The diagnosis of acute stress disorder was introduced in DSM-IV. Like posttraumatic stress disorder (PTSD), acute stress disorder is defined in DSM-IV as a disorder that follows experiencing, witnessing, or being confronted with events involving actual or threatened death, physical injury, or other threats to the physical integrity of the self or others. In addition, to meet the definition of an appropriate stressor (criterion A), the person’s response has to involve intense fear, helplessness, or horror. Whereas PTSD reflects disturbance that has lasted for more than 1 month, acute stress disorder must last for a minimum of 2 days and can only be diagnosed up to 1 month after the stressor. Acute stress disorder also differs from PTSD in being explicitly formulated as a dissociative response to trauma. Thus, a diagnosis of acute stress disorder requires at least three dissociative symptoms (criterion B) but only one symptom from each of the reexperiencing (criterion C), avoidance (criterion D), and arousal (criterion E) categories. Impairment (criterion F) is also necessary and is formulated somewhat differently from that specified for PTSD. At this early stage in the formulation of acute stress disorder, little empirical evidence is available for the specific assumptions incorporated in DSM-IV.
For example, consistent with other theoretical statements
(1), DSM-IV proposes that acute stress disorder represents a recognizable conjunction of symptoms and that it constitutes a risk factor for the development of PTSD. Although there is evidence that dissociative symptoms are sometimes predictive of later PTSD
(2,
3), Dancu et al.
(4) reported that this predictive relationship held true for victims of physical assault but not for rape victims. In three studies investigators have attempted to assign diagnoses of acute stress disorder retrospectively, using various methods to assess the dissociative symptoms and without detailed consideration of whether the participants met criteria A (stressor) and F (impairment). A probable diagnosis of acute stress disorder was shown to be a predictor of later PTSD in typhoon survivors
(5) and in a small group of disaster workers (unpublished 1997 paper by T.A. Grieger et al.), but a small-scale study of road accident victims
(6) failed to find any relation between acute stress disorder and subsequent PTSD. Little is yet known about whether some dissociative symptoms are more pathological, and hence are better predictors, than others.
Previous research has indicated that reexperiencing and avoidance symptoms may also be predictive of later clinical outcomes
(7–
10). Although some investigators
(3,
5) have reported that dissociative symptoms were superior to other types of symptoms in predicting later PTSD, no studies have yet provided empirical support for the central role of dissociative responses in acute stress disorder by examining the comparative predictive power of different clusters of acute stress disorder symptoms. Similarly, Bryant and Harvey
(11) have noted that there is as yet little empirical justification for the number and severity of dissociative, reexperiencing, avoidance, and arousal symptoms specified by DSM-IV as being required for this diagnosis.
In the current study, victims of violent crime were interviewed within 1 month of the crime and completed questionnaires to assess the presence of the individual symptoms of acute stress disorder and of an overall acute stress disorder diagnosis. They were reinterviewed at 6 and 11 months to assess PTSD, but because of the low numbers of individuals with PTSD at 11 months, this paper focuses on the 6-month diagnoses. The outcome measure was a DSM-III-R diagnosis of PTSD. This was necessary because, according to new and more restrictive criteria introduced in DSM-IV, a diagnosis of PTSD now depends on the same definition of a criterion A event (i.e., subjective experience of intense fear, helplessness, or horror) that is involved in acute stress disorder. Use of the new criterion A might therefore exclude some individuals previously diagnosable according to the DSM-III-R criteria for PTSD, and none of these individuals would qualify for a diagnosis of acute stress disorder either. The effect of the overlapping criterion is that it would no longer be possible to diagnose PTSD fully independently of acute stress disorder. This reduction in the independence of the two diagnostic categories might lead to an overestimation of the association between acute stress disorder and PTSD.
METHOD
Participants
To qualify, victims of a violent crime (actual or attempted physical or sexual assault, or bag snatch) had to be 18 years old or older and to have been assaulted by someone who was not a member of the same household. Local police and medical services assisted in identifying potential participants, who were each sent a letter asking the recipient to contact the research team if he or she would be willing to take part in a study of attitudes toward crime and punishment. Initial interviews were then scheduled, all of which had to be conducted within 1 month of the crime (mean=21 days postcrime). The study had also been designed to evaluate the impact of early intervention on the development of traumatic symptoms following the crime, and the participants were randomly assigned to three different types of interview, involving education about trauma, psychological debriefing plus education, or assessment only. Subsequent analysis showed that interview type was unrelated to clinical outcome either at baseline or at 6-month follow-up (unpublished 1998 paper by S. Rose et al.), and the three groups have therefore been combined in the following analyses. A total of 2,161 letters of invitation were sent, to which 243 responses (11%) were received. After ineligible participants were screened out, 157 interviews were achieved, and 88% of those interviewed persons were successfully followed up at 6 months. Although the low initial response rate meant that it was not possible to generate meaningful prevalence estimates for acute stress disorder from this study, there was no reason to believe that the response rate would jeopardize the associations between acute stress disorder and PTSD that are the focus of this report.
The 118 men and 39 women who participated in the initial interviews had an average age of 35 years (SD=13, range=18–76). The gender distribution was typical of people reporting violent crime (other than domestic assault) in England and Wales, but the age distribution was somewhat skewed toward older respondents, probably because of our specified minimum age of 18 years
(12). Forty-five percent were married or cohabiting, 38% were single, and 18% were separated, divorced, or widowed. Level of education was used as a proxy measure of social class: 45% of the group had ended full-time education by the age of 16, 26% had high school or further education not to degree level, and 28% were educated to degree level or equivalent. Place of birth was the United Kingdom for 86% of the group, and 89% described their cultural background as European.
Overwhelmingly, the group had experienced actual physical assault (95% of men, 90% of women). Other types of violent crime included threatened physical assault (5% of men, 3% of women), sexual assault (0% of men, 15% of women), threatened sexual assault (0% of men, 3% of women), and bag snatch (0% of men, 5% of women). The bag snatches and the majority of the assaults were perpetrated by strangers (73% for men, 70% for women). The assaults had occurred in a variety of locations, including own residence (13%), the workplace (11%), bars and nightclubs (18%), and other public places (53%), and they involved multiple assailants in 48% of the incidents. Ten percent of the study group had no injuries, 8% had minor weals or abrasions, 49% had cuts or severe bruising, and 33% had more severe injuries, such as broken bones. Property was taken in 18% of the incidents, and theft was attempted in a further 7% of incidents. After complete description of the study to the subjects, written informed consent was obtained.
Measures
PTSD.
This was assessed by using the self-report version of the Posttraumatic Stress Disorder Symptom Scale (PTSD Symptom Scale)
(13). Seventeen items corresponding to DSM-III-R symptoms (four reexperiencing symptoms, seven avoidance/numbing symptoms, and six arousal symptoms) are rated on 4-point scales. The PTSD Symptom Scale has been shown to have good internal and test-retest reliability and good concurrent validity. Diagnoses of PTSD based on the scale (when any symptom with a score of at least 1 is counted as present) agree with diagnoses based on the Structured Clinical Interview for DSM-III-R (SCID) in 86% of cases
(13). In the current study this method of scoring led to some participants’ receiving PTSD diagnoses even though no symptom was rated more than 1 and the total PTSD Symptom Scale score was as low as 9 (actual range=9–43, possible range=0–51). In order to eliminate low scorers andto conform more exactly to the DSM-III-R requirement that the symptoms be persistent, scale items were therefore counted toward a PTSD diagnosis only if they were scored 2 or more. This yielded a range of 17–43 on the PTSD Symptom Scale among participants with PTSD diagnoses. The mean total score among men with PTSD diagnoses was 29.6, and among women with PTSD diagnoses it was 33.0. By comparison, in a study of women who had been assaulted and had PTSD diagnoses
(14), the mean PTSD Symptom Scale score was 35.2.
Acute stress disorder.
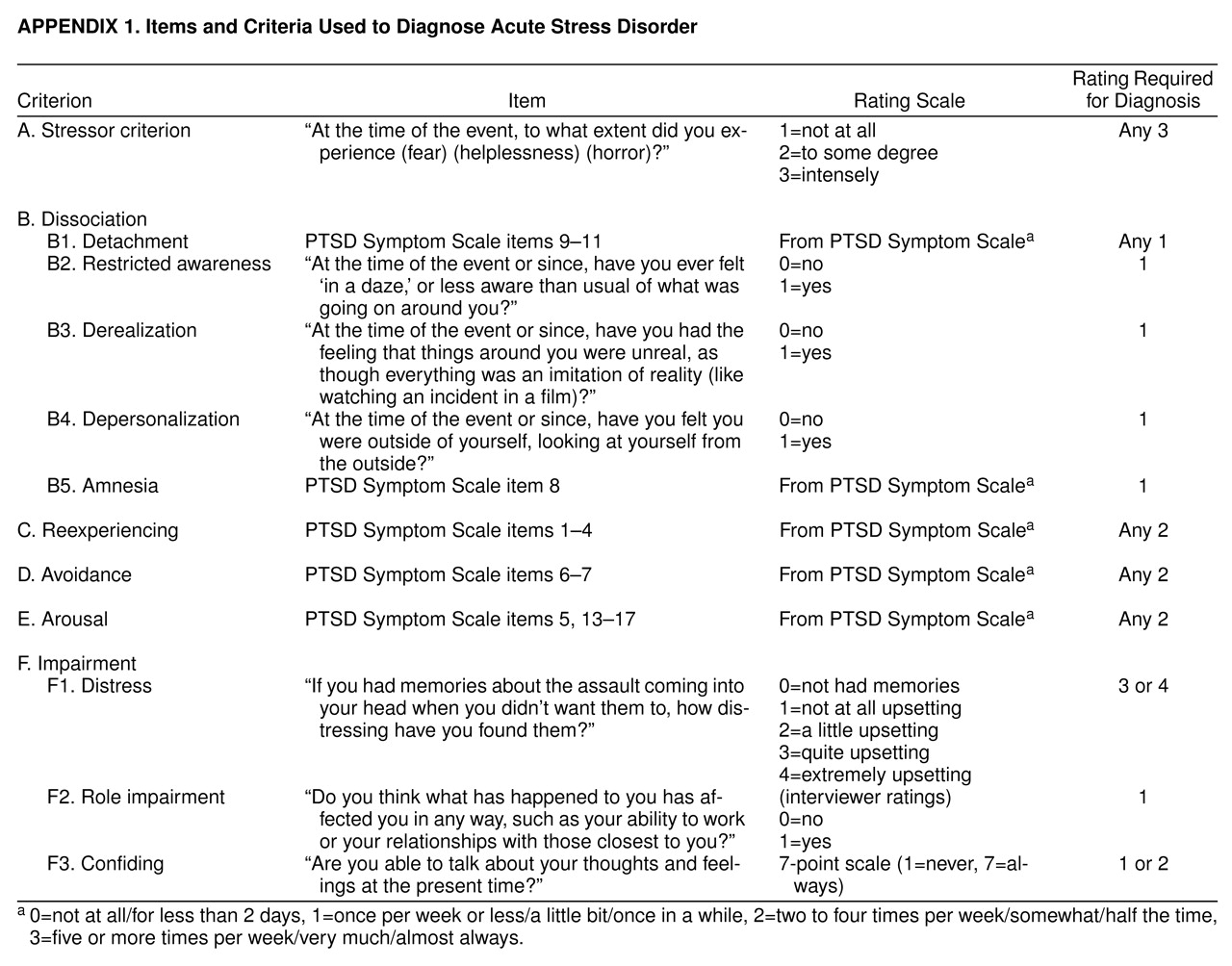
At the outset of the study there were no published interview or questionnaire measures for assessing the new diagnostic category of acute stress disorder. Our assessment of acute stress disorder therefore involved using items from the PTSD Symptom Scale where possible to assess reexperiencing, avoidance/numbing, and arousal, supplemented with additional items when required. Details of the PTSD Symptom Scale items and new questions, along with the appropriate rating scale and score required for a diagnosis of acute stress disorder, are shown in APPENDIX 1.
In keeping with the requirement of DSM-IV, the participants had to acknowledge intense fear, helplessness, or horror to meet the stressor criterion (A), and this was assessed with three new items. Criterion B (dissociation) requires the presence of at least three dissociative symptoms but does not require any particular level of intensity or persistence. Where PTSD Symptom Scale items were used, a rating of 1 (once per week or less/a little bit/once in a while) or above was therefore sufficient to qualify. Three new items required participants simply to indicate the presence or absence of restriction of awareness, derealization, and depersonalization. Because we were concerned that these concepts might be unfamiliar and difficult to understand for some participants, these new items were also administered orally to a subset of 21 participants. There was good agreement between the two formats (kappa=0.60–0.81, p<0.01).
In contrast to criterion B, which does not require a particular level of intensity or persistence, criteria C (reexperiencing), D (avoidance), and E (arousal) require at least one persistent or marked symptom, and therefore a rating of 2 (two to four times per week/somewhat/half the time) or above on the relevant PTSD Symptom Scale items was required to qualify for inclusion in the criteria for a diagnosis.
Criterion F (impairment) requires that the disturbance cause clinically significant distress or role impairment or that it impairs some necessary task, such as the mobilization of social support through confiding about the trauma. Distress was assessed with a new item on which participants rated the distress associated with their memories on a 4-point scale of severity, the top 2 points of which qualified for a rating of impairment. Because of vagueness in the DSM-IV definition of role impairment, this was assessed by having the interviewers rate responses to a new item. Responses indicating a substantial adverse effect on work, deterioration in relationships, or interference with social activities were taken as evidence of impairment, unless this was clearly stated to be due to the physical injuries sustained and not to the psychological impact of the crime. Confiding was assessed with an item from the Quality of Crisis Support scale
(15).
All participants received a set of dichotomous ratings indicating whether they had met the criteria for each of the individual symptom clusters (A–F) contributing to a diagnosis of acute stress disorder and whether they had met the criteria for an overall diagnosis.
Impact of Event Scale.
The Impact of Event Scale
(16) is a 15-item scale of current subjective distress related to a specific incident. It is widely used in research on PTSD and contains two subscales measuring intrusion and avoidance symptoms.
RESULTS
Symptoms of Acute Stress Disorder
Thirty participants (19%) were found to meet the criteria for a DSM-IV diagnosis of acute stress disorder at the baseline assessment. Acute stress disorder showed a nonsignificant trend toward being more frequent among women than among men (31% versus 15%) (χ2=3.62, df=1, p<0.06). The percentages of participants meeting the criteria in each of the various symptom clusters ranged from 46% to 65%. The contingency coefficients representing the associations between the presence/absence of individual symptom clusters and between these clusters and the full diagnosis ranged from 0.23 to 0.47 (all significant at p<0.005). Coefficient alpha, an index of the internal reliability of the items making up the diagnosis, was 0.82, indicating that acute stress disorder represents a coherent group of symptom clusters.
Concurrent Validity of Acute Stress Disorder Diagnosis
Respondents with and without a diagnosis of acute stress disorder were compared in terms of scores on the Impact of Event Scale and on the 17-item PTSD Symptom Scale. Respondents with the diagnosis had significantly higher mean scores than respondents without the diagnosis on both the Impact of Event Scale (48.9, SD=12.0, versus 21.2, SD=15.5) (t=9.14, df=155, p<0.001) and the PTSD Symptom Scale (34.1, SD=8.8, versus 11.3, SD=9.6) (t=11.86, df=155, p<0.001). The correlation between meeting/not meeting criterion C (reexperiencing) and the intrusion subscale of the Impact of Event Scale was r=0.79 (df=156), and the correlation between meeting/not meeting criterion D (avoidance) and the avoidance subscale of the Impact of Event Scale was r=0.67 (df=156).
Prediction of PTSD
Overall, 28 of the 138 reinterviewed participants (20%) met the criteria for a DSM-III-R diagnosis of PTSD at 6 months. Women were significantly more likely than men to have PTSD (38% versus 14%) (χ
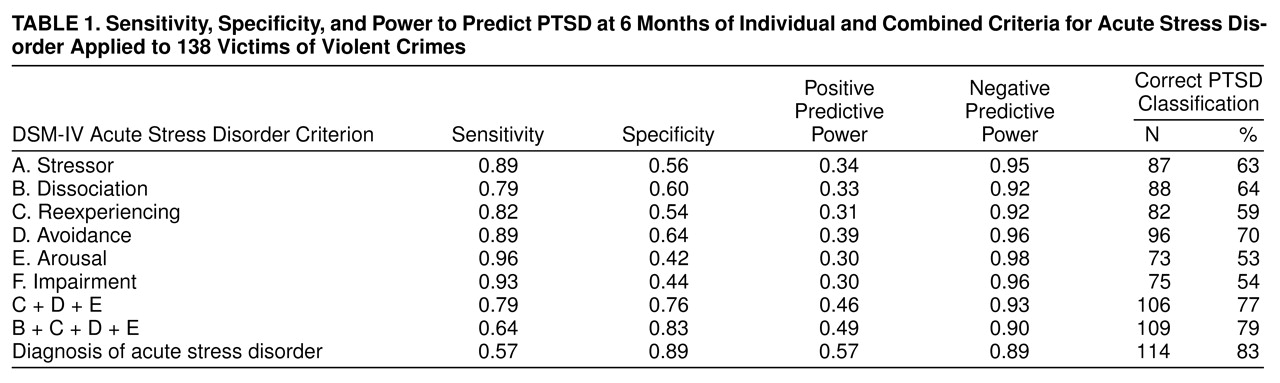
2=7.57, df=1, p<0.01). The extent to which the symptom clusters, alone and in combination, and the full diagnosis of acute stress disorder were associated with the development of PTSD at 6 months is reported in
table 1. All individual symptom clusters were significantly associated with later PTSD (smallest χ
2=13.3, df=1, p<0.001).
Table 1 shows the sensitivity of each cluster, i.e., the probability that someone with a PTSD diagnosis will have earlier reported that symptom cluster, and its specificity, i.e., the probability that someone without a later PTSD diagnosis will not have reported that symptom cluster. Table 1 also shows the positive predictive power of each cluster, i.e., the probability that someone with that symptom cluster will later report a diagnosis of PTSD, and its negative predictive power, i.e., the probability that someone without that symptom cluster will not subsequently receive a PTSD diagnosis. The overall percentage of cases correctly classified is also shown.
From
table 1 it is evident that the individual symptom clusters are approximately equivalent in having high sensitivity and negative predictive power. In other words, almost everyone with a PTSD diagnosis will have reported these symptom clusters earlier, and the absence of these symptom clusters implies a low risk of later PTSD. On the other hand, they show relatively lower specificity and ability to positively predict later PTSD. Avoidance leads to more accurate classification than any other cluster. Table 1 also shows the combined predictive power of the reexperiencing, avoidance, and arousal clusters (criteria C, D, and E) and the effect of adding the dissociative cluster (criterion B). It can be seen that the three criteria combined yield more accurate classification and better positive predictive power than any one criterion alone, but the added effect of the dissociative cluster is small. When logistic regression was used to predict PTSD status at 6 months, the improvement to the model produced by adding criterion B to criteria C, D, and E was not significant (χ
2=1.29, df=1, p>0.10).
The full diagnosis of acute stress disorder produces much better classification than any individual symptom cluster, and it is much better able to positively predict later PTSD. When logistic regression was used to predict PTSD status at 6 months, the improvement to the model produced by adding criteria A, B, and F to criteria C, D, and E was significant (χ2=10.88, df=1, p<0.02). With all of the criteria for acute stress disorder simultaneously entered in the model, the only predictors to account for significant unique variance in PTSD at 6 months were criterion A (stressor) (Wald=6.13, df=1, p<0.02) and criterion D (avoidance) (Wald=6.50, df=1, p<0.02).
Individual Dissociative Symptoms and Prediction of PTSD
All associations between individual dissociation items and later PTSD were significant, with chi-square values (df=1) ranging from 4.92 (p<0.05) to 24.16 (p<0.001), with the exception of the depersonalization item (χ2=2.67, df=1, p>0.10). With all dissociation items simultaneously entered in a logistic regression, the only predictors to account for significant unique variance in PTSD at 6 months were loss of interest (Wald=6.25, df=1, p<0.02) and emotional numbness (Wald=7.77, df=1, p<0.006).
Varying Acute Stress Disorder Criteria and Prediction of PTSD
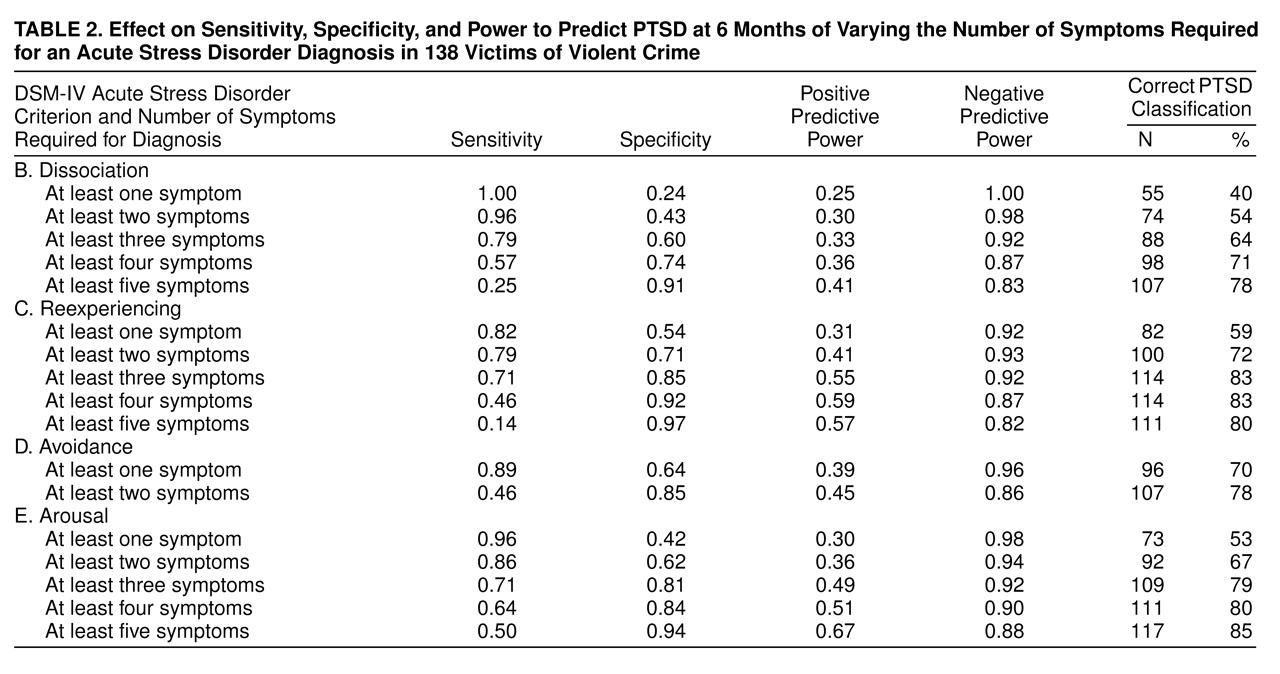
table 2 shows the effect on the prediction of PTSD of varying the number of symptoms required for an acute stress disorder diagnosis in each of the major clusters. All associations were significant at the p<0.001 level (smallest χ
2=10.83, df=1), except for thresholds of one or more dissociative symptoms (χ
2=8.54, df=1, p<0.01), four or more dissociative symptoms (χ
2=10.32, df=1, p<0.01), five or more dissociative symptoms (χ
2=5.23, df=1, p<0.05), and five or more reexperiencing symptoms (χ
2=6.19, df=1, p<0.05).
Table 2 shows that the criteria of three or more dissociative symptoms and one or more avoidance symptoms specified in DSM-IV produce a realistic balance of sensitivity, specificity, and positive and negative predictive power. While different thresholds might lead to better predictive power, for example, there are obvious costs in terms of a loss of sensitivity.
From table 2, however, it appears that more accurate classification could be obtained by adopting a threshold of three or more reexperiencing and arousal symptoms. In both cases this would bring about a substantial increase in positive predictive power, while still leaving an adequate level of sensitivity. Both these thresholds lead to levels of classification that are virtually identical to that obtained with a full diagnosis of acute stress disorder (table 1). This raises the question of whether an acute stress disorder diagnosis would add any further predictive power to the use of these new thresholds on their own. Using logistic regression to predict PTSD status, we therefore tested the effect of adding an acute stress disorder diagnosis to these revised criteria. The diagnosis resulted in significant increments both to the threshold of three reexperiencing symptoms (χ2=4.14, df=1, p<0.05) and to the threshold of three arousal symptoms (χ2=6.42, df=1, p<0.02). Changing the criteria for acute stress disorder to incorporate a threshold of three reexperiencing symptoms or three arousal symptoms did not, however, improve the overall classification rate previously achieved by an acute stress disorder diagnosis (83%) by more than an additional 1%.
DISCUSSION
To our knowledge, this is the largest prospective study of trauma victims to examine the relationship between acute stress disorder and PTSD, and the results add to findings from recent prospective studies of motor vehicle accident victims
(17) and bystanders to violence
(18). In our study group, the proportion of respondents meeting the criteria for acute stress disorder within 1 month of the assault was similar to the proportion meeting the DSM-III-R criteria for PTSD at 6 months. Respondents with acute stress disorder had scores on the Impact of Event Scale and PTSD Symptom Scale that are equivalent to those found in subjects diagnosed as having PTSD. The major findings were consistent with DSM-IV proposals in that symptoms of acute stress disorder were highly interrelated (making acute stress disorder an internally coherent construct), the numbers of symptoms necessary to meet the different criteria appeared appropriate, and acute stress disorder was strongly predictive of PTSD. Moreover, acute stress disorder was a better predictor than its constituent symptom clusters.
All of the clusters of individual symptoms of acute stress disorder were predictive of later PTSD, but there was no evidence that dissociation was a better predictor than other clusters. Previous studies have shown that later PTSD is somewhat more strongly related to dissociation symptoms than to other symptoms
(3,
5,
17,
18), but those studies did not generally investigate whether dissociation accounts for unique variance in later PTSD. One difference among studies lies in the measures of dissociation they have employed. For example, some studies focused on dissociation at the time of the event (peritraumatic dissociation), whereas others, such as ours, included dissociation both at the time of the event and afterward. Findings may well be affected by these temporal variables. As discussed by several authors
(11,
19), individual posttraumatic symptoms, including dissociative symptoms, appear to be common during or following a highly stressful event and are not necessarily pathological. In this group no one dissociation symptom stood out as being uniquely related to outcome, although loss of interest and emotional numbness appeared to be the strongest predictors. Numbing symptoms were also found to be a strong predictor by Staab et al.
(5) and Harvey and Bryant
(17), and Foa et al.
(20) found that numbing symptoms were particularly important in distinguishing assault victims with PTSD from those without PTSD.
In general, the greater the number of symptoms posttrauma, the better the prediction of later PTSD. In each symptom cluster, more symptoms led to greater positive predictive power and a higher rate of correct classification. However, if too high a threshold is set, the number of people exceeding the threshold becomes small and the index has low sensitivity. Optimum prediction of later PTSD appeared to be achieved by three or more persistent or marked reexperiencing or arousal symptoms. This finding is consistent with results of previous research on the ability of intrusive symptoms to predict outcome
(7–
10). It appears that a simple count of reexperiencing or arousal symptoms may be a highly efficient method of predicting later PTSD in victims of violent crime, a method that is as efficient as computing a full diagnosis of acute stress disorder. We are currently developing a brief screening instrument based on this finding.
Of considerable theoretical interest, however, is the fact that both acute stress disorder and high levels of reexperiencing/arousal symptoms made independent contributions to predicting later PTSD. One explanation is that the reexperiencing and arousal symptom thresholds suggested in DSM-IV for acute stress disorder are too low. But increasing these thresholds to three reexperiencing or arousal symptoms did not result in an improved classification rate. This suggests an alternative explanation, namely, that there may be two independent factors increasing the risk of PTSD, one captured by the acute stress disorder diagnosis and one captured by high levels of reexperiencing or arousal symptoms. This possibility requires investigation in future research.
The most important limitations of this preliminary study were 1) the absence of a measure of acute stress disorder with established reliability and validity and 2) the possibility that biases were introduced by the low numbers of participants responding to the letter of invitation. It is therefore reassuring that the prevalence of acute stress disorder was approximately equal to the rate of PTSD and that the symptom levels in the group diagnosed as having acute stress disorder, as indexed by the Impact of Event Scale and PTSD Symptom Scale, were comparable to those in previous groups of subjects with PTSD. In addition, the rate of PTSD among female participants in this group (38%) was similar to the rates in other studies of female victims of physical assault
(21), and the severity of PTSD was equivalent according to ratings with the PTSD Symptom Scale. Another limitation was the small number of avoidance symptoms measured, which may have limited the predictive power of this symptom cluster. Recently, the 30-item Stanford Acute Stress Reaction Questionnaire
(22) has been developed as a measure of acute stress disorder. This has a broader coverage of dissociative and avoidance symptoms, and it permits a quantitative assessment of acute stress disorder symptoms. However, it does not require respondents to specifically endorse intense feelings of fear, helplessness, or horror concerning the event, as specified in DSM-IV, and does not cover all aspects of impairment mentioned by DSM-IV.
Despite these caveats, our data are among the first to provide clear support for the specific complex of acute stress disorder symptoms proposed in DSM-IV and for the proposed symptom thresholds. Whereas we confirmed the predictive utility of acute stress disorder, we also showed that a simple threshold of three reexperiencing or arousal symptoms made an equal and independent contribution to predicting later PTSD. We also failed to find a unique role for dissociative symptoms. It should be noted that these conclusions are based on multiple analyses of the data and are therefore in need of replication and that they may not be generalizable to study groups with other types of stressors and different prevalences of acute stress disorder and PTSD.