Pathological gambling is a disabling disorder that is progressive, chronic, and associated with a 20% rate of suicide attempts (
1). Over the last decade, with increased access to legalized forms of gambling, prevalence estimates of pathological gambling have grown from 4.6% to 7.3% of the adult population (
2), yet pathological gambling remains a neglected disorder with few treatment studies.
Use of the selective serotonin reuptake inhibitor (SSRI) fluvoxamine in the treatment of pathological gambling is supported by evidence of serotonin dysfunction in pathological gambling (
3–
5), a phenomenological link to compulsivity (
6), utility of fluvoxamine in other obsessive-compulsive spectrum disorders (i.e., compulsive shopping) (
7), and a possible response in pathological gambling to the serotonin reuptake inhibitor clomipramine (
8).
METHOD
Subjects were recruited by professional referrals, media (press, radio, television) advertising, and flier postings; therefore, the findings of this study may not be applicable to a non-treatment-seeking gambling population. Forty-nine subjects were screened to enroll 16 subjects. Following a telephone screen, comorbid axis I disorders were determined by a research psychiatrist (C.M.W., S.M., or R.G.) who conducted face-to-face clinical interviews. Minimum entry criteria included a DSM-IV diagnosis of pathological gambling and a South Oaks Gambling Screen (
9) score greater than 5. Study-eligible patients also participated in a Structured Clinical Interview for DSM-III-R Personality Disorders and completed the South Oaks Gambling Screen and the Clinical Global Impression (CGI) pathological gambling scale to assess pathological gambling severity. Individuals currently abusing substances and those with past or present schizophrenia, schizoaffective disorder, organic mental syndromes, or bipolar disorder type I or type II, as well as those taking terfenadine, astenizole, or cisapride, were excluded from the study. Written informed consent was obtained from all participants after a complete description of the study. Family history data were derived from the South Oaks Gambling Screen and self-report.
Subjects entered an 8-week single-blind placebo lead-in phase to establish a stable baseline, to account for a possible early placebo response followed by relapse, and to ensure compliance. An 8-week single-blind fluvoxamine trial followed. Weekly visits occurred for the first 4 weeks of each phase and biweekly visits for the next 4 weeks of each phase. The baseline score for the fluvoxamine trial was the mean of scores for the last two visits on placebo. Ratings performed by the study psychiatrist included gambling urge and behavior scores on the pathological gambling modification of the Yale-Brown Obsessive Compulsive Scale (a modified version of the original reliable and valid Yale-Brown scale) and global gambling improvement scores on the CGI pathological gambling improvement scale. Interrater reliability, assessed by intraclass correlations, for Yale-Brown scale urge and behavior scores, respectively, were high—0.99 and 0.98 (unpublished work by C.M. DeCaria et al.). Yale-Brown scale scores correlated well with CGI scores (r=0.89, df=8, p<0.001) and had high convergent validity with South Oaks Gambling Screen scores (r=0.86, df=8, p=0.003) (unpublished work by C.M. DeCaria et al.). Friedman’s analysis of ranks was used to compare the Yale-Brown scale scores at baseline (average of last two placebo visits) and six subsequent scores during treatment with fluvoxamine.
RESULTS
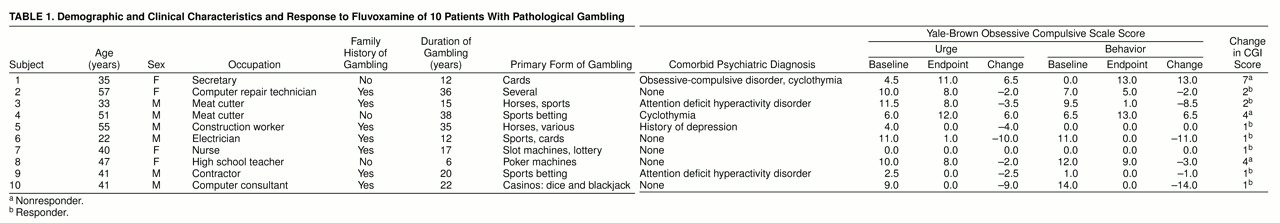
Sixteen patients entered the placebo lead-in phase. Six dropped out while receiving placebo, and 10 patients completed the 8-week trial of fluvoxamine. Completers included six men and four women; their mean age was 42.2 years (SD=10.7, range=22–57), mean duration of illness was 21.3 years (SD=11.3, range=6–38), and mean South Oaks Gambling Screen score was 15.2 (SD=3.3). Four of the 10 patients were married, three were divorced, and three were single. Comorbid diagnoses included attention deficit hyperactivity disorder (N=2), cyclothymia (N=2), obsessive-compulsive disorder (N=1), and major depressive episode (N=1). Seven patients reported a positive family history of problem gambling, although diagnoses for family members were not confirmed by direct interview. There was no apparent relationship between treatment response and family history. The mean fluvoxamine dose at study endpoint was 220 mg/day (SD=79, range=100–300, minimum=100 mg/day for 4 weeks), and treatment responders tended to have lower doses (mean=207 mg/day, SD=79) than nonresponders (mean=250 mg/day, SD=87).
Of the six dropouts, four were terminated for noncompliance after baseline ratings, and two completed 8 weeks of the placebo phase and terminated secondary to lack of improvement. The nonrandomized design contributed to an early, rapid placebo response in that the mean Yale-Brown scale urge score decreased from 11.6 (SD=4.0) to 6.5 (SD=3.6) between baseline and week 2, followed by a gradual worsening until the end of the placebo phase (mean=6.9, SD=3.9). By contrast, there was a steady drop in Yale-Brown scale urge score throughout the 8-week fluvoxamine treatment phase from 6.9 (SD=3.9) to 4.8 (SD=5.0), corresponding to a 30% overall fluvoxamine treatment response and a 64.6% improvement for the treatment responders (from mean=6.9, SD=4.6, to mean=2.4, SD=3.8). This trend was also seen in Yale-Brown scale behavior scores (the baseline mean of 13.1, SD=3.1, dropped to mean=5.4, SD=4.4, by week 2, rose to mean=6.1, SD=5.5, at the end of the placebo phase, and then decreased to mean=4.1, SD=5.5, at end of fluvoxamine treatment), for a 33% improvement on Yale-Brown scale behavior overall and an 86% improvement for the seven responders (from mean=6.1, SD=5.8, to mean=0.9, SD=1.9) while taking fluvoxamine.
Seven of 10 patients were judged treatment responders at endpoint: 1) their clinician-rated CGI scores were very much improved (score=1) or much improved (score=2) in gambling severity, and 2) they had greater than 25% decreases in Yale-Brown scale gambling behavior scores. Although five (41.7%) of 12 patients in the original group of 16 patients were rated as CGI responders during placebo, and seven (70%) of 10 patients who completed the study were rated as CGI responders, chi-square analysis did not demonstrate significance (χ2=1.766, df=1, p=0.18). Friedman’s analysis of ranks during the fluvoxamine part of the trial was significant for Yale-Brown scale urge score (χ2=14.25, df=6, p=0.03), showing that the mean baseline score of 6.9 (SD=4.0) and the mean treatment week 1 score of 5.8 (SD=4.9) were higher than the mean scores for subsequent treatment weeks (ranging from mean=5.2, SD=4.2, to mean=4.5, SD=4.4). The analysis for Yale-Brown scale gambling behavior scores was not significant.
In addition to reducing the gambling urge, fluvoxamine treatment resulted in total abstinence of gambling behavior in the seven treatment responders, according to patient report, clinician and patient ratings, and information from other informants. Patients may be abstinent but still have low positive scores on the Yale-Brown scale due to a subjective feeling of lack of complete control over the behavior. A typical responder, patient 10, went from a baseline of gambling 12 hours at a casino once a week (for an average net loss of $3,000/week) to complete abstinence at the end of treatment (
table 1).
DISCUSSION
In this preliminary study, seven of 10 patients with pathological gambling who completed a fluvoxamine trial met criteria for response, including a much improved or very much improved CGI pathological gambling improvement score and a greater than 25% reduction in the gambling behavior score on the Yale-Brown scale. All seven responders achieved gambling abstinence, and they had a mean 86% improvement in the gambling behavior score on the Yale-Brown scale. However, this study should be viewed with caution because of the non-double-blind design and the small number of subjects. The nonrandomized initial placebo lead-in resulted in a rapid reduction of symptoms over 2 weeks, followed by a gradual deterioration of symptoms over the course of the placebo phase. The placebo lead-in phase was used to exclude noncompliant patients and to establish a stable baseline. Two of the three fluvoxamine nonresponders had a history of cyclothymia, and exacerbation of their comorbid condition by fluvoxamine at a higher dose (250 mg/day) may have been associated with relapse in gambling behavior.
Few treatment outcome studies in pathological gambling have been conducted, and available treatments demonstrate little efficacy over time (i.e., only 8% of Gamblers Anonymous members are abstinent at 1-year follow-up [
10]). This preliminary study suggests that the SSRI fluvoxamine may be effective in the treatment of pathological gambling. However, given the nonrandomized nature of the trial, a randomized, controlled trial is needed to confirm efficacy, and long-term follow-up is needed to determine whether putative treatment response is maintained over time.