Several lines of evidence, including consistent observation of a negative association between rheumatoid arthritis and schizophrenia
(1), suggest that the human lymphocyte antigen (HLA) region is a candidate locus for a susceptibility gene for schizophrenia. Previously
(2), we observed a nonsignificant positive association of HLA-DR1 with schizophrenia in a small number of Japanese subjects. The result appeared consistent with another relatively small serological study of HLA-DR in Japanese subjects
(3). To draw a conclusion regarding these findings, however, further studies with larger numbers of subjects are required. A negative association between schizophrenia and HLA-DR4, which is positively associated with rheumatoid arthritis, has been reported in Caucasian subjects
(4). Two Japanese studies
(2,
3) found slightly lower rates of HLA-DR4 in patients with schizophrenia than in normal subjects; however, the difference did not reach statistical significance, possibly due to the limited number of subjects. Because further investigations of the rates of HLA-DR1 and HLA-DR4 are of interest, in the current study we performed HLA-DR typing in a large number of Japanese patients with schizophrenia and healthy comparison subjects.
METHOD
The subjects were 233 unrelated Japanese patients; 112 were men, and 121 were women. Their mean age was 38 years (SD=10). All of the patients met DSM-IV criteria for schizophrenia; 132 were recruited from the outpatient psychiatric clinics of Teikyo University Hospital in Tokyo and Teikyo University Mizonokuchi Hospital in Kawasaki. Approximately half of these 132 patients had a history of psychiatric hospitalization. The remaining 101 patients were recruited from the inpatient wards of Kichijoji Mental Hospital and Toda Mental Hospital in Tokyo. All of the hospitals were within a 20-km radius of Tokyo. Written informed consent was obtained from all subjects. The comparison group comprised 493 unrelated healthy Japanese subjects who resided in the Tokyo area. Details of the comparison group have been described elsewhere
(5).
The HLA typing was performed by using polymerase-chain-reaction-based microtitre plate hybridization; details of this genotyping method have been described elsewhere
(6). In the whole typing procedure, the low-resolution DR types were determined first. Then, the alleles of each DR type were studied by the high-resolution microtitre plate hybridization method or the single-strand conformation polymorphism method (for the DR1 alleles). The results of the microtitre plate hybridization were automatically analyzed by using a personal computer, which was combined with a microtitre-plate reader. For DR4, the determination of the alleles by the high-resolution typing was conducted in the subjects of our previous study
(2), as well as those in this study. Chi-square tests were used to determine the statistical significance of differences between groups.
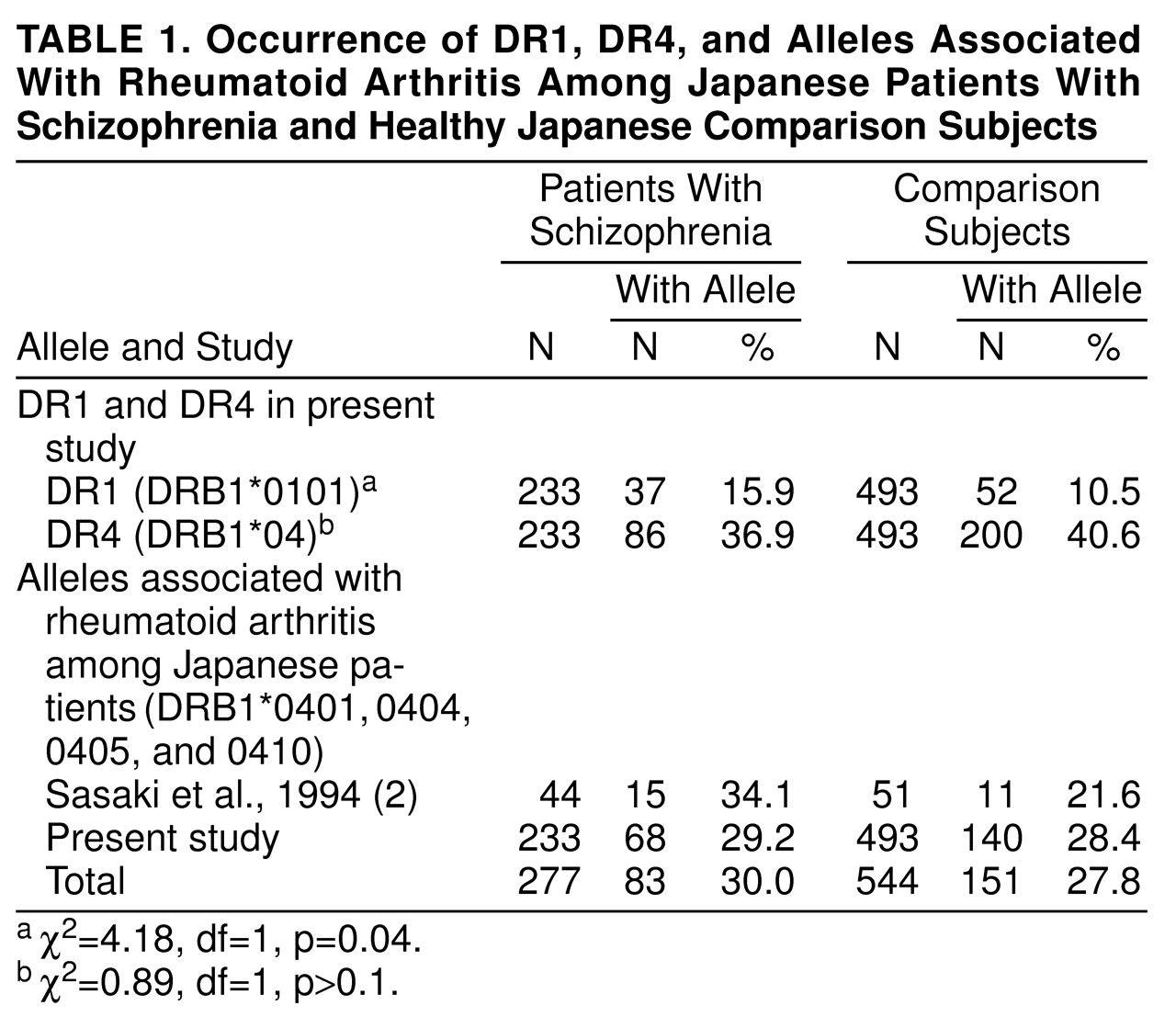
DISCUSSION
We found a significantly higher rate of HLA-DR1 (DRB1*0101) in Japanese patients with schizophrenia than in normal subjects in the present study. A higher rate of HLA-DR1 in patients with schizophrenia in the Japanese population was first reported in a small serological study
(3), which we replicated in a small DNA-based study
(2). Recently, another Japanese group (Arinami et al.
[7]) also observed a significantly higher rate of DR1 (DRB1*0101) in patients with schizophrenia (15.4%) than in subjects without schizophrenia (8.9%) (χ
2=5.47, df=1, p=0.02). Thus, the findings of all four studies examining this gene, without exception, support a higher rate of HLA-DR1 in patients with schizophrenia in the Japanese population.
Among the combined group of subjects from the three DNA-based studies
(2,
7, and the present study), the significance of the difference in rates of DR1 between the patients with schizophrenia and the normal subjects (88 [16.2%] of 543 patients compared with 82 [9.9%] of 825 normal subjects) reached a p value of 0.0006 (χ
2=11.82, df=1). We conclude, therefore, that HLA-DR1 (DRB1*0101) may be positively associated with schizophrenia in the Japanese population, although its role in the development of the disease may be relatively small or confined to a limited portion of the patients.
A slight, nonsignificantly lower rate of DR4 was observed in the patients with schizophrenia in the present study; this finding is similar to the findings of previous Japanese studies
(2,
3). Another recent study
(7), however, observed a significantly lower rate of DR4 in patients with schizophrenia (p=0.02). When we combined the data from our present and previous
(2) studies with those of the recent study
(7), we found a higher level of significance (χ
2=7.86, df=1, p=0.005) for the lower rate of DR4 in patients with schizophrenia (181 [33.3%] of 543 patients compared with 337 [40.8%] of 825 comparison subjects). This finding is consistent with the report of a lower rate of DR4 in Caucasian patients with schizophrenia
(2).
DR4 data should be interpreted with caution because statistical significance has been generated only in one
(7) out of four Japanese studies. Also, the rates of the DR4 alleles, which are associated with rheumatoid arthritis in the Japanese population, were not lower in our studies (
table 1). These alleles were not investigated by Arinami et al.
(7). Therefore, it is not clear whether the association is related to the lower rate of rheumatoid arthritis in schizophrenia in Japanese subjects.
Further studies, especially in other populations, would be of interest. Thus far, higher rates of DR1 have been observed in patients with schizophrenia from the Turkish population, although the authors concluded that this might be due to some biases
(8). No other studies have observed higher rates of DR1 in schizophrenia. The lower rate of DR4 in Caucasian patients has been reported by only one group
(4). Several interacting factors unique to each population might cause the difference between populations. Also, a lack of statistical power, which was related to the small relative risk or the limited number of subjects in the studies, may have affected the results. Further studies with larger numbers of subjects are recommended.