greater risks of unintentional overdose. For example, there were negative associations between having three or more opioid prescribers and unintentional opioid deaths in the younger age groups. Opioid prescription “doctor shopping,” which peaks around age 30 (
43), is associated with opioid dependence and low rates of treatment seeking (
44). Facing local declines in the availability of prescription opioids via multiple opioid prescribers or other sources, some individuals may initiate use of nonprescription illicit opioids.
The present analysis has several limitations. First, as an observational ecological study, this analysis cannot establish cause and effect. Because of potential confounding by time-varying factors within each commuting zone, we cannot infer that the local changes in opioid prescribing caused the coincident changes in the various mortality outcomes. Second, as stated above, it is difficult to classify overdose events according to intent, and this may be particularly true for fatal events (
40). Third, the analysis only captured changes in prescription opioids and lacked a means of measuring illicitly obtained opioids that are directly involved in a large proportion of overdose deaths (
45). Fourth, due to incomplete population coverage of the IQVIA prescription data, there is uncertainty associated with the opioid prescription measurement. Finally, because the opioid crisis has evolved from being closely tied to prescribed opioids to being related to illicit heroin and fentanyl (
46), and because the COVID-19 pandemic may have had population-level effects on suicide risk (
47), results from the 2009–2017 period may not directly apply to contemporary conditions.
Because opioids pose a greater risk than any other drug class that an intentional overdose will prove to be lethal (
2), it is not surprising that regional declines in opioid prescribing were found to ameliorate local trends in suicide deaths. These findings reinforce the importance of safe opioid prescribing practices and proper disposal of unused opioids. In managing patients with pain, physicians should evaluate whether adequate relief can be achieved with nonpharmacological interventions (
48). While some patients with pain need and benefit from opioids without risk, those for whom opioids are prescribed should be evaluated and, if necessary, treated for co-occurring mental health disorders that might otherwise increase their risk of suicide. Finally, despite the epidemiological linkage between regional decreases in opioid prescribing and lowered suicide risk, some patients who are physically dependent on opioids develop serious withdrawal symptoms that may include suicide when the opioid medications are suddenly discontinued or the dosage is quickly decreased (
49).