There are few studies of adolescent schizophrenia (
1,
2). During adolescence there are neurodevelopmental events including changes in synaptic density and morphology in the frontal lobe (
3), a decline in the ratio of gray matter to white matter (
4), marked sleep EEG changes, and a decline in cerebral metabolism (
3). These changes are believed to involve maturational reorganization consisting of selective synaptic enhancement and elimination of redundant axons (i.e., pruning). These maturational events have been summoned in support of what Keshaven et al. (
5) have described as a “late” neurodevelopmental model of the etiology of schizophrenia (
3,
6) in contrast to the “early” developmental model (
7), which posits a fixed lesion from early life that interacts with normal neurodevelopmental events occurring at a later point. A neurodevelopmental perspective suggests that substantial neurocognitive deficits should be evident very early in the course of schizophrenia.
We report the first comprehensive neuropsychological assessment of adolescent schizophrenic patients.
METHOD
Seventeen adolescent patients (12 male and five female) were included in this study. They were aged 13–18 years (mean=15.71 years, SD=1.65) and were diagnosed with schizophrenia (N=12), schizophreniform disorder (N=1), or schizoaffective disorder, mainly schizophrenic (N=4). The patients' mean age at onset of illness was 13.79 years (SD=2.42). The patients were stabilized on antipsychotic medication regimens at testing. Seventeen normal adolescent subjects (nine male and eight female) aged 13–18 years were recruited through advertisements. Their mean age was 15.12 years (SD=1.27). Written informed consent was obtained from all subjects and their parents or legal guardians.
All subjects were medically healthy. No subject had had a neurological illness or major head trauma with loss of consciousness for more than 20 minutes. The subjects did not have histories of substance abuse, as reported by the parents, and all subjects had an estimated IQ of at least 70.
Clinical diagnostic interviews were conducted by physician-investigators (S.C.S., R.L.F.). Subjects were also interviewed by a psychologist (T.P.S.) using the Schedule for Affective Disorders and Schizophrenia for School-Age Children: Epidemiologic Version (K-SADS-E) (
8). Consensus diagnoses were based on DSM-III-R criteria. Patients were studied after being clinically stabilized either early in the course of outpatient treatment or at the end of inpatient care. All of the normal subjects were also assessed with the K-SADS-E and were free of clinically significant psychopathology.
The test battery description, along with the rationale supporting the cognitive constructs purported to be measured by the individual tests, has been presented elsewhere (
9,
10). The neuropsychological tests included measures of attention (Stroop Color and Word Test [11], Digit Span Distraction [12], and Paced Auditory Serial Addition Task [13]), working memory (Trigram Recall With Interference Test [14, 15]), a measure sensitive to both attention and working memory (the coding subtest of the Wechsler Intelligence Scale for Children—Revised [WISC-R] [16]), verbal learning and memory (Selective Reminding, Categorical Clustering, and Verbal List Learning, immediate recall and delayed recall [17] and Logical Memory I and Logical Memory II, Wechsler Memory Scale—Revised [18]), generative naming (Controlled Oral Word Retrieval Test [19] and Category Instance Retrieval Test [20]), and executive functions (Wisconsin Card Sorting Test [21] and the maze subtest of the WISC-R). An estimated IQ was created on the basis of three IQ subtests (information, similarities, and block design [WISC-R]). Thus, there were 11 neuropsychological tests with 13 total measures and a single IQ estimate.
In the statistical analysis, patients and normal subjects were compared on cognitive measures by one-tailed tests, because the patients were expected to perform more poorly than the comparison group. Effect sizes were scaled as “g” (
22,
23) and indicate mean group differences in standard deviation units. To assess the number of adolescent patients with clinically significant impairment, a threshold of 2 SD from the mean of the normal subjects was used.
RESULTS
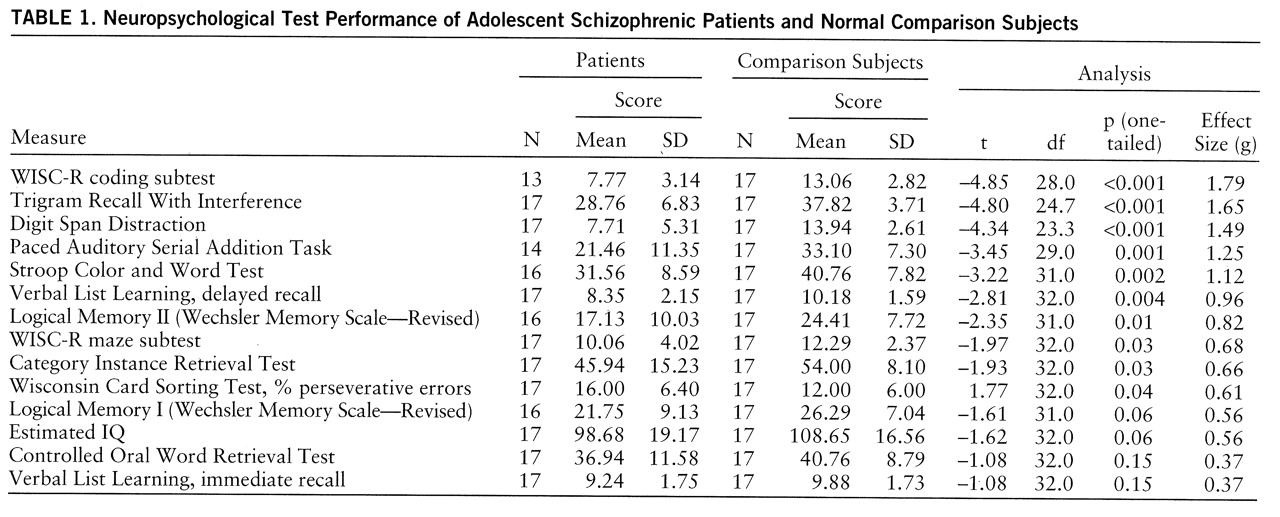
The results of the primary analysis are presented in
table 1. The measures are ordered by effect size. The patients were impaired with respect to the normal subjects (p<0.05, one-tailed) on 10 of the 13 neuropsychological measures (excluding IQ). The overall average effect size (g=0.92) was quite large (
24).
The measures showing the greatest impairment (i.e., the largest effect sizes) were those with a strong component of working memory or attention. Also, the percentage of patients who performed more than 2 SD below the mean of the normal subjects was greater for WISC-R coding (47%), Trigram Recall With Interference (65%), and Digit Span Distraction (71%) than for the measures of other functions (range=12%–35%).
DISCUSSION
The main finding was that adolescents with schizophrenia showed generalized neuropsychological impairment on measures of attention, working memory, secondary memory, generative naming, and executive functions. The effect sizes were moderate to very large (
24). To our knowledge, this study is the first to identify neuropsychological dysfunction in adolescents with schizophrenia with the use of a comprehensive test battery and with nonpsychiatric comparison subjects.
The largest effect sizes were on measures of focused and divided attention as well as working memory. Also, a large percentage of the patients performed at a clinically significant level of impairment. Taken together, these findings attest to the relatively greater role of attention and working memory deficits in adolescent schizophrenia.
The precise neurodevelopmental etiology of the impaired cognitive performance of adolescent schizophrenic patients is unclear. It is unknown whether the neurodevelopmental and disease processes are independent or, alternatively, whether the neurodevelopmental process itself is diseased.