Despite the emphasis placed on physical deficits during the early stages of recovery from a severe brain injury, it is cognitive and behavioral deficits that give rise to the major morbidity which most impairs the capacity to return to work and maintain social activities
(1). Although neurobehavioral consequences of a traumatic brain injury, such as mood swings, apathy, irritability, aggression, poor concentration and memory, and difficulty in planning, have been studied extensively in the past, the extent and the type of psychiatric syndromes per se have rarely been studied
(2,
3). Previous studies of psychiatric illness among patients with traumatic brain injury either had a small study group or failed to use validated, standardized, internationally accepted diagnostic tools
(4). In the past, subjects were recruited either from a clinic-based sample or from patients with severe traumatic brain injury who were admitted to a neurosurgical unit or a specialist neurorehabilitation unit. We thus decided to study the rate of psychiatric illnesses in a population-based sample of patients with traumatic brain injuries of all degrees of severity by means of a two-stage diagnostic procedure with the help of standardized, internationally accepted diagnostic methods.
METHOD
During a 1-year period, 3,667 adults over 17 years of age who had a diagnosis of a head injury attended the Accident and Emergency Department of the Cardiff Royal Infirmary in Wales. Of these, 14% (N=515) were admitted to a hospital; this excluded patients who had injuries only to their facial, nasal, and orbital bones. Of those who were admitted to a hospital, 86% (N=442) had an address within the South Glamorgan Health District in Wales. With the use of ICD-9 codes, a list of all of the South Glamorgan patients who were admitted to a hospital between July 1, 1994, and June 30, 1995, with a diagnosis of a traumatic brain injury (N=346) was obtained from the Health Authority’s central database. According to the case notes, 196 patients had a period of lost consciousness, radiological evidence of brain assault, or a Glasgow Coma Scale
(5) score of less than 15. These 196 patients formed the study group. The inclusion criteria mentioned above were used to confirm the clinical or radiological evidence of brain injury associated with the head trauma.
Patients were invited by mail to take part in the study. Those who did not respond received a reminder letter 6 weeks after the initial letter and again 12 weeks after. In some cases patients were contacted by telephone or through their general practitioners. Consultants under whose care the patients were admitted gave consent for research staff members to examine the patients’ medical case notes. The study was approved by the local district ethics committee. After complete description of the study to the subjects, written informed consent was obtained, copies of which were sent to the patients’ general practitioners.
A purpose-designed questionnaire was used to collect information from medical case notes and patient interviews in the following areas: age, sex, severity of head injury according to initial Glasgow Coma Scale scores (mild=15–13, moderate=12–9, severe <9), history of preinjury alcohol consumption, number of years of formal education, preinjury occupational status and social class, history of a previous head injury, history of a psychiatric illness, and family history of a psychiatric illness. Research staff members (I.L. and C.K.) interviewed most of the patients and their relatives at home approximately 1 year after the traumatic brain injury. The first 22 patients were jointly interviewed by the research staff members to improve interrater reliability. During the interview the researcher assessed the patient’s overall disability with the Glasgow Outcome Scale
(6) (1=dead, 2=persistent vegetative state, 3=severe disability, 4=moderate disability, 5=no disability). Category 5 (no disability) was considered as a favorable outcome, and the rest were considered as unfavorable outcomes according to the scale. Patients’ current cognitive ability was assessed by the Mini-Mental State examination
(7), and their premorbid IQ by the National Adult Reading Test (
8).
Psychiatric assessment was performed in two stages. First, all consenting patients were screened with the General Health Questionnaire, 28-item version
(9). The Clinical Interview Schedule—Revised
(10) and the Psychosis Screening Questionnaire
(11) were also administered. These two instruments were used in a study by the Office of Population Censuses and Survey (Department of Health, United Kingdom) and were shown to be reliable screening instruments for the detection of psychiatric cases in a general adult population
(12). Subjects who scored 11 or more on the General Health Questionnaire, scored 12 or more on the Clinical Interview Schedule—Revised, or had a positive score on any of the eight psychotic symptoms on the Psychosis Screening Questionnaire were classified as having cases of psychiatric illness.
Patients who were diagnosed as having a psychiatric illness in the screening stage underwent further assessment in the second stage with the Schedules for Clinical Assessment in Neuropsychiatry
(13), derived from the Present State Examination (PSE), within 4 weeks. The Schedules for Clinical Assessment in Neuropsychiatry is an internationally accepted, well-validated, and standardized semistructured interview which provides data that can be used in a computer program (CATEGO) to generate a psychiatric diagnosis according to ICD-10. The computer program also generates an index of definition score between 0 and 10. In this study an index of definition score of less than 4 was taken as evidence of the absence of a psychiatric disorder. Schedules for Clinical Assessment in Neuropsychiatry interviews were conducted by two psychiatrists (I.L. and I.A.) previously trained in administration of the instrument. Psychiatric symptoms within the 4 weeks prior to the interview were rated.
Statistical analysis of the data collected was performed with the use of the SPSS for Windows program
(14). Proportions with 95% confidence intervals (CI) were calculated. Chi-square analysis was used to compare rates of psychiatric illnesses among the patients with traumatic brain injury and the general population. A multiple logistic regression analysis of variables was carried out to assess the possible risk factors for precipitation of a psychiatric illness in the study group.
RESULTS
The age range of the 196 patients was 18–94 years (median=43.5 years; quartile=28). One hundred twenty-seven (65%) of the patients were male, and 69 (35%) were female. Thirty-two patients were either deceased or not available for an interview. The remaining 164 patients had face-to-face interviews. The age range of the 164 patients interviewed (110 male and 54 female) was 18–94 years. Eighty-two percent (N=134) had sustained a minor head injury, and 18% (N=30) a moderate to severe degree of head injury, according to the Glasgow Coma Scale scores.
One year after traumatic brain injury, 6.7% (N=12) of 180 patients had developed severe disability, 25.5% (N=46) had moderate disability, and 58.3% (N=105) had no disability according to the Glasgow Outcome Scale scores. The rest (9.5%, N=17) were either deceased or in a persistent vegetative state. Sixty-two patients were identified as psychiatric cases according to their scores on the General Health Questionnaire, of whom 28 also had a positive diagnosis according to their scores on the Clinical Interview Schedule—Revised. Of the 62 patients with positive cases, 45 (73%) consented to a Schedules for Clinical Assessment in Neuropsychiatry interview in the second stage. The age range of these 62 subjects was 18–87 years; 46 of them were male, and 16 were female. Of the 45 patients who had a Schedules for Clinical Assessment in Neuropsychiatry interview, 34 were male, and 11 were female, and their ages ranged between 20 and 72 years.
Of the overall study group (N=164), 30 patients (18.3%) had an ICD-10 psychiatric diagnosis according to the Schedules for Clinical Assessment in Neuropsychiatry interview (95% CI=12.9%–25.2%). Of the 45 patients who had a Schedules for Clinical Assessment in Neuropsychiatry interview, 66.7% (N=30) had a psychiatric diagnosis (95% CI=50.9%–79.6%). A higher proportion of patients with Clinical Interview Schedule—Revised positive cases (82%, N=23 of 28), compared with those with positive cases according to the General Health Questionnaire (48%, N=30 of 62), had a psychiatric diagnosis. Of the 30 patients who had an ICD-10 diagnosis of a psychiatric illness according to the Schedules for Clinical Assessment in Neuropsychiatry interview, 11 had an index of definition score of 4 or 5, 18 had a score of 6 or 7, and one had a score of 8. Of these 30 patients, six (3.7% of 164) had a diagnosis of alcohol dependence syndrome, and one (0.6% of 164) had a diagnosis of opioid dependence syndrome.
The most common diagnosis was depressive episode, which was present in 21 patients (12.8%; 95% CI=8.3%–19.1%) (five mild, 10 moderate, three severe, three severe with psychotic symptoms). The second most common diagnosis was panic disorder, which was found in 11 patients (6.7%; 95% CI=3.6%–12.0%). A diagnosis of panic disorder was associated with a diagnosis of alcohol dependence in four patients, depressive episode in five patients, obsessive-compulsive disorder in one patient, and generalized anxiety disorder in one patient. The third most common diagnosis was nightmare, which was diagnosed in seven patients (4.2%; 95% CI=1.9%–8.9%).
Three patients had a diagnosis of generalized anxiety disorder, two had obsessive-compulsive disorder, one phobic disorder, and one schizophrenia. Four patients showed symptoms of posttraumatic stress disorder at the time of the study. All of these patients had memory of the incident involving the head injury. Only 10 of the 30 patients with ICD-10 positive cases had a single psychiatric diagnosis. The rest had more than one psychiatric diagnosis (one had five diagnoses, one had four, four had three, and 14 had two). The patient with the diagnosis of schizophrenia had the maximum number of diagnoses, including depressive episode, schizoaffective disorder, sleep disorder, and obsessive-compulsive disorder. His psychiatric symptoms were long-standing and were present before the traumatic brain injury.
Twenty-six (21.7%) of the 120 adults between ages 18 and 64 years and four (9.1%) of the 44 adults over age 64 had an ICD-10 psychiatric diagnosis (95% CI=14.6%–29.8% and 3.1%–23.5%, respectively). In the Office of Population Censuses and Survey study
(12), 16.4% of 10,108 adults in the general population between ages 16 and 64 in the United Kingdom were shown to have an ICD-10 diagnosis of a psychiatric disorder on the basis of symptoms expressed within the previous 4 weeks of the study. However, in that study psychiatric diagnoses were made according to an algorithm based on Clinical Interview Schedule—Revised symptom ratings but not on the basis of a Schedules for Clinical Assessment in Neuropsychiatry interview.
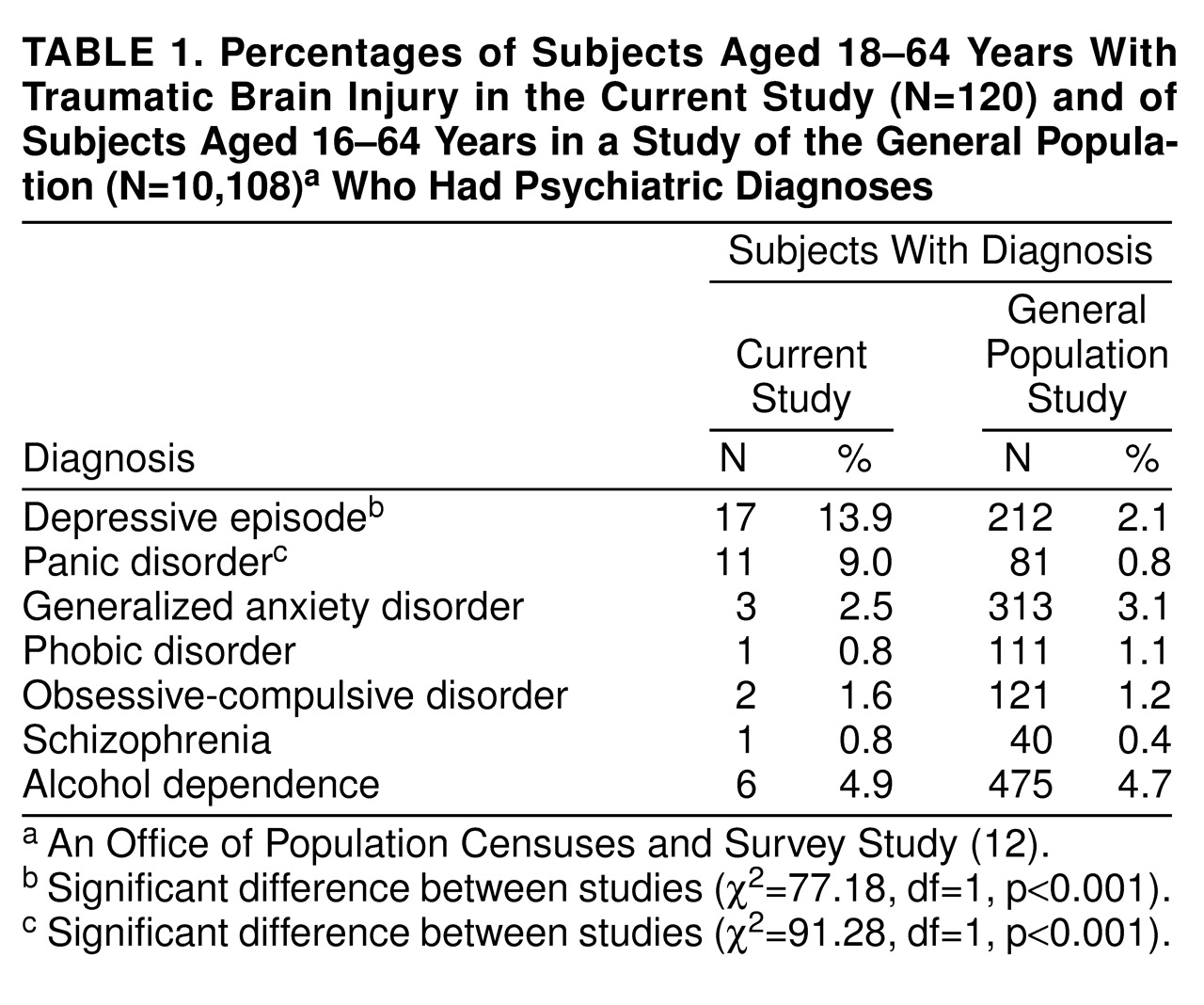
Table 1 shows the rates of psychiatric disorders found among the 18- to 64-year age group in the present study and those in the Office of Population Censuses and Survey study. In
Table 1 the prevalence of a depressive episode alone (2.1%) according to the Office of Population Census and Survey study is shown. In the same study 7.7% of the subjects also showed mixed anxiety and depressive disorder; these data were not used for comparison with the data from the current study. A chi-square analysis did not show a statistically significant difference in the rate of psychiatric illness among the 18- to 64-year age group of patients in the current study (21.7%) when compared with that among the 16- to 64-year age group of adults in the general population in the Office of Population Censuses and Survey study (16.4%) (χ
2=2.12, df=1, p=0.14).
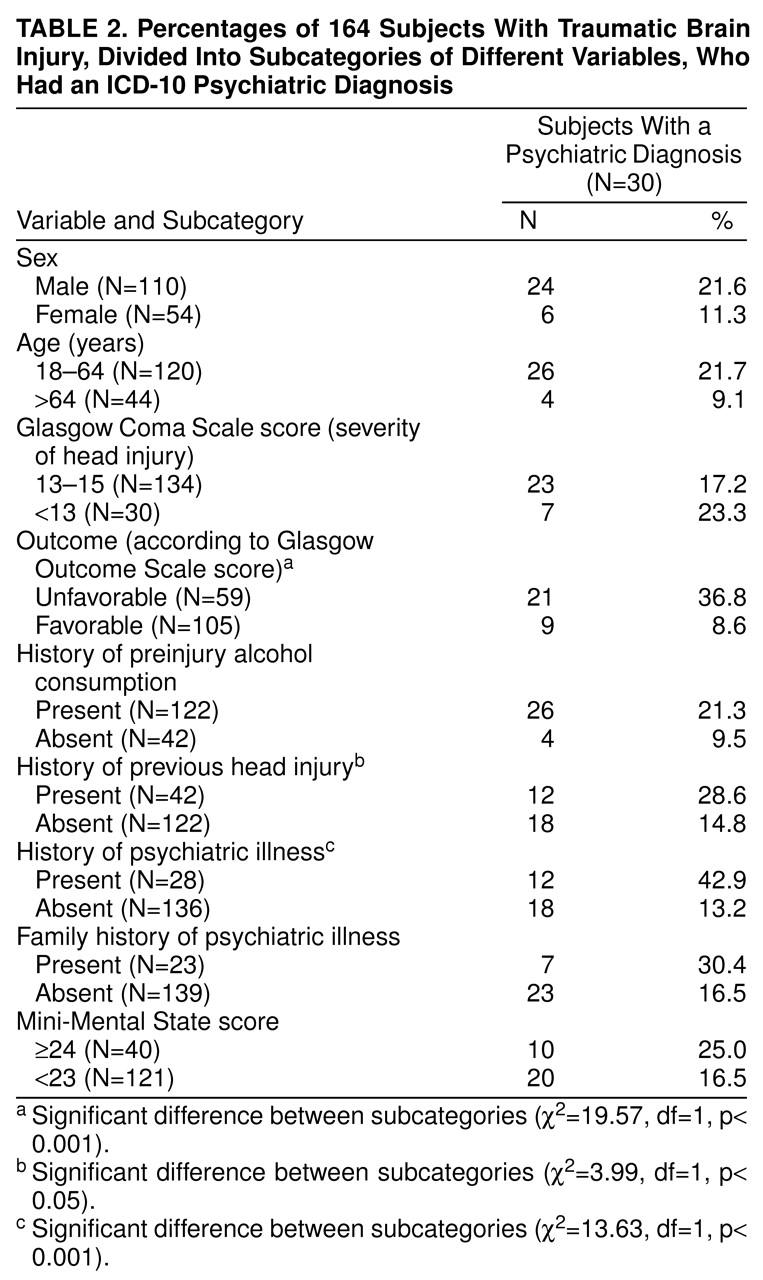
A multiple logistic regression analysis was carried out by using the presence or absence of a psychiatric diagnosis as a dependent variable and the following risk factors as covariates: age, sex, history of preinjury alcohol consumption, initial severity of head injury according to the Glasgow Coma Scale score, current level of disability according to the Glasgow Outcome Scale score, level of premorbid cognitive function according to the National Adult Reading Test score, previous history of a psychiatric illness, previous history of a head injury, family history of a psychiatric illness, number of years of formal education, and level of current cognitive deficit according to the Mini-Mental State score. The percentages of patients in each subcategory of these variables (e.g., 21.6% of male patients versus 11.3% of female patients, 17.2% of the mildly head-injured versus 23.3% of the moderately to severely head-injured, etc.) who had a diagnosis of a psychiatric illness are shown in
table 2. According to the logistic regression analysis, there was a statistically significant association (at the 0.05 level or better) between the presence of a psychiatric illness and a younger age, a poorer outcome according to Glasgow Outcome Scale score, a history of preinjury alcohol consumption, a history of a psychiatric illness, a lower Mini-Mental State score, and a lower number of years of formal education. Thirty-four patients (20.7%) were involved in compensation claim litigation at the time of the study. A chi-square analysis did not reveal any statistically significant intergroup difference in the prevalence of psychiatric illness between those who were involved and those who were not involved in a compensation claim (χ
2=0.10, df=1, p=0.74).
DISCUSSION
As far as we know, this is the first report of a higher rate of ICD-10 psychiatric diagnosis among adult patients with traumatic brain injury compared with a general population. This is also the first report of a significantly higher rate of depressive episode and panic disorder among patients with traumatic brain injury. Although there have been previous studies of depressive symptoms among such patients
(15–
19), there has been only one study
(20) of the rate of depressive disorder diagnosed in this patient population with use of the PSE (predecessor of the Schedules for Clinical Assessment in Neuropsychiatry). This also seems to be the first report on the relatively significant influence of risk factors such as a younger age, a history of preinjury alcohol consumption, a lower cognitive score, a history of a psychiatric illness, an unfavorable global outcome, and fewer years of formal education on the prevalence of psychiatric illness after traumatic brain injury.
The findings of the current study, however, have to be interpreted in the context of certain methodological problems. In any study of patients with traumatic brain injury, there remains the problem of case ascertainment, case definition, and case detection. It is not easy to define a head injury. It is even more difficult to define a traumatic brain injury where there is evidence of injury to the brain occurring in the context of a head trauma. As much as possible, this study’s inclusion criteria ensured that the patients in the study not only had a head injury but also showed indirect evidence of brain assault. The psychiatric consequences of a road traffic accident have been studied
(21). Therefore, the particular interest of this study was to assess the psychiatric consequences of a brain injury as opposed to a head injury. However, the findings of this study are based on a subset of patients with head injury who attended the local accident and emergency department, and thus they have to be interpreted within that context. Not all of the medical case notes were available for scrutiny, and in a number of case notes, no documentation on the length of coma or Glasgow Coma Scale score was found. It is also likely that by using ICD-9 codes to access the Health Authority’s database, we had an incomplete list of hospitalized patients with traumatic brain injury
(22).
The relationship between the timing of the traumatic brain injury and the occurrence of the psychiatric symptoms is also important. In a cross-sectional study such as this, it is always difficult to assess the course of psychiatric illness over a period of time, which in the case of traumatic brain injury patients is likely to change. The lack of a properly matched control group is a drawback of the current study. However, it is well-known that patients with traumatic brain injury are often young men who come from a lower socioeconomic background, tend to misuse alcohol and drugs, and possess certain premorbid personality traits. These characteristics may make them vulnerable to developing psychiatric illness but at the same time make it difficult to find a properly matched control group for them.
It is difficult to compare our findings with previous studies because of the relative paucity of information on this subject. Fenton and colleagues
(23) assessed 41 consecutive admissions of head-injured patients with the PSE 6 weeks after injury and found that 39% had a psychiatric diagnosis. Most of the other studies in this area reported primarily on psychiatric symptoms rather than a full spectrum of psychiatric syndromes. The reported rate of depression seems to vary between 26% and 60% according to different studies
15–
(19). The number of subjects in these studies varied between 18 and 66.
Using DSM-III-R criteria, Jorge and colleagues
(20) found that 42.42% of 66 head-injured patients suffered from major depression. Seventeen (25.75%) had the diagnosis in the acute stage (at 3-month follow-up), and 11 (16.66%) had the diagnosis at 12-month follow-up. At 12-month follow-up, the rate of depressive disorder in that study was marginally higher than the rate in our study. This could be explained by the presence of a higher proportion of patients with moderate and severe head injury in the study by Jorge et al. Anxiety symptoms have been reported in 24%–28% of patients with traumatic brain injury in the past
(18,
19). Schoenhuber and Gentilini
(24) compared the rate of generalized anxiety disorder in a group of head-injured patients and a control group; no significant difference was detected. The data on the rates of panic disorder, obsessive-compulsive disorder, and manic disorder in patients with traumatic brain injury have come primarily from case reports. One small-group study involving 18 patients
(19) found that one person (5.5%) had a diagnosis of obsessive-compulsive disorder, and another person had a diagnosis of panic disorder.
Although in the current study panic disorder was the second most common diagnosis after depressive episode, it was almost inevitably associated with other psychiatric diagnoses, mainly alcohol dependence syndrome and depressive episode. However, the research staff were careful not to include symptoms of alcohol withdrawal as part of a diagnosis of panic disorder. A provocative hypothesis is that panic disorder in this study group may have been an unusual expression of posttraumatic stress disorder because the patients lost the memory of the incident involving the head injury. In the absence of data available from either a sample based on the general population or any previous study involving patients with traumatic brain injury, it is difficult to comment on the high rate of sleep disorder, particularly nightmares, observed in the current study. It is worth mentioning, however, that these nightmares were not associated with any flashback of the original incident.
Lishman
(25) hypothesized that many of the psychiatric symptoms following a head injury are precipitated initially by organic factors, but in some patients they are maintained by psychosocial factors for a long period of time. Psychosocial factors may include the patient’s socioeconomic status and premorbid personality. Although it was not possible for us to adequately assess the premorbid personality of the patients in our study, the fact that a history of psychiatric illness remained the most important predictive factor in precipitating a psychiatric illness 1 year after traumatic brain injury seems to support Lishman’s original hypothesis. In this patient group there were other possible risk factors for the development of psychiatric illness that did not reach the level of statistical significance but nevertheless showed a difference. These were male sex, severe head injury, and a family history of psychiatric illness. However, psychiatric illness was significantly more common among the patients who showed unfavorable outcome according to the Glasgow Outcome Scale 1 year after traumatic brain injury. It is interesting that premorbid factors such as lower social class and lower educational achievement, head-injury-related factors such as a low Glasgow Coma Scale score, and outcome-related factors such as the presence of disability and psychiatric “caseness” according to the Clinical Interview Schedule—Revised significantly influenced the rate and the pattern of neurobehavioral symptoms in the same study group
(26); as in the present study, the rate of neurobehavioral symptoms was not related to the rate of compensation claims. It is now being accepted that the occurrence of a psychiatric illness following traumatic brain injury depends on a complex interaction among psychosocial and organic factors, and the findings of the current study are broadly supportive of that notion.