Differences between black and white Americans in access to and utilization of health care services have become a focus of growing attention and concern in recent years (
1). Studies have shown that blacks are significantly less likely than whites to receive advanced medical treatment (
2,
3), including coronary angiography and bypass surgery (
4), hemodialysis and kidney transplants (
5), surgical treatments for cerebrovascular disease (
6), and specialized treatments for AIDS (
7). Analysis of data from the Medicare program also suggests that blacks receive lower-quality health care than do whites (
8).
Several groups of investigators have used administrative databases to document racial differences in the delivery of mental health services (
9–
11). However, these studies did not address differences in the personal experiences of patients from different ethnocultural groups in the same program. A survey of literature published before 1988 showed racial differences in participation in, and benefit from, psychotherapy in only a small number of studies (
12). A more recent series of studies of specialized Department of Veterans Affairs (VA) mental health programs also showed few differences between black and white veterans in health care service utilization and in outcomes (
13–
17). However, one study that focused on the interpersonal context of treatment showed that the pairing of black patients with white clinicians was associated with early dropping out of treatment and receipt of less intensive services (
18). Identification of racial differences in the experience of mental health treatment may thus require attention to personalized features of the treatment experience.
Few studies have offered explanations for racial differences in health service use beyond general references to the history of racial bias in American society. If adequate adjustment is made for differences in health status and in help-seeking behavior (
6), there are three plausible explanations for the observed differences in health service use by black and white Americans. First, persistent institutional biases, embedded in the culture and power arrangements of U.S. health care organizations, may create a hostile treatment environment for minorities. Second, negative attitudes toward blacks among white health professionals, administrators, staff, and patients may discourage minority participation in treatment. Finally, distrust and alienation among black patients as a result of past negative experiences in both the health care system and other social institutions in American society may impair the sense of trust that is an important part of any therapeutic relationship. In the mental health field, in particular, racial distrust may generate differences in treatment participation and outcomes. These features are especially likely to be prominent when treatment is delivered in an intensive interpersonal milieu, such as an inpatient psychiatric ward or long-term residential treatment program. We are aware of no studies, however, that have compared the participation and outcome of racial groups in such programs.
In the current study we examined the subjective, as well as objective, experiences of black and white veterans in an intensive psychosocial residential rehabilitation and work therapy program in operation at several VA facilities. In this study we compared baseline characteristics, objective and subjective indicators of program involvement, and 3-month postdischarge outcomes of black and white veterans who participated in a multisite residential work therapy program for veterans with severe substance abuse.
We addressed three questions: 1) Are there differences between black and white veterans in subjective experiences and objective measures of program participation, when differences in baseline status are controlled for? 2) Are there important differences between black and white veterans in clinical improvement 3 months after treatment? and 3) Are subjective and objective measures of program participation and clinical improvement influenced by the racial composition of the program, i.e., do the treatment experiences of African American veterans differ between programs in which they constitute a high proportion of participants and programs in which they constitute a minority?
METHOD
Compensated Work Therapy/Transitional Residence Program
The VA Compensated Work Therapy/Transitional Residence Program is a rehabilitative bridge that puts a strong emphasis on community living and workplace collaboration. The program provides three key services: 1) residential treatment, provided in community settings, where veterans live together and share responsibility for paying their rent and maintaining their residence, 2) a required therapeutic work-for-pay program that provides supported work placements that encourage and reinforce adaptive work behaviors, and 3) substance abuse outpatient treatment provided at the residence, at VA outpatient clinics, and through linkage with Alcohol Anonymous (AA) or Narcotics Anonymous (NA) (
19).
The program is based on the premises that patients with severe substance abuse disorders will benefit from extended residential treatment, peer involvement, and professional support and that such treatment should require responsible community-oriented behavior, such as working at a job and paying rent, in addition to staying sober and participating in treatment. The veterans are required to work in the work therapy program and to deduct a portion of their earnings as rent. The work therapy program is a therapeutic work-for-pay program in which private sector businesses or federal agencies contract with VA for work to be performed by veterans (
20).
Study Group
From October 1990 to September 1995, 628 black veterans and 688 white veterans each completed an episode of treatment at 15 sites across the country. Veterans who were of Hispanic, American Indian, Alaskan, or Asian ethnicity were excluded from these analyses. The study sample included 962 veterans (73.1% of the total) who were interviewed at baseline and were successfully reinterviewed 3 months after discharge. There was no significant difference between the percent of white veterans reinterviewed after discharge (71.5%, N=492) and the percent of black veterans reinterviewed (74.8%, N=470) (χ2=1.97, df=1, p=0.16).
Comparison of the black veterans who were not reinterviewed after discharge and those who were revealed no significant difference on any sociodemographic or baseline clinical measure. The white veterans who were not reinterviewed 3 months after discharge were significantly different from those who were reinterviewed on only two baseline measures; they had higher scores on the global severity index of the Brief Symptom Inventory (
21) (t=–2.1, df=684, p=0.03), and a larger proportion reported alcohol use in the last 30 days that they lived in the community (79.1% versus 71.1%) (χ
2=4.5, df=1, p=0.03).
Data Collection
The data were collected by research assistants who received face-to-face training in interview procedures at the beginning of the study and ongoing supervision. At the time of each veteran's admission to the program the research assistant 1) explained the study procedures and obtained written informed consent and 2) conducted an extensive baseline assessment interview addressing demographic characteristics; health status, including substance use; and social adjustment.
One month after admission, the veterans completed two questionnaires that assessed their subjective perception of the therapeutic environments in the residence and in the work therapy component of the program. Research assistants completed structured summaries documenting delivery of all program services. At the time of discharge, data on length of stay and discharge status were recorded on a structured discharge form completed by program clinicians. Follow-up interviews were conducted 3 months after discharge (mean=121 days, SD=50 days).
Outcome Measures
Clinical psychiatric diagnoses, obtained at admission, were based on assessments by clinicians using DSM-III-R criteria. Alcohol, drug, and psychiatric problems were assessed by using composite indices from the Addiction Severity Index (
22), and psychological distress was assessed with the global severity index of the Brief Symptom Inventory (
21). The reliability and validity of the core instruments used in this study (the Addiction Severity Index and Brief Symptom Inventory) have been established previously (
21–
23).
Current employment was determined by a single question that asked the number of days each veteran had worked in competitive employment in the past 30 days.
Program Participation Measures
Subjective experience measures. The 40-item version of the Community-Oriented Programs Environment Scale (
24) was used to characterize the veterans' perception of the residential treatment environment 1 month after admission to the program. Interrelationships between the 10 subscales were examined, and mean scores on nine of the 10 subscales were combined to form a modified score for the Community-Oriented Programs Environment Scale (Cronbach's alpha=0.80). The subscale for anger and aggression was not included in the index and was addressed separately.
The Work Environment Scale (
25), a social environment instrument similar to the Community-Oriented Programs Environment Scale, was used to assess the veterans' experience of the therapeutic work-for-pay component of the program 1 month after program admission. Mean scores on nine of the 10 subscales were combined to form an overall work environment score (Cronbach's alpha=0.85). The work pressure subscale was only weakly interrelated with the other nine subscales, and so it was not included in the index and was addressed separately.
Objective measures. Clinical summaries yielded data on 1) average number of hours worked per week, 2) employment earnings per month (through both the work therapy program and supplemental competitive community employment), 3) average rent paid per month for support of the residence, 4) average number of toxicology screens performed per month, and 5) average number of AA/NA meetings attended per month. Upon discharge, clinicians documented each veteran's length of stay and mode of program discharge.
Proportion of Blacks at Each Site
On the basis of data on veteran ethnicity collected at baseline, the 15 participating program sites were ranked as to the proportion of black Americans in each program. The sites were then categorized into tertiles according to program racial composition, generating three levels: high, moderate, and low. The sites categorized as “high” were the five sites with the largest proportions of black veterans (>50%), those rated “low” were the five sites with the lowest proportions of blacks (<30%), and the remaining five sites, the “moderate” group, were the sites where the proportions of black veterans were between 30% and 50%.
Analyses
First, the significance of differences between blacks and whites on baseline characteristics was determined. Second, analysis of covariance (ANCOVA) and logistic regression were used to evaluate differences between black and white veterans on subjective and objective measures of program participation and postdischarge outcomes. Statistical adjustment was made for measures that were different between blacks and whites. In the analyses of differences between black and white veterans on postdischarge outcomes, the baseline value of the outcome measure was also included as a covariate. In a final series of analyses, factorial ANCOVAs were performed to examine the effect of the interaction between race and program racial composition on measures of program participation and outcome.
RESULTS
Comparison of Black and White Veterans
Of the 962 veterans for whom complete baseline, program participation, and follow-up data were obtained, 48.9% (N=470) were African American.
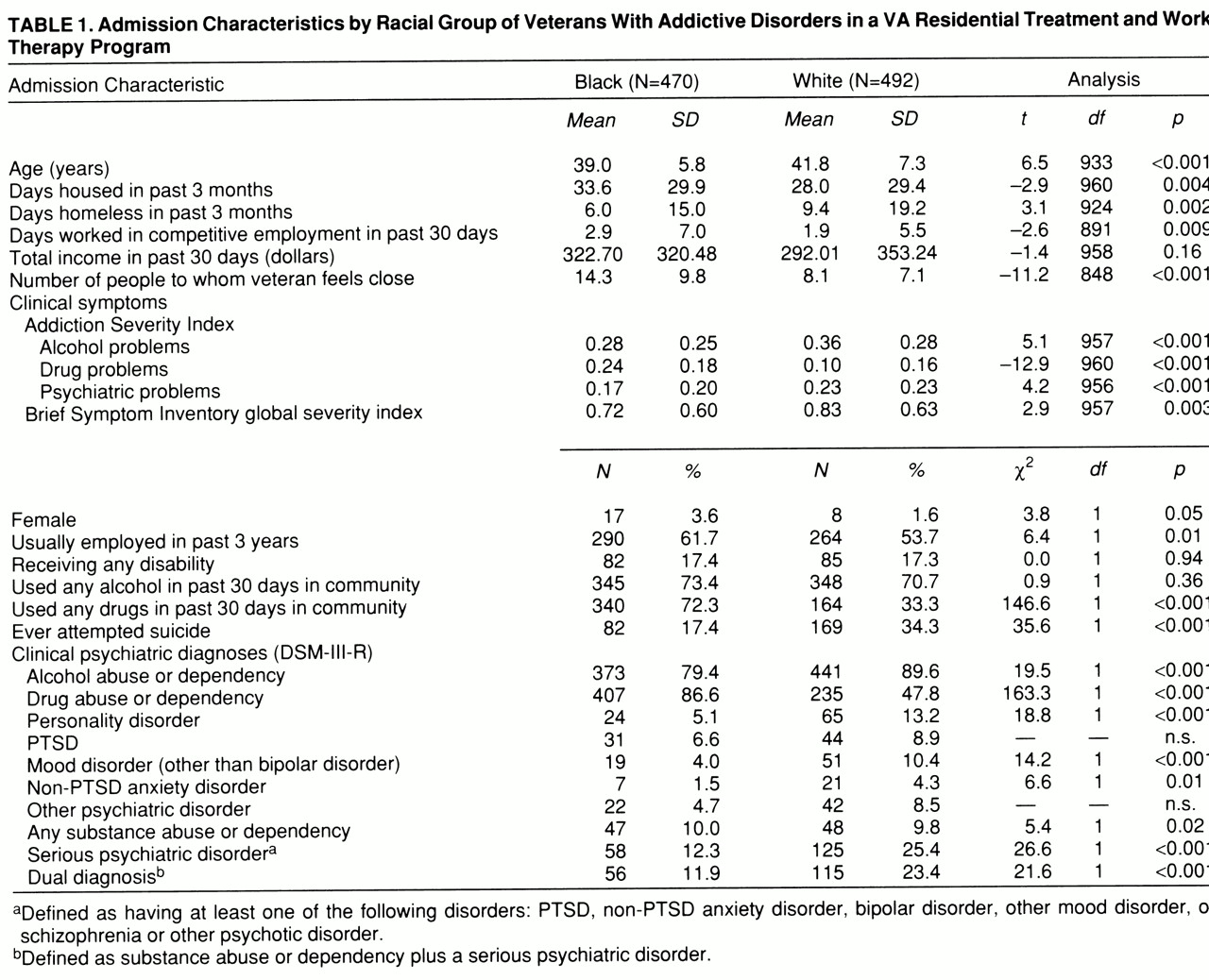
Baseline characteristics. Table 1 shows that the black and white veterans differed significantly on a number of baseline measures. The blacks were younger than the whites, spent more days housed during the 3 months before admission, and had better employment histories before entering the program. The black veterans had significantly higher scores on the Addiction Severity Index drug index and were more likely to have used drugs during the last 30 days they had lived in the community. Blacks had significantly lower Addiction Severity Index composite scores for alcohol and psychiatric problems, lower scores on the global severity index of the Brief Symptom Inventory, and were less likely to have ever attempted suicide in their lifetimes. Social network size, the number of people the subject reported feeling close to, was larger for blacks than for whites.
Black veterans were more likely to have had a diagnosis of drug abuse or dependency, while significantly more white veterans had diagnoses of alcohol abuse or dependency, had serious psychiatric illnesses (e.g., mood, anxiety, bipolar, and psychotic disorders), or were dually diagnosed with a substance abuse problem and serious psychiatric illness (
table 1).
Program participation. Overall, when baseline characteristics were controlled for, there were few differences between blacks and whites on measures of program participation with the exception of two measures. Compared to the white veterans, black veterans perceived the milieu of the residential treatment component of the program to be more positive, as measured by the Community-Oriented Programs Environment Scale index, and on average they worked more hours per month in the work therapy component of the program (
table 2).
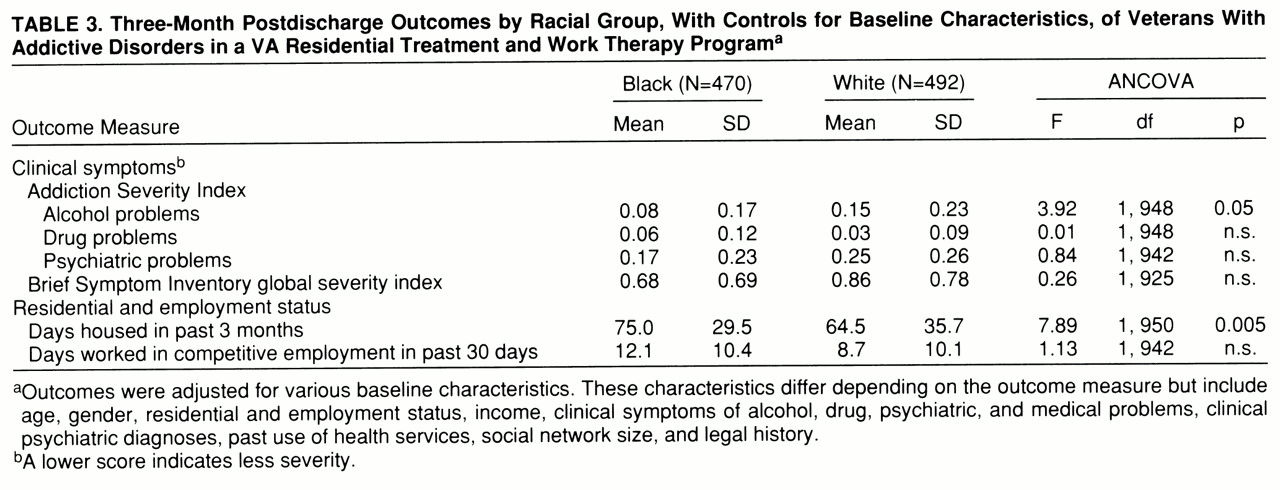
Outcomes. The percentage of black veterans who were sober at 3 months was 66.2% (N=311), and the percentage for whites was 58.5% (N=288) (logistic regression Wald χ²=13.87, df=1, p<0.001).
Table 3 contains the results of ANCOVAs on the six other outcome measures, with baseline status controlled for. Compared to white veterans, black veterans had more improvement on three of the seven outcomes: rate of sobriety, score for alcohol problems on the Addiction Severity Index, and days of housing in the previous 3 months.
Patient Race and Program Racial Composition
Of the 439 veterans in the racial composition group classified as having a high percentage of blacks, 300 (68.3%) were African American; the number of African American in the “moderate” racial composition group was 99 (41.3%) of 240, and the number of African American veterans in the “low” racial composition group was 71 (25.1%) of 283.
Program participation. Multivariate analysis showed no significant interactions between the patient's race and the racial composition of the program for any of the 13 program participation measures. Blacks thus had no more positive experiences of the program when there was a high proportion of blacks in the program than when there was a low proportion of blacks.
Outcomes. There was only one outcome measure, sobriety for the previous 3 months, for which there appeared to be a significant interaction between patient race and program racial composition (Wald χ²=7.05, p=0.008), although this significance was lost when the Bonferroni correction was used to adjust for the fact that seven outcome measures were tested. The data thus no more than suggest that black veterans are more likely to remain sober at program sites with a high proportion of blacks and white veterans are more likely to remain sober at programs with a low proportion of blacks.
DISCUSSION
The findings of this study are generally consistent with results from other studies that have examined the experience of black and white veterans in specialized VA mental health programs (
13–
17). As in studies of homeless veterans and veterans with posttraumatic stress disorder, the blacks were younger than the whites and had more severe drug abuse problems, less severe alcohol and psychiatric problems, and more extensive social support networks. This study was distinctive in that it included detailed data on both objective and subjective indicators of treatment experiences. Contrary to our expectations, there were no differences between blacks and whites on 11 of 13 measures of program participation, and blacks felt more positively about the therapeutic milieu than whites and worked more hours per month in the work therapy program (after statistical adjustment for baseline differences in sociodemographic and clinical characteristics). Black veterans also showed more improvement than whites in alcohol use and housing.
In contrast to previous findings that the pairing of black patients with white clinicians was associated with early dropping out of treatment and receipt of significantly less intensive services (
18), the proportion of black participants at the site level had no impact on measures of program participation or outcome among black participants with one exception: blacks were more likely to achieve 3-month sobriety when treated at programs with higher proportions of black participants. This is an isolated finding but one that suggests the possibility of some clinical advantage for minorities in more racially balanced programs.
This study differs from others (
18,
26) in emphasizing the racial composition of the peer group rather than client-clinician matching. In milieu programs such as this one, which are based on the premise that the “community” is the central therapeutic agent, we feel that it is the racial composition of the program participants, rather than clinician-client matching at the level of the individual clinician, that is most salient. It is notable, however, that the proportion of black clinicians in this program was also generally greatest at the sites that treated larger proportions of black patients, reflecting local demographic trends.
This study thus suggests that it is important to distinguish studies that examine differences between racial groups in the types of programs they use (inpatient versus outpatient; crisis treatment versus psychotherapy) from studies that focus on differences in their personal experience of programs in which they are active participants. Studies reviewed here, and others of which we are aware, suggest that differences between racial groups are more important in program selection or accessibility than in personal experience as a participant. Participant experiences are likely to have been more different for blacks and whites in the past and may have improved with the changes in race relations in the United States in recent decades. Current efforts to enhance the equity of delivery of mental health services may be better focused at the level of the organization of service delivery systems than at the level of individual clinicians.
Several methodological limitations require acknowledgment. First, veterans are a distinct subgroup of the U.S. population, including few women, and VA is unusual in that it is a national, government-operated system. As a result, we can not assume that VA results are generalizable to other health care systems. In fact, as a free health care system operated by the federal government for specially entitled citizens, VA may engender less racial mistrust than do other institutions (
15). Additional studies such as this one are needed to clarify these issues in other health care systems.
Second, selection bias poses a potential threat to the validity of any nonexperimental study. Although we statistically controlled for all baseline variables that significantly differed between racial groups, the possibility remains that other, unmeasured factors may explain our findings. It seems unlikely, however, that such factors would so dramatically reverse our results that blacks would have lower levels of program participation and poorer outcomes than whites.
Third, although the reliability and validity of the instruments used in this study have been demonstrated in previous studies, reliability testing was not conducted and self-report data were not independently validated.
On the basis of the detailed data on program participation and outcome from this large group of participants in an intensive residential program, we found no evidence that black veterans experience less program participation or worse outcome. These results, while consistent with others from studies that addressed participation in specific treatment programs, stand in notable contrast to findings of substantial differences in the types of programs used by blacks and whites.