Medical disorders may be divided into two classes: those which represent discrete entities or continua with only a negative pole (e.g., Huntington's chorea or diabetes) and those which have both a positive and a negative pole (e.g., idiopathic mental deficiency or myopia). High intelligence and 20/15 eyesight, after all, are assets. This paper examines the possibility that there may be individuals resistant to depression at the positive pole of the affective disorder continuum.
The more that an illness results from a clear organic defect, as now seems to be the case in schizophrenia (
1), or from a single gene (e.g., Huntington's chorea), the less likely there is to be a positive pole. The more that an illness is polygenic and without a known specific structural defect (e.g., being tone deaf or having low intelligence), the more likely there is an opposite end of the continuum where we will find a Mozart or an Einstein. The fact that some forms of low intelligence or poor vision can be caused by specific genetic defects does not invalidate the coexisting concept of a continuum. Children with gene-specific Down's syndrome and phenylketonuria may also manifest a wide range of intelligence.
To test the hypothesis that vulnerability to mood disorder lies on a continuum, this paper uses data from a 55-year longitudinal study (
2,
3) originally designed to examine positive mental health. At the outset, it must be acknowledged that some forms of affective disorder (type 1 bipolar illness, for example) may be genetically distinct subtypes of DSM-IV major depressive disorder, just as Down's syndrome is a distinct subtype of mental deficiency. The existence of genetically distinct subtypes of depressive disorder, however, does not invalidate the concept of a polygenic continuum of affective/dysthymic disorder. Despite the distinctions in DSM-IV, generalized anxiety disorder, dysthymia, and bipolar illness all share a greater familial risk for major depressive disorder. This point of view is supported by genetic evidence (
4,
5), by comorbidity with other disorders (
6,
7), by longitudinal study (
8,
9), and by a common response to antidepressants (
10,
11). Such mood-disorder-vulnerable patients also manifest high affective distress (measured by neuroticism [12, 13] and SCL-90 scales).
In hopes of identifying men resistant to distress at the healthy end of an affective continuum, a subgroup of men were identified who, after 55 years of observation, appeared as different as possible from men with major depressive disorder. Three objective criteria were used to identify this subgroup of consistently undistressed men: 1) they had never used psychotropic drugs before the age of 50, 2) they had never visited a psychiatrist before the age of 50, and 3) they were classified as “emotionally stable” at the age of 21. The first two of these criteria were chosen because over the observation period of more than 50 years, men with major depressive disorder had shown themselves to have the most visits to psychiatrists and to be the highest users of psychotropic medication. Furthermore, men who were classified as emotionally stable at age 21 were less likely to have a family history of affective disorder and subsequently to experience symptoms of major depressive disorder. Alcohol abuse has different antecedents but similar consequences to major depressive disorder (
14); therefore, to avoid problems of comorbidity, men with primary alcoholism were excluded from the analyses.
METHOD
Subjects
Between 1939 and 1942, a university health service chose 268 college sophomores for intensive multidisciplinary study (
2,
3). These sophomores were selected because their physical examination at college entrance had revealed no mental or physical health problems and their deans had perceived them as having the potential to become promising adults. The students' parents were interviewed, and extensive family, social, and medical histories were obtained. Of the original study group of 268 men, only 237 are included in this report. The attrition of 31 men was due to incomplete data (N=19) or death before age 45 (N=12).
At the beginning of the study, the men were studied by internists, psychiatrists, psychologists, and anthropologists. Half of the men were on scholarship and/or had to work during college to meet expenses; 64% obtained a graduate degree. The men have been reinterviewed at approximately ages 25, 30, and 50. In adult life, most have worked as physicians, lawyers, university professors, or business executives. Since age 45 they have been followed by means of questionnaires every 2 years and physical examinations every 5 years through their 70th year. In 1996 their mean age was 75 years (SD=2).
Measures
To reduce halo effects, 10 different independent raters and/or the men themselves were responsible for the following ratings.
The mood disorder continuum. A rating of 1 on this continuum indicated that the subject was undistressed—that at age 21, the subject was classified as emotionally stable and that up to age 50 he reported no use of psychotropic medications or visits to psychiatrists or psychotherapists (N=64). A rating of 2 on this continuum indicated that the subject was intermediate—that he did not meet the definitions for depressed or undistressed (N=109). A rating of 3 indicated that the subject was depressed or vulnerable to mood disorder—that before age 50 he had a score of 2 or more on the Indicators of Major Depressive Disorder Scale (mean=5.3 indicators) (N=20). (This scale was developed specifically for this study.) Forty-four men with alcohol abuse and without unambiguous preexisting major depressive disorder (a clear bipolar diagnosis or five or more indicators of major depressive disorder) were excluded from some of the analyses. To determine the age at onset of depression and of alcohol abuse, independent psychiatrists reviewed each man's entire record (
17).
Alcohol abuse. DSM-III criteria were used to diagnose alcohol. A rating of 1 indicated no abuse; a rating of 2 indicated alcohol abuse (the subject experienced social complications of alcohol use and had difficulty controlling alcohol use or a pathological pattern of alcohol use), and a rating of 3 indicated alcohol dependence (the subject met criteria for abuse plus tolerance or withdrawal symptoms). At age 45–50, the men were interviewed by experienced clinicians regarding problem drinking. Since age 47, each biennial questionnaire has asked whether each man, his friends, his family, or his physician has worried about his drinking. Medical and psychiatric records were reviewed.
Variables Underlying the Mood Disorder Continuum
Indicators of Major Depressive Disorder Scale. This scale was designed to assess objective evidence of major depressive disorder in this community sample of men before the onset of chronic physical illness (and before modern assessment instruments were introduced). An independent psychiatrist, blinded to summary ratings, reviewed each man's complete records (from college until the men were age 50) for nine correlates of depression: 1) being seriously depressed for 2 weeks or more by self-report, 2) diagnosed as clinically depressed by a nonstudy clinician, 3) receiving antidepressant medication, 4) experiencing manic episodes, 5) sustained (>2 weeks) anergia or decreased concentration, 6) neurovegetative signs of depression, 7) attempted or completed suicide, 8) sustained anhedonia, and 9) psychiatric hospitalization (not for alcohol abuse). For the purpose of this paper, all men with two or more indicators of depression but without preexisting alcohol abuse were classified as depressed. Twenty men met these criteria; they had a mean of 5.3 indicators of depression (SD=2.5). Although in previous papers (
16,
17), depressive heredity had been included as a tenth item, in this paper depressive heredity is used as an independent variable.
Use of psychotropic drugs before age 50 (maximum yearly use). A rating of 1 on this item indicated no use of psychotropic drugs—i.e., less than 5 days per year use of sleeping pills, stimulants, tranquilizers, or antidepressants. A rating of 2 indicated 5–30 days of use per year. A rating of 3 indicated more than 30 days of use in at least 1 year. A rating of 4 indicated misuse of psychotropic medication. Scores of 3 or 4 were categorized as regular use. Use of psychotropic medications to manage medical illness was not included.
Psychiatric visits. The total numbers of visits for personal problems to psychiatrists and psychotherapists between age 20 and age 50 were summed.
Emotional stability. Between 1942 and 1944, a research psychiatrist rated the men on 25 individual traits (
18) on a present/absent basis. Rater reliability was not obtained. One of these 25 traits correlated most negatively with lifetime risk for major depressive disorder and with family history of major depressive disorder. This trait was emotinal stability—being “well-integrated” after 3 years of study during college. The trait was defined as being “steady, stable, dependable, thorough, sincere, and trustworthy.steadiness and integrity of personality.factor(s) that enable a young man to surmount common problems”
(2, p. 23).
Antecedent Variables
Ancestral longevity. The age of each grandparent at death was obtained either from the subjects' parents at the start of the study or, if the grandparents survived past 1941, from the subjects themselves. Since the men themselves now have a mean age of 75 (SD=2), 99% of their parents have died.
Family history of depression and alcoholism. When the subjects were sophomores (1940 to 1942), a social investigator visited the men's homes and took an extensive social history from their parents. This history included age and cause of death of any deceased close relative and whether any close relative suffered from mental illness, alcohol abuse, or had committed suicide. Over the next 50 years, alcohol abuse and depression among siblings were recorded. In middle life, the men were again specifically questioned about both depressed and alcoholic relatives. Raters blind to clinical outcome separately coded men for alcoholic and depressed relatives. A code of 1 indicated no afflicted relatives, a code of 2 indicated one afflicted relative, a code of 3 indicated two afflicted or one severely afflicted relative, and a code of 4 indicated multiple severely afflicted relatives.
College psychological traits. In addition to the trait of emotional stability, three of the other 25 individual traits were relevant to the analysis. Two traits correlated most positively and one trait correlated most negatively with a 1–3 scale of overall “psychological soundness” assessed at age 21. The positive traits were vital affect (“richness of affect.a spontaneous force and energy” [2, p. 24]) and friendly (“makes friends easily.unhampered by shyness or awkwardness” [2, p. 28]). The negative trait was asocial (“social life, intimate friendships, and an interest in people are relatively unimportant. Lack of feeling for human behavior” [2, p. 28]).
Bleak childhood (ages 0 to 18). Two research assistants, blinded to all data gathered after the men were 19 years old, rated five facets of the men's childhood environmental strengths (global impression, family cohesion, and relations with mother, father, and siblings) on a scale from 1 to 5. A bleak childhood was defined by a score of 0–10 (bottom third) out of a possible 25. Interrater reliability was r=0.71 (
19).
Psychosocial adjustment (ages 20 to 30). After reviewing all available data after 12 years of follow-up in 1950–1951, the original study director classified each subject on a 1–5 scale of “personality stability.” Ratings of 4 or 5 were categorized as worst personality stability at age 30.
Outcome Variables
By design, raters for each of the following variables were blind to other study ratings.
Income (ages 45 to 55). This variable was the maximum annual earned income in 1977 dollars.
Objective physical health status. Each man's physical examination (obtained every 5 years) was rated by an internist. A rating of 1 indicated excellent physical health, a rating of 2 indicated minor irreversible problems (e.g., glaucoma, gout, well-controlled hypertension), a rating of 3 indicated life-shortening irreversible illness (e.g., diabetes, myocardial infarction), a rating of 4 indicated chronic illness with substantial disability (e.g., advanced emphysema or multiple sclerosis), and a rating of 5 indicated that the subject had died. The scale is described in greater detail elsewhere (
20). Men given a rating of 1 or 2 at age 70 were classified as having good physical health.
Limitations of physical activity at age 70. Every 2 years since age 65 the men have completed a 10-question multiple-choice assessment of grades of physical limitation. Scores ranged from 10 to 23. No limitations (score of 10–12) meant that the men continued to play active sports, could climb two flights of stairs without resting, and could move furniture without limitation.
Mortality (age 75 plus or minus 2 years). Mortality was confirmed by death certificate through 1995 except for two subjects who died overseas.
Confounding (Health Risk) Variables
The following variables were included in the analysis to control for association of major depressive disorder with unhealthy habits.
Obesity. Obesity was defined in terms of body mass index (kg/m2). Men with a body mass index of 30 kg/m2 or more were classified as obese.
Cholesterol. Cholesterol levels (mg/100 ml) were assessed at ages 45–55.
Lifetime cigarette smoking. Cigarette smoking was measured in pack-years (
15).
Extensive exercise (ages 20 to 60) (N=178). Exercise that burned more than 2000 kilocalories/week was classified as extensive (
21).
Mental Health Outcome Variables
The following variables were included to show association of the criteria for being undistressed with other measures of positive mental health.
Affective spectrum disorder. After thorough review of their complete records up to age 50, 23 men were diagnosed as having probable “affective spectrum disorder” by an independent study clinician. Nineteen men were classified as having probable major depressive disorder and four as having severe anxiety disorder with affective symptoms (
16).
Neuroticism. Neuroticism was measured at a mean age of 68 (SD=1) by using the Neuroticism-Extroversion-Openness Personality Inventory of Costa and McCrae (
22). Their neuroticism scale correlates at r=0.75 with the neuroticism scale of the Eysenck Personality Inventory (
12,
13).
Depression. Depression was measured by using a subscale of the Neuroticism-Extroversion-Openness Personality Inventory that “measures the tendency of normal persons to experience depressive affect.scores on this scale are the best single predictor of overall happiness or unhappiness” (
22).
Marital stability (ages 20 to 70). Marital stability was measured on the basis of five multiple-choice questionnaires of marital satisfaction from the husbands and three from the wives over a 40-year period. A man was classified as having achieved a long stable marriage if a first marriage had lasted for 30 years or a second marriage had lasted for 20 years and both partners agreed that it was without serious sustained conflicts or actual separation (
23).
Statistical Methods
Kaplan-Meier curves were used to estimate rates of health decline. The curves were compared by using the Wilcoxon-Gehan log rank test (
24). The characteristics and health outcomes for each of the four groups of men (undistressed, intermediate, depressed, alcoholic) were compared by using chi-square. Analysis of variance was used for continuous variables, and results are presented as means and standard deviations. Spearman rank-order correlation was used as a test of association. Because many of the significant findings supported each other in consistent directions, a full Bonferroni correction for multiple comparisons seemed too conservative. Instead, the paper comments on results significant at p≤0.01 (two-tailed).
RESULTS
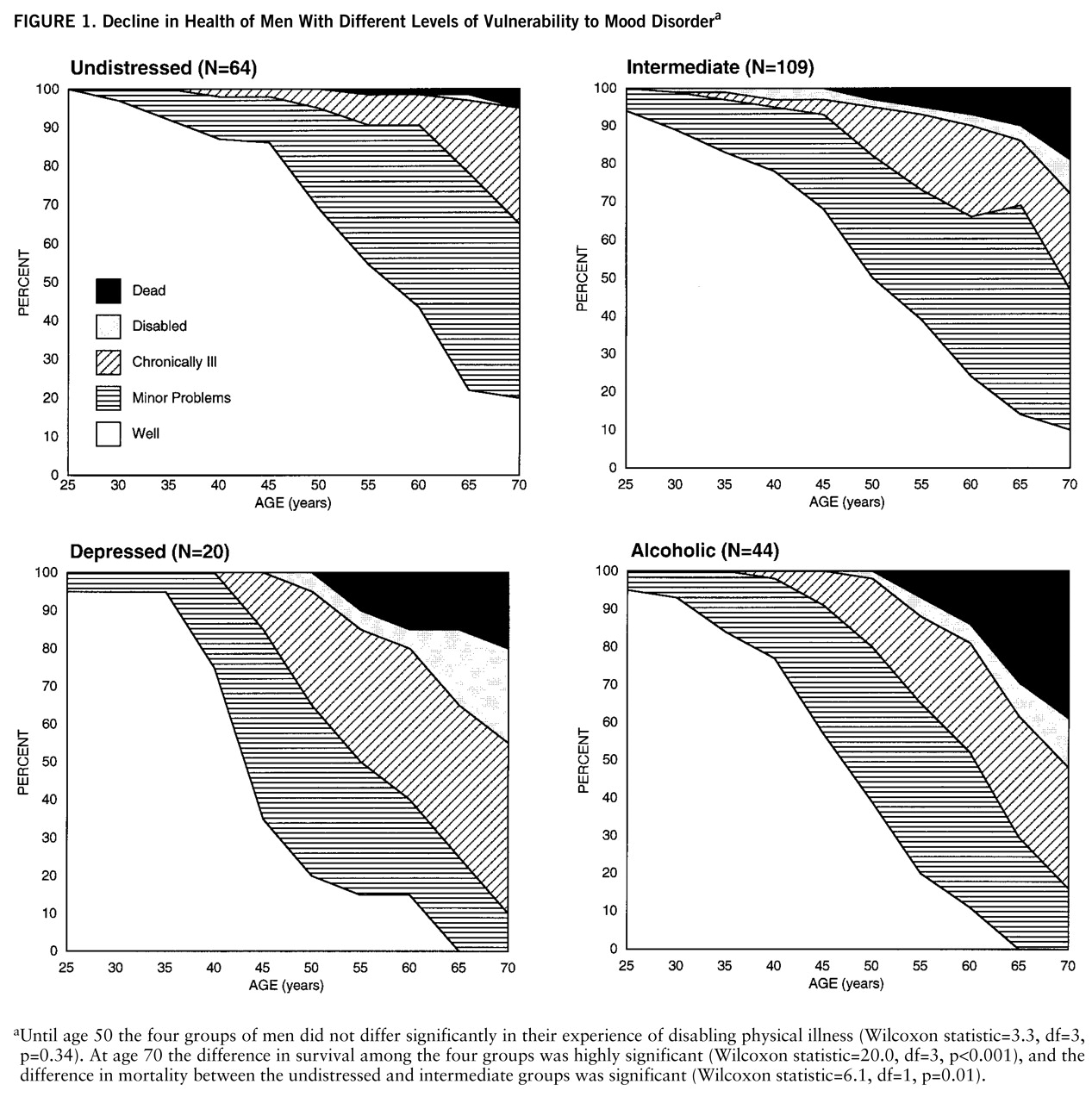
Figure 1 shows the decline in health of the 64 undistressed men, the 20 depressed men, the 109 men in the intermediate group, and the 44 men with alcohol abuse.
For the undistressed men, physical disability between ages 50 and 70 continued to be minimal. In contrast, the depressed and alcohol-abusing groups have spent 50% of those two decades chronically ill, disabled, or dead. However, in only two cases had the evidence of clinical depression occurred after development of chronic physical illness. At age 50, 97 of the 135 men who eventually became ill were still in good health. Survival curve analysis revealed that the differences between the rate of onset of disabling chronic irreversible disease between the 64 undistressed men and the 109 men in the intermediate group was highly significant (Wilcoxon statistic=12.1, df=1, p<0.001).
Only seven (3%) of the 237 men developed diabetes. Heavy smoking, hypertension, and obesity were also relatively rare (work in preparation). Thus, the 19% death rate (N=45) for the whole study group by age 70 was only half the death rate for U.S. white males born in 1920 (
25). The death rate for the undistressed men, however, was only one-eighth of that expected for white males their age.
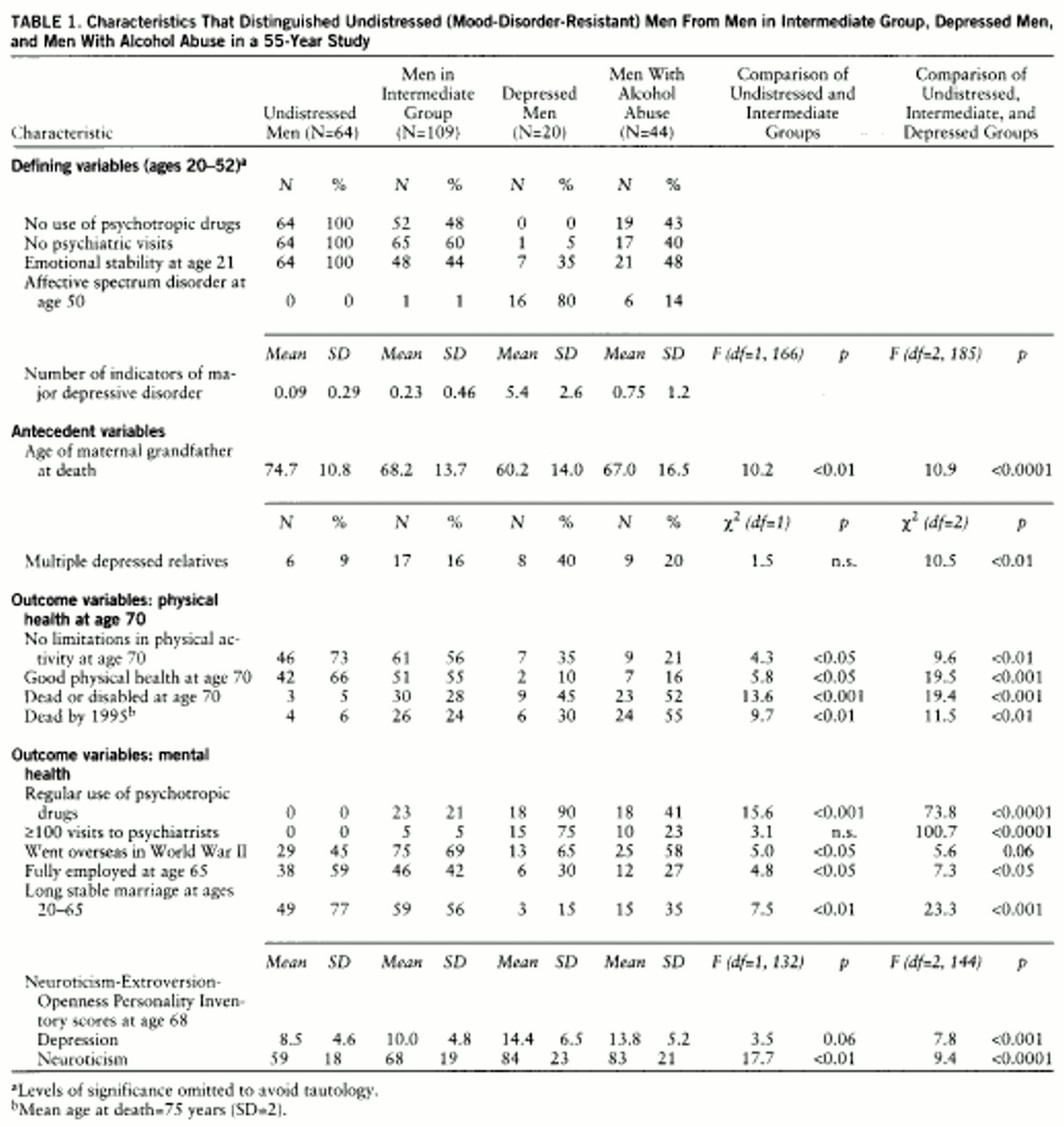
Table 1 presents evidence that the arbitrary categorization of men into the undistressed, intermediate, depressed, and alcohol abuser categories had good face validity. Although there were inevitable overlaps (due to comorbidity) among the three groups (i.e., one man in the intermediate group and six men who had alcohol abuse were clinically categorized as manifesting “affective spectrum disorder,” and six depressed men met criteria for alcohol abuse), the groups represent three clearly different clinical clusters. The men categorized as depressed experienced several times as many indicators for major depressive disorder as any other group.
Table 1 presents the antecedent variables and the psychological variables that distinguished the undistressed from the intermediate group and that supported the existence of a mood-disorder-resistant pole. In terms of neuroticism and physical health, the undistressed were significantly different from the intermediate group. In terms of their different patterns of staying “Stateside” during World War II, sustained working after age 65, and stable marriage, the lives of the undistressed men reflected the same wish not to change that was reflected by their not using mood-altering agents.
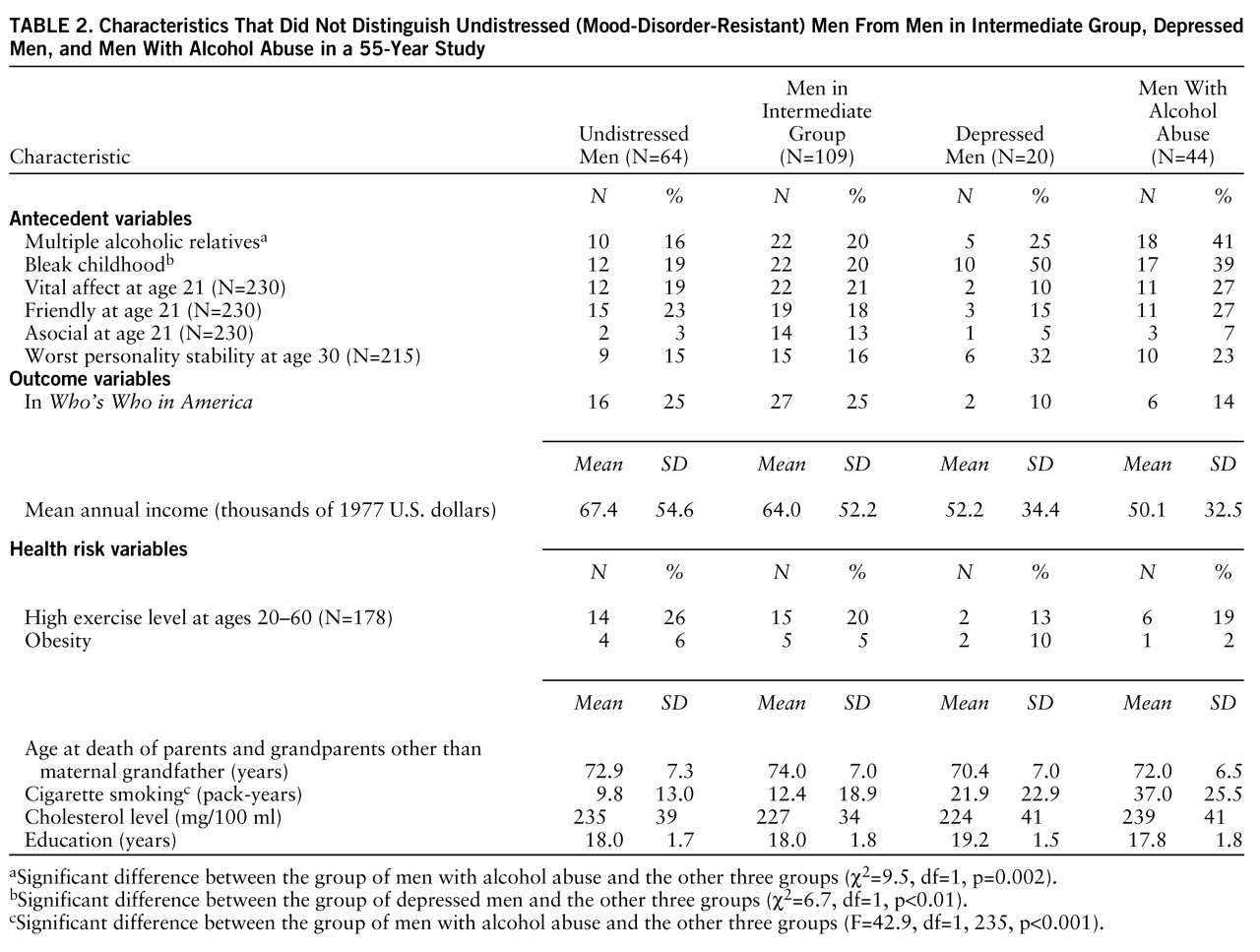
Table 2 helps to distinguish the theoretical continuum of vulnerability to affective distress from a continuum of mental health per se. The variables associated most positively (vital affect and friendly) and most negatively (asocial) with good college mental health (
2) did not distinguish the undistressed men from those in the intermediate group or from the depressed or alcoholic men. Although both personality instability at age 30 and occupational failure were correlated with personality disorder (
26) and with poor global mental health at age 65, these variables did not distinguish the undistressed men from those who were depressed or those in the intermediate group. Men with alcohol abuse, although excluded from calculations of statistical significance, are included for comparison.
Table 2 also makes it clear that the lower rate of physical morbidity that distinguished the undistressed group from the intermediate group could not be easily attributed to an absence of common biological risk variables. None of the men in both the undistressed and intermediate groups abused alcohol, and these two groups had similar rates of exercise, obesity, and heavy smoking. Excluding the age of their maternal grandfathers at death, the undistressed men were as likely to have short-lived and alcoholic relatives as the men in the intermediate group.
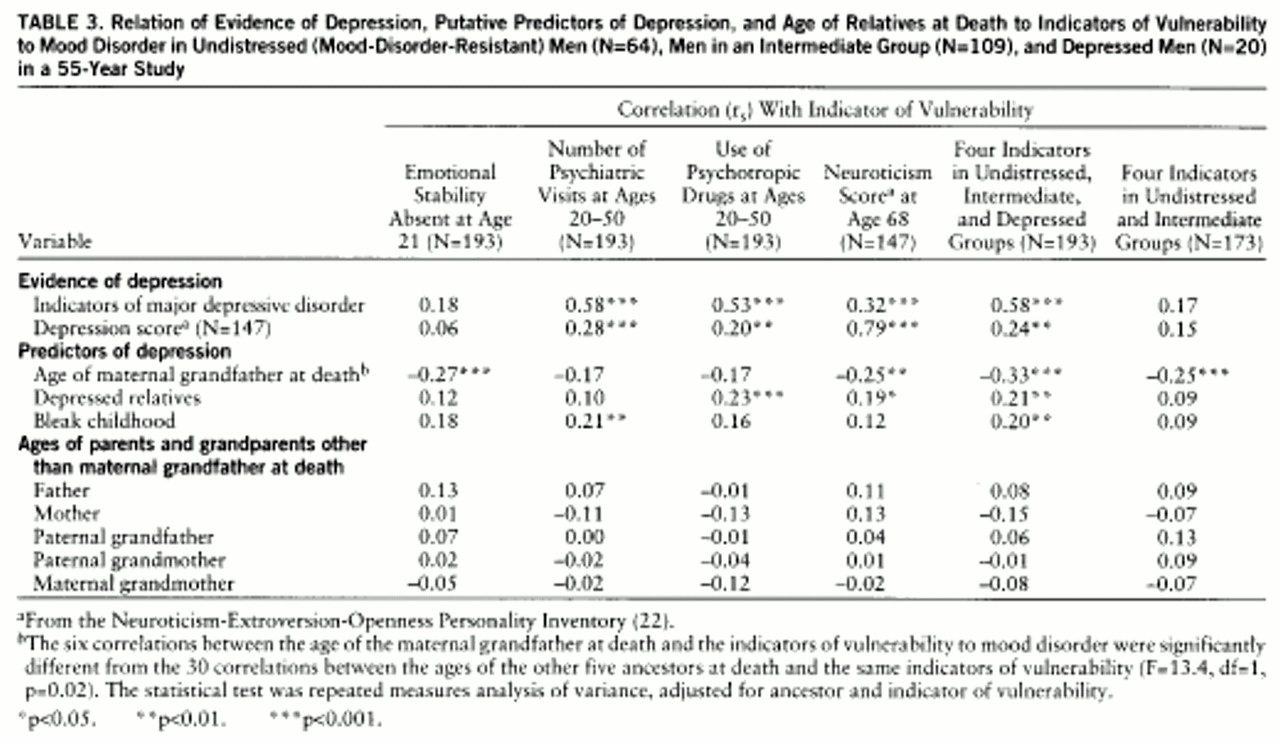
Table 3 illustrates the strong association of clinical evidence for major depressive disorder with the three indirect measures of distress and with neuroticism. Significant predictors of the distress continuum included both genetics (family history of depression and age of maternal grandfather at death) and childhood environment. The association between childhood environment and the distinction between the undistressed and intermediate groups was not significant. There was no consistent trend of association between the longevity of the subject's parents and the three grandparents other than the maternal grandfather and evidence of mood disorder.
DISCUSSION
The hypothesis that mood disorders lie on a continuum is venerable but debatable (
7,
27). First proposed by Mapother, then by Sir Aubrey Lewis (
28) more than a half century ago, and more recently supported by Andrews et al. (
29) and Hudson and Pope (
6), the hypothesis suggests that many anxiety disorders and most depressive disorders lie along a single biological continuum. The data in this paper suggest that such a psychobiological continuum may extend to include a distress-resistant positive pole. At one extreme are those individuals identified by low levels of neuroticism, long-lived maternal grandfathers, and a life-long pattern of not attempting to change state or mood (through the adventure of war, mood-altering drugs, alcohol, or divorce). At the other end of the continuum are individuals defined as vulnerable to mood disorders by a wide variety of indicators, including both family history of depression and short-lived maternal grandfathers.
The concept of a continuum was supported by the striking absence of death and disability among the men classified as undistressed (
Figure 1 and
table 1) as well as the greater morbidity (strongly associated with poor self-care—cigarette smoking, alcohol abuse, suicide, accidents, etc.) (
16) among the depressed men. The fact that longevity of the maternal grandfather very significantly differentiated the undistressed, intermediate, and depressed groups of men (
table 1) lends support to the hypothesis that resistance to mood disorders might have a biological as well as a behavioral basis. Long-lived maternal grandfathers not only predicted being categorized as undistressed (
table 1) but also predicted being in the lowest quartile (score <55) on the neuroticism scale (F=8.1, df=1, p=0.005). Short-lived maternal grandfathers were more common not only among the depressed men (
table 1) but also in the clinically convergent groups of men who reported receiving antidepressant medication (N=18, mean age of maternal grandfather at death=62.1, SD=13.2) (F=7.1, df=1, p<0.01) and men clinically classified as having affective spectrum disorder (
16) (N=23, mean age of maternal grandfather at death=60.1, SD=13.7) (F=10.81, df=1, p<0.001). Age at death of maternal grandfather of men without major depressive disorder but with alcohol abuse (
table 1) or personality disorder (
17) did not differ from that of the intermediate group. Such findings are consistent with the evidence of
table 2 that the proposed continuum is one of vulnerability or resistance to mood disorder and not of mental health per se. It is of interest, however, that the maternal grandfather's age at death was uncorrelated with a family history of affective disorder (r
s=–0.02). In other words, the maternal grandfather's age at death and the number of depressed relatives appeared to be independent risk factors.
The findings of this 55-year study must be interpreted with extreme caution. First, the number of subjects is small and the subjects are socially advantaged men from a single birth cohort. Second, the association of early death of maternal grandfather with affective illness is puzzling and requires confirmation. Even if confirmed, such an association by no means demonstrates causality. Unfortunately, information regarding premature cause of death of maternal grandfather was inadequate (
17).
The indirect diagnosis of major depressive disorder (necessitated by a study of a nonclinical sample observed before 1970) is also a serious limitation. To overcome this limitation, convergent data were obtained from multiple independent sources: 1) the men's biennial questionnaires, 2) utilization of mood-altering drugs and visits to psychiatrists, 3) family history of depression, 4) review of entire record for objective indicators of depression by an independent psychiatrist (
17), and 5) the Neuroticism-Extroversion-Openness Personality Inventory. However, such methods do not differentiate major depressive disorder from dysthymia or even from adjustment disorder with depressed mood. As the almost threefold discrepancy in lifetime prevalence of major depressive disorder between the Epidemiologic Catchment Area study (
30) and the National Comorbidity Survey (
31) suggests, any categorization of lifetime risk of depression disorder is still imperfect.
Absence of distress (stable personality in college and no efforts to seek psychological help or change mental state with medication over a 30-year period) reflects an equally indirect category. Absence of distress cannot be distinguished with certainty from sustained stoicism. For example, when the undistressed men were contrasted with the men in the intermediate group, not only were the former somewhat less likely to report physiological symptoms under stress (rs=0.20, p=0.03) and experience fewer psychosomatic illnesses (rs=0.19, p=0.03), they were also somewhat more likely in college to have been called inarticulate (rs=0.20, p<0.01) and at midlife noted to use the defense of suppression (rs=0.17, p=0.05).
Arguably, these limitations are balanced by the unique advantages of studying a relatively homogeneous cohort of men selected for health rather than illness, with multiple baseline measures, and with prospective ascertainment of ancestral death, alcohol abuse, and affective illness. Most important, the prospective study design ruled out the possibility that preexisting physical illness (figure 1) preceded the men's visits to psychiatrists and use of mood-altering drugs before age 50.
To clarify why the mood-disorder-resistant men (the undistressed) had less physical disability than the men in the intermediate group requires further study. Previous investigation of this study group suggests that the intervening mechanism linking low levels of psychological distress to good physical health did not appear to be simply fewer obvious biological risk factors (
table 2), absence of stressful life events (
32), high social class and education (work in preparation), absence of World War II combat-induced symptoms (
33), or resistance to cancer (
16). The better physical health of the undistressed men may be due to their not seeking change in mood or state—whether that be through divorce or seeking combat, through psychotherapy or early retirement, or through tranquilizers and alcohol. Just as mood disorder leads people to seek multiple other means of altering one's state, lifelong resistance to mood disorder, almost by definition, may be reflected by a lifestyle embracing self-care and many healthy—even stodgy—habits.