Traditionally, therapeutic interventions for schizophrenia have been evaluated for their effectiveness in reducing symptoms, especially symptoms of psychosis, which are central to the definition of the disorder
(1,
2). However, there has been increasing interest in the ability of such interventions to reduce negative symptoms and/or the cognitive dysfunctions that often accompany schizophrenia
(3–
5). This is at least partially a result of data indicating that level of performance in various cognitive domains may be important in the prediction of adjustment to and functioning in the community
(6,
7). Indeed, in a review of the relevant literature, Green concluded, “Certain neurocognitive measures are more strongly associated with functional outcome than are psychotic symptoms”
(6, p. 327). Green tempered his conclusions by noting that the number of prospective studies evaluating neurocognitive predictors of functioning is remarkably small.
Aggregating results across studies, each of which may not include both symptom and neurocognitive measures, risks confounding differences in the predictive value of indices with differences in the characteristics of the study groups. Studies comparing the predictive value of symptoms and neurocognitive indices in the same group of patients are, therefore, particularly important. Of the studies reviewed by Green, only three
(7–
9) contrasted in the same group of patients the power of symptoms versus neurocognitive measures to prospectively predict subsequent community functioning.
Wykes et al.
(8) examined measures of response processing time and symptoms (assessed with the Present State Examination) as predictors of the level of care required by chronically ill psychiatric patients (most of whom had a diagnosis of schizophrenia) at 6 months, 18 months, and 3 years after initial assessment. Only response processing time, in conjunction with some demographic variables, predicted subsequent level of care, especially night care. Interpretation of these findings is complicated by the fact that the measure of response processing was related to the initial level of care, whereas symptoms were not. It is possible, therefore, that the superiority of the cognitive measure in predicting subsequent level of care reflects a confounding with the initial level of care—patients initially in long-stay wards having longer response processing time.
Among 237 first-episode patients, Johnstone et al.
(7) found that employment status after 2 years (stable or improved versus worse or no occupation) was predicted by aspects of what are generally known as negative symptoms, but not by such cognitive measures as digit symbol substitution or picture vocabulary tests. Unambiguous measures of psychotic symptoms were not reported.
Goldman et al.
(9) assessed the value of positive and negative symptoms and several aspects of cognitive functioning in predicting 1-year outcome for 19 acutely ill schizophrenic inpatients. Semantic memory function at initial assessment was found to predict outcome defined by total score on the Strauss-Carpenter scale at 1 year, while cognitive measures involving construction ability, sustained attention, executive functioning, and general verbal intellectual functioning were not significant predictors. Although symptoms early in the course of the acute episode did not predict 1-year outcome, the levels of positive and negative symptoms present after approximately 4 weeks of treatment were better predictors of long-term outcome than any cognitive measures.
A review of the preceding three studies shows that up to the time of Green’s review, research evaluating the comparative power of cognitive and symptom measures to predict subsequent outcome in the same group of patients actually yields results not entirely supportive of the conclusion that cognition is a better predictor than symptom measures. Of particular importance is the observation from Goldman et al.
(9) that symptoms after treatment may be more predictive of long-term outcome than are symptoms at the time of an acute episode. Such a proposition is intuitively compelling and also consistent with observations by others
(10,
11).
In the current paper we present data relevant to the prediction of social functioning from both cognitive performance and psychopathology measures. These data are based on cognitive and symptom measures collected for patients who were part of an earlier study
(12) in order to predict level of social functioning as subsequently assessed in a community treatment program based in a teaching hospital. The data that were available on these patients allowed us to assess several issues of particular importance in understanding these relationships. As Green
(6) commented, it is important to investigate further the relationship of cognitive functioning and symptoms to specific and differentiated aspects of community functioning rather than composite or summary indices. In the current study, we used the Life Skills Profile
(13), which, in addition to providing an overall index of community functioning, allows differentiation of the five specific domains of self-care, nonturbulence, social contact, communication, and responsibility.
Green
(6) noted that data concerning the ability of negative symptoms to predict social and community functioning are inconsistent. The interpretation of such inconsistent relations between negative symptoms and outcome is complicated by several factors; two of the most paramount are the likely conceptual overlap between aspects of negative symptoms and community functioning (see also reference
14) and findings
(14,
15) that symptoms in schizophrenia are probably best conceived of as constituting at least three rather than two dimensions—reality distortion, disorganization, and psychomotor poverty. As aspects of disorganization are varyingly identified as positive versus negative symptoms, clearer findings regarding the relationship of symptoms to functioning may emerge when this more differentiated approach to symptom categorization is used. In this study, we used indices of negative symptoms that do not directly overlap with measures of community functioning, and we separately examined conceptual disorganization as a predictor of such functioning.
Finally, the data reviewed by Green
(6) led him to conclude that verbal memory is more likely to be related to various aspects of community functioning than are other aspects of cognitive functioning. The data to be reported allow a direct test of this hypothesis.
METHOD
Subjects
Measures of symptoms and neurocognitive functioning were collected as part of a research protocol for an earlier neurocognitive study
(12). Fifty of the patients who participated in that study subsequently received treatment in the Community Treatment and Reintegration Program of London Health Sciences Centre in London, Ont., Canada. For these patients, it was possible to retrieve information concerning social and community functioning by using the Life Skills Profile, which had been introduced to the monitoring protocol of the program. The Community Treatment and Reintegration Program provides case management, medication, family intervention, and other psychosocial services to individuals living in the community.
All subjects had a DSM-III-R diagnosis of schizophrenia as confirmed by the Structured Clinical Interview for DSM-III-R
(16). All subjects were between the ages of 17 and 60 years. After completely describing the study to subjects, we obtained written informed consent.
Cognitive Measures
The cognitive tests had been selected to reflect functioning in the brain areas most frequently implicated in the pathophysiology of schizophrenia. More details concerning the tests, their administration, and the rationale for their selection can be found elsewhere
(12).
Performance on the Wisconsin Card Sorting Test
(17) appears to be particularly sensitive to dorsolateral frontal lobe function, and it is widely considered to reflect the cognitive functions (abstraction, planning, formation, and shifting of cognitive sets) most frequently found to be compromised in schizophrenia (for instance, see reference
18). The number of categories correctly achieved and the percentage of perseverative errors are the most commonly used indices of performance on the Wisconsin Card Sorting Test and were calculated for the subjects in this study.
The Rey Auditory Verbal Learning Test
(19) and the logical memory test of the Wechsler Memory Scale—Revised
(20) both assess verbal memory, and dysfunction on such tests has been most strongly associated with left temporal lobe anomalies. For the Rey Auditory Verbal Learning Test, we used the average number of words correctly recalled in six trials. For the logical memory test of the Wechsler Memory Scale, we recorded the average number of correct recalls on the immediate- and delayed-recall tests.
The Benton Visual Retention Test
(21) and Rey-Osterrieth Complex Figures test
(22) assess visual memory, and performance on these tests is typically associated with right temporal lobe function. The Benton Visual Retention Test was scored by using the criteria recommended by Benton
(21), and the Rey-Osterrieth Complex Figure test was scored on the basis of the delayed-recall trial.
Scores on the Design Fluency Test
(23) were calculated by using the total number of acceptable designs generated by the subjects in both the unrestricted portion of the test and the portion in which designs are restricted to four lines. The total score on the Chicago Word Fluency Test
(24) was calculated on the basis of the number of generated words beginning with “S” followed by the number of generated words beginning with “C.” Scores on the design and word fluency tests have been found to be especially sensitive to right and left basal frontal cortical functions, respectively
(23,
25).
Assessment of Symptoms
Symptoms were assessed by using the Scale for the Assessment of Positive Symptoms (SAPS)
(26) and the Scale for the Assessment of Negative Symptoms (SANS)
(27). Symptoms were rated with regard to the 1 month before the assessment. The assessments were carried out by one of two psychiatrists (A.M. or L.C.) or a clinical psychologist (R.N.). The patients were in a relatively stable state following treatment of any recent acute episodes, and the symptoms assessed primarily reflect residual symptoms that the patients were experiencing.
The scoring of the three syndromes of psychomotor poverty, disorganization, and reality distortion was based on the method used by Liddle and Morris
(28). The psychomotor poverty syndrome was scored by using the score for poverty of speech, the score for decreased spontaneous movement, and the average for four items reflecting aspects of blunting of affect (affective nonresponsivity, unchanging facial expression, paucity of expressive gestures, and lack of vocal inflections). The rating for the disorganization syndrome was the sum of the scores for inappropriate affect and for poverty of content of speech and the global rating of positive formal thought disorder. The score for the reality distortion syndrome was the sum of the scores on the items for auditory hallucinations commenting on the patient’s behavior, for persecutory delusions, and for delusions of reference. There were no significant intercorrelations between the three syndrome scores (r values ranged between 0.05 and –0.04).
The Liddle-Morris method of deriving the three syndromes was chosen because the items used for calculation of each of the three syndromes do not have substantial direct overlap with the items included in measures of social functioning, such as the Life Skills Profile. This selection of items was designed to directly reflect underlying psychopathology rather than partially or entirely reflecting self-care or social and occupational functioning
(14).
Community Functioning
The Life Skills Profile
(13) was completed by case managers within the Community Treatment and Reintegration Program. The case managers are qualified psychiatric nurses with additional undergraduate degrees in behavioral or social science who follow their patients over the years and have ample opportunity to observe and assess patient functioning in various community settings. The Life Skills Profile was designed specifically to assess constructs of relevance to survival and adaptation in the community. Its development was based on sound psychometric procedures, and the scale has demonstrated good internal consistency of subscales and adequate interrater reliability
(13). The 39 items of the scale measure five key dimensions: self-care (grooming, hygiene, budgeting, food preparation, etc.); nonturbulence (degree of offensiveness, violence, intrusiveness, anger control, etc.); social contact (friendships, interpersonal interests and activities, etc.); communication (conversational skills, inappropriate gesturing, etc.); and responsibility (cooperativeness, responsibility regarding personal property and medication, etc.).
Multiple assessments on the Life Skills Profile were completed as part of the monitoring protocol for patients within the program and were carried out without reference to or knowledge of patient data (symptoms or cognitive scores) in the neurocognitive study. For patients for whom multiple Life Skills Profiles were available, it was deemed most appropriate to aggregate these assessments by calculating average scores across time. The average length of time between a patient’s symptom and cognitive assessments and the first Life Skills Profile assessment was 10.6 months (range=1–31), and the average number of assessments available per patient was 3.4 (range=1–8).
RESULTS
Subject Characteristics
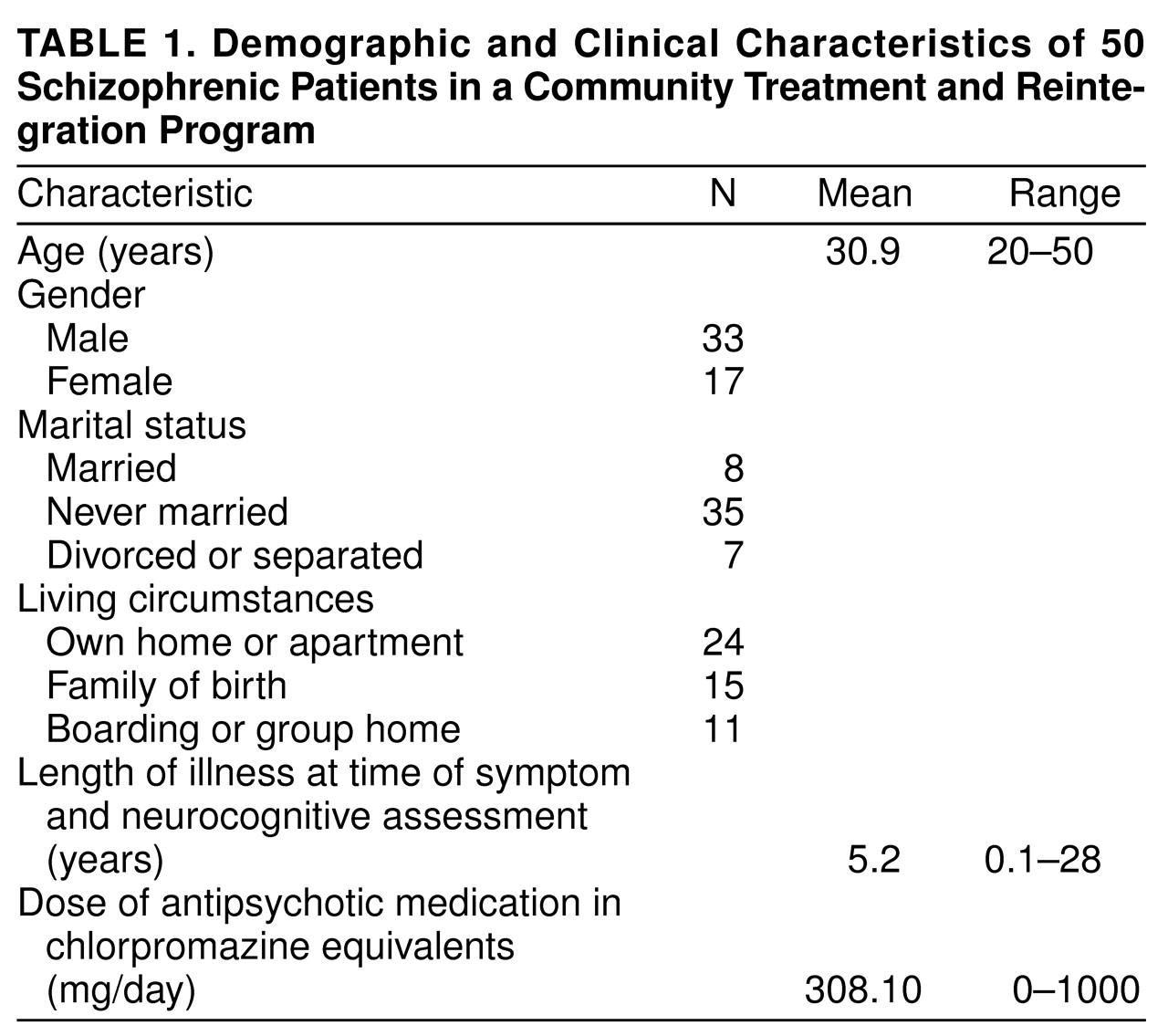
Table 1 presents the demographic and clinical characteristics of the study group. There was a considerable range of age and length of illness. Approximately two-thirds of the subjects were male, the majority had never been married, and approximately one-half were living in their own homes or apartments.
Relation of Symptoms and Cognition to Social Functioning
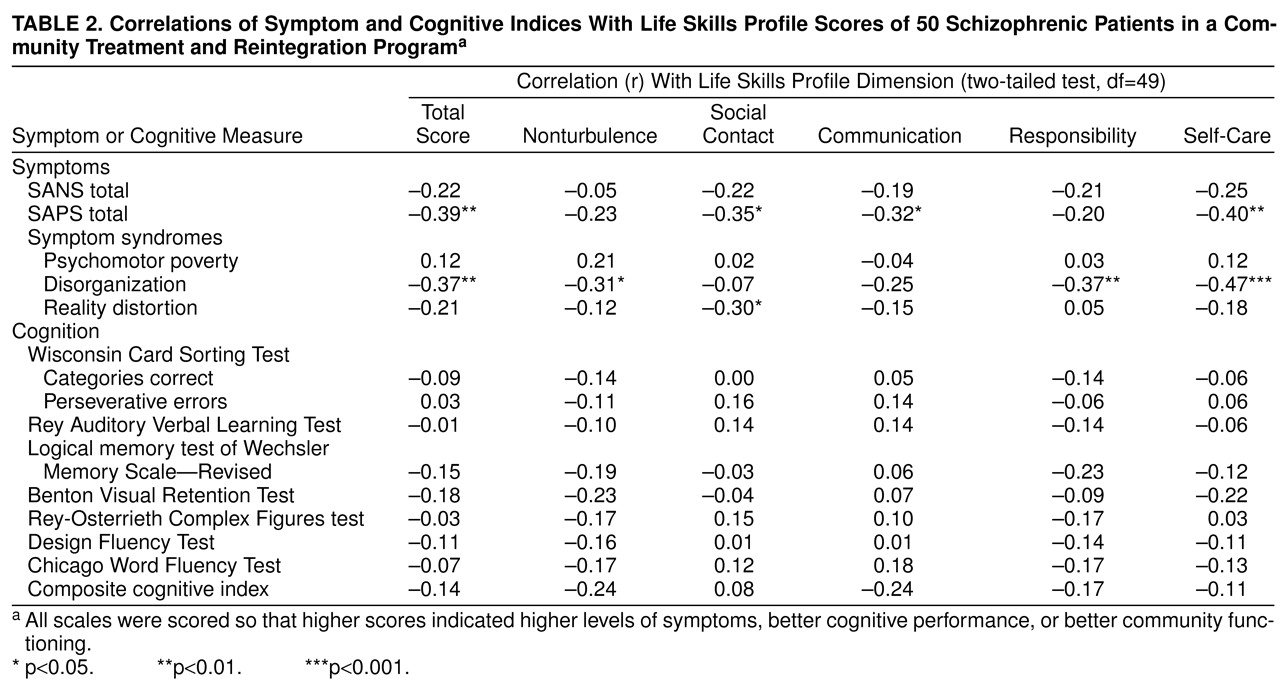
Table 2 presents the bivariate product-moment correlations of the symptom and cognitive indices with scores on the Life Skills Profile. A similar pattern of results was found when the relationships were assessed by using Spearman rho. All scales included in
table 2 were scored so that higher scores indicated higher levels of symptoms, better cognitive performance, or better community functioning. Only the symptom measures showed significant correlations with subsequently rated community functioning. When these relationships are examined in terms of the traditional distinction between positive and negative symptoms, it appears that positive symptoms are more reliably related to functioning as assessed by the Life Skills Profile. When we analyze symptoms by using the tripartite distinction between psychomotor poverty, disorganization, and reality distortion, it is disorganization that shows the most reliable relationship to community functioning—having a significant negative correlation with total score on the Life Skills Profile and three of the five subscales (nonturbulence, responsibility, and self-care). The other significant correlation is between greater reality distortion and less social contact.
The absence of a relationship between formally assessed cognitive functioning and community functioning might reflect the fact that the cognitive tests used were assessing quite specific cognitive capabilities, and community functioning might prove to be more strongly related to a composite index of cognitive functioning. For this reason, we calculated a composite index by adding the Z score transformations of each subject’s performance on the cognitive tests. The correlations reported in the bottom row of
table 2 show that this composite index did not show a significant correlation with any of the Life Skills Profile indices.
Another possible explanation for the failure to find significant correlations with the cognitive measures could be a restricted range in the scores on these indices. This does not provide an explanation as on all cognitive indices the standard deviation of the scores was equal to or greater than that reported for the general population
(29).
In order to assess the possibility that the correlations between the symptom measures and indices of community functioning were at least partially mediated by cognitive dysfunction, we calculated partial correlations between the various symptom scores and the Life Skills Profile scores while controlling for scores on the composite cognitive index. The resulting partial correlations showed the same pattern of significant relationships between symptoms and community functioning as presented in the upper portion of
table 2.
Medication as Possible Mediator
It is conceivable that medication-related factors could serve as mediators of some of the relationships found between symptom indices and community functioning. Neuroleptic or anticholinergic medication may be prescribed in higher doses for more symptomatic patients, and there may be adverse effects of such medication on aspects of day-to-day functioning
(30). It could also be that patients who are less likely to take their medication are more likely to have higher levels of symptoms and to have greater difficulty in community functioning.
Case records provided information by which to estimate daily chlorpromazine equivalences of neuroleptic doses and benztropine equivalences of each patient’s antiparkinsonian medication (anticholinergics) for the period between the symptom and cognitive assessment and the final Life Skills Profile assessment. In addition, at the time that the symptom and cognitive assessments were being completed, the clinician with primary responsibility for the care of each patient had been asked to rate on a 7-point scale that patient’s overall conscientiousness in taking the prescribed medication. The clinicians usually had long-standing knowledge of the patients and were able to assess medication-taking behavior on the basis of corroboration from several sources, including relatives, other clinicians familiar with the patient, relevant blood level assessments, and reports from community workers. We carried out a series of partial correlations parallel to the bivariate correlations presented in
table 2, removing variance possibly attributable to each of the three medication-related variables. Most of the significant correlations shown in the upper portion of table 2 were not notably changed by partialling out neuroleptic or anticholinergic dose. The exceptions were the loss of significance for the correlation between the disorganization syndrome and the nonturbulence subscale of the Life Skills Profile when either dose was controlled. In addition, the correlation between reality distortion and social contact became of borderline significance when either dose was partialled out.
The effects of partialling out medication-taking behavior were more substantial. The correlations of the total SAPS score with the total Life Skills Profile score and with each of the communication and self-care subscales became nonsignificant, as did the correlation between disorganization and nonturbulence.
Statistically controlling for medication-related variables had no noteworthy impact on any of the nonsignificant relationships between the cognitive indices and Life Skills Profile scores.
DISCUSSION
Why are the results of this study inconsistent with Green’s conclusion
(6) that neurocognitive measures are more strongly related to functioning in the community than symptom measures? One possibility is that the neurocognitive measures included in this study are not those most likely to prove to be related to community functioning. This seems unlikely to provide an explanation. An examination of Green’s review reveals that he concluded that the measures most consistently related to community functioning outcomes were “secondary verbal memory” and “card sorting/executive functions,” both of which were well represented in this study. Indeed, Green felt that the evidence for the importance of verbal memory was sufficient to justify an a priori hypothesis that it (and vigilance, which unfortunately is not represented in our data) would predict community functioning.
A second possibility is that the cognitive measures were assessed further in advance of the measures of community functioning than were symptom assessments. Although the symptom and cognitive assessments were carried out by different individuals (kept blind as to one another’s findings), both sets of assessments were typically completed within a span of 1 to 2 weeks. Furthermore, the cognitive assessments were almost always carried out after the symptom assessments, so any bias introduced would tend to favor the cognitive measures over the symptom measures.
As noted earlier, a careful inspection of past studies in which symptoms and neurocognitive measures were used with the same subjects prospectively to predict community functioning does not strongly favor cognitive measures as a better predictor. Furthermore, there is evidence that it may be important to use symptoms after optimal treatment rather than acute symptoms as predictors of subsequent community functioning
(9–
11). At least some of the failures to find symptoms predicting level of community functioning in past studies may reflect the use of acute symptoms rather than symptoms after treatment of an acute episode.
Our finding that symptoms (particularly disorganization symptoms) are more strongly related than formal cognitive test scores to community functioning appears inconsistent with two recent reports of cross-sectional data. Both Dickerson et al.
(31) and Velligan et al.
(32) found evidence that symptoms did not relate to social functioning as strongly as did cognitive measures. It should be noted, however, that neither of these studies clearly separated out the disorganization syndrome that our data suggest to be the best symptom-related predictor of community functioning. In addition, one of these studies
(32) was based on subjects undergoing hospitalization for acute symptoms, and it was not clearly specified during which period of time the symptoms were being assessed.
As Green
(6) noted, there needs to be more research examining prospective predictors of various domains of community and social functioning in patients suffering from psychotic illnesses such as schizophrenia. Environmental factors may moderate the relative importance of cognition and symptoms as predictors of community functioning. Subjects in this study were clients of a comprehensive community treatment and reintegration program
(33) that, among other things, attempts to optimize the match between clients’ needs and capacities and their living environment. Such services may buffer the influence of cognition on community functioning. We are sympathetic to the suggestion that cognitive functioning is an important dimension along which to evaluate treatment outcome, and our clinical experience leaves us convinced that such neurocognitive processes can have important implications for patients’ quality of life, but the current results suggest caution in concluding that symptoms are always less important than cognition in this respect.
We found disorganization to be the most reliable predictor of several aspects of community functioning. On the other hand, low social contact (friendships and interpersonal interests) seems primarily related to a high level of reality distortion. The latter relationship is likely to reflect the disruptive impact of common delusional and hallucinatory experiences on the ability to cultivate and maintain interpersonal relations. The Life Skills Profile does not directly assess employment behavior, and cognition may be a stronger predictor of employment-related behavior or other aspects of community functioning that were not assessed in our study. Recent findings by Hoffman and Kupper
(34), however, support the particular importance of disorganization symptoms as correlates of work performance.
Although conceptual disorganization, in itself, might appear to reflect cognitive impairment, it is interesting that, in our data, relevant partial correlations showed conceptual disorganization as a symptom dimension to be a substantial predictor of community functioning independently of formally assessed neurocognitive performance. Future investigations should examine the extent to which the relationship between disorganization and aspects of community functioning might be mediated by other formally assessed cognitive functions, such as attention.
Our finding that disorganization symptoms are particularly related to poorer outcome implies that it is important to explore the extent to which therapeutic interventions affect this dimension. It is possible that the medications used in this study group did not produce adequate change in these symptoms in at least a proportion of the patients. This may, at least partially, be the result of lack of adherence to antipsychotic drug therapy by patients showing only partial resolution of their symptoms, and the results of our partial correlations controlling for medication-taking behavior provide support for such a contention. The fact that the patients in the current study were primarily being treated with typical neuroleptics may also explain the levels of residual symptoms.
Unfortunately, clinical trials of even newer “atypical” antipsychotic agents fail to examine their differential efficacy in relation to the disorganization dimension, although a noteworthy exception is the recent contrast of the effects of risperidone and haloperidol
(35). Most reports of clinical trials also fail to indicate the level of residual symptoms following use of typical or atypical agents in the treatment of acute psychotic episodes. Future research should examine the effects of newer treatments on a more differentiated basis than in the past—separating out various symptom complexes such as disorganization—and examine which if any of these changes mediates a better functional outcome in the long term.