Although the notion that some of the children and adolescents predestined to develop schizophrenia present subtle behavioral and intellectual abnormalities has been described long ago
(29,
30), their prevalence, phenomenology, and pathophysiological significance are far from clear. Studies attempting to clarify the antecedents of schizophrenia have employed one of the following strategies: high-risk studies, birth cohort studies, retrospective studies, and follow-back studies. However, all strategies have inevitable methodological limitations because schizophrenia is a relatively low-incidence disease, and no powerful risk factors for schizophrenia have been identified; a high number of at-risk individuals has to be followed to obtain a small number of patients. As a result, high-risk studies are very expensive, and the results are not suitable to test multiple hypotheses with sufficient statistical power. Birth cohort studies, which draw patients from an epidemiological group, have the advantage of examining the early antecedents of a representative group of individuals who are later diagnosed with schizophrenia. However, like high-risk studies, they are very expensive and, in the end, yield a relatively small number of patients. Also, because these studies are generally not intended to specifically study schizophrenia but all aspects of development
(31), they do not include measurements presumed to be relevant to schizophrenia like the high-risk studies. Studies based on a retrospective assessment of the developmental history of ill individuals are limited by selective recall and by the high prevalence of subtle behavioral and intellectual deviations in the general adolescent population that are retrospectively attributed to the illness. The present study is a follow-back or historical, prospective study. It has the advantage of including an entire national population; hence, it can examine markers predicting vulnerability to the illness with high statistical power. The study was done by merging the Israeli National Psychiatric Hospitalization Case Registry with the Israeli Draft Board Registry, which contains the scores of behavioral and intellectual assessments of male adolescents obtained at ages 16 to 17 years. The specific purpose of the study was to determine if future psychiatric hospitalization caused by schizophrenia could be predicted from the results of the Israeli Draft Board Registry preinduction assessment tests. If sensitive, specific, and reliable tests predictive of psychosis and hospitalization can be developed, it may be possible to treat at-risk individuals very early, perhaps improving the outcome of the illness
(32–
34).
RESULTS
As a group, the individuals destined to develop schizophrenia (N=509) obtained statistically significant lower (worse) scores on all measures than matched nonpatients (N=9,215) and the entire population (all p values were lower than 0.0001).
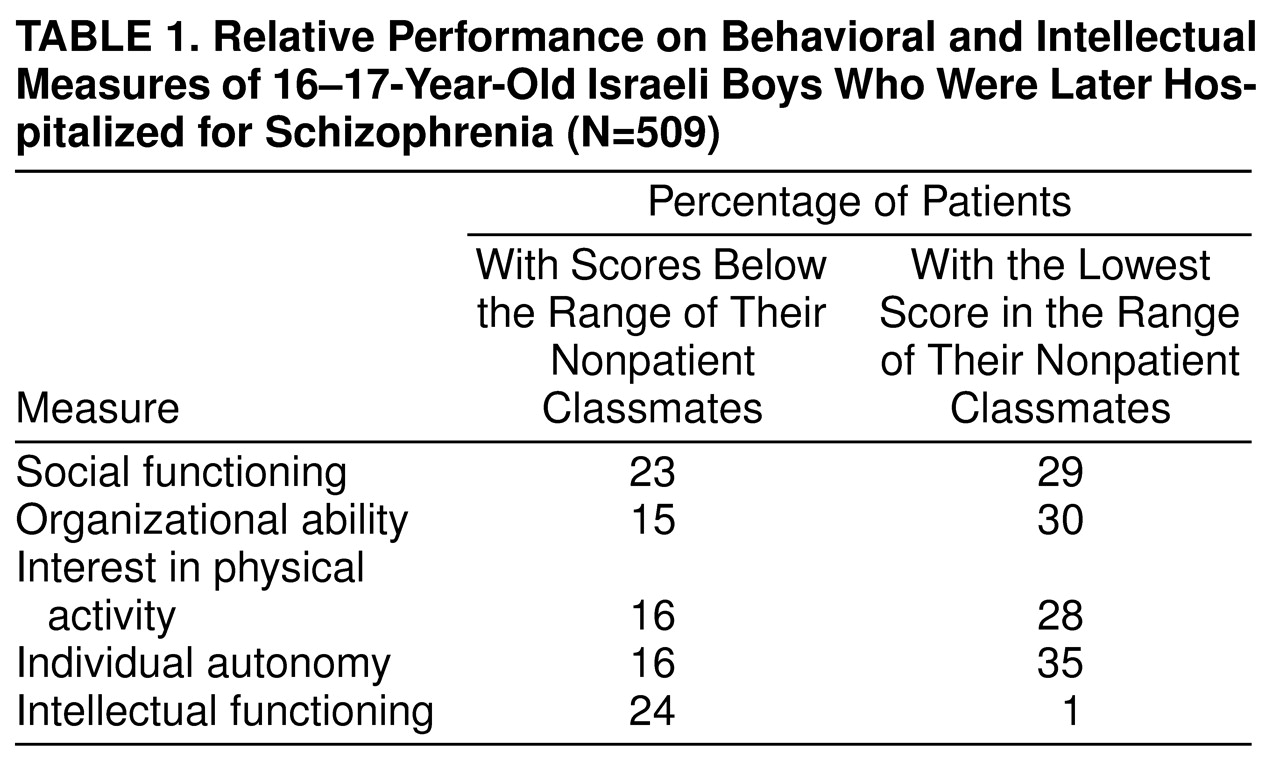
The differences between patients and their respective nonpatients are presented in
Table 1. This table specifies the percentages of patients who performed below the normal range relative to their comparison group (i.e., a comparison to the poorest performance of a healthy individual of the same age attending the same high school) on each measure. As shown, a high proportion of the patients performed below the range of their nonpatient peers. This was most pronounced in social functioning, where 23.2% of the patients performed below the range of their nonpatient classmates and 29.1% performed at the lowest normal range. Thus, 52.3% of the patients had a social functioning score that was equal to or lower than that of their matched nonpatients. This analysis illustrates the power of comparing patients to matched subjects from the same school.
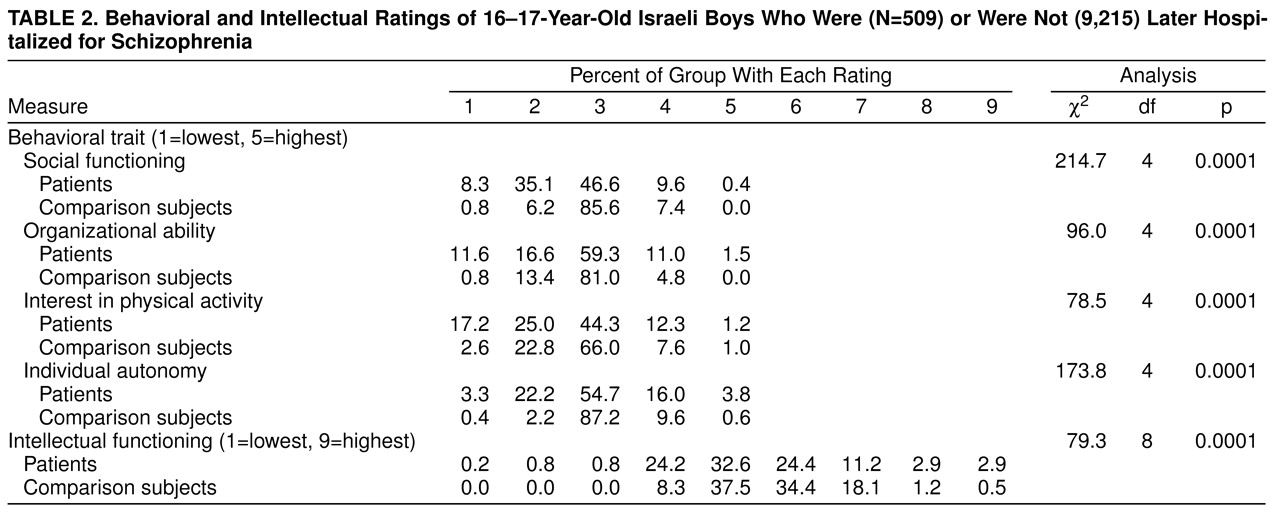
Table 2 presents a comparison of the distribution of all patients to all nonpatients. For this and subsequent analyses, the mean score of the nonpatient matched comparison subjects was used. As shown, there are large and statistically significant differences on all behavioral measures. Again, the most pronounced differences were in social functioning, where 8.3% of patients had the lowest score and 35.1% had the second-to-lowest score, whereas only 0.8% and 6.2% of nonpatients, respectively, had scores in these categories. By using, for example, the social functioning scale alone, with a cut-off point of the lowest two quintiles, one could accurately predict membership in the patient group in 43.4% of the patients (8.3% plus 35.1%) and membership in the nonpatient group in 93.0% (85.6% plus 7.4% plus 0.0%). On the measure of intellectual functioning, which was rescaled into a variable with nine categories, there was also a large and statistically significant difference between patients and nonpatients. Despite the differences, it should be noted that patients performed over the same range as nonpatients.
The combined predictive ability of the four behavioral measures and intellectual functioning were studied by using logistic regression. Using standard logistic regression, we found that the best predictors of future schizophrenia were poor social functioning (Wald χ2=87.9, df=1, p=0.0001; odds ratio=3.22, 95% confidence interval [CI]=2.54–4.13) and lower intellectual functioning (scaled) (Wald χ2=6.5, df=1, p=0.01; odds ratio=1.18, 95% CI=1.04–1.33). Using a cutoff point of 0.7, which best divided the groups, we obtained a sensitivity of 53.1% and a validated specificity of 95.0% (model χ2=129.6, df=2, p=0.0001), with an overall rate of correct classification of 92.8% and a positive predictive value of 36.9%. The positive predictive value was calculated by using the sensitivity and validated specificity values, assuming a prevalence rate of 1% for schizophrenia.
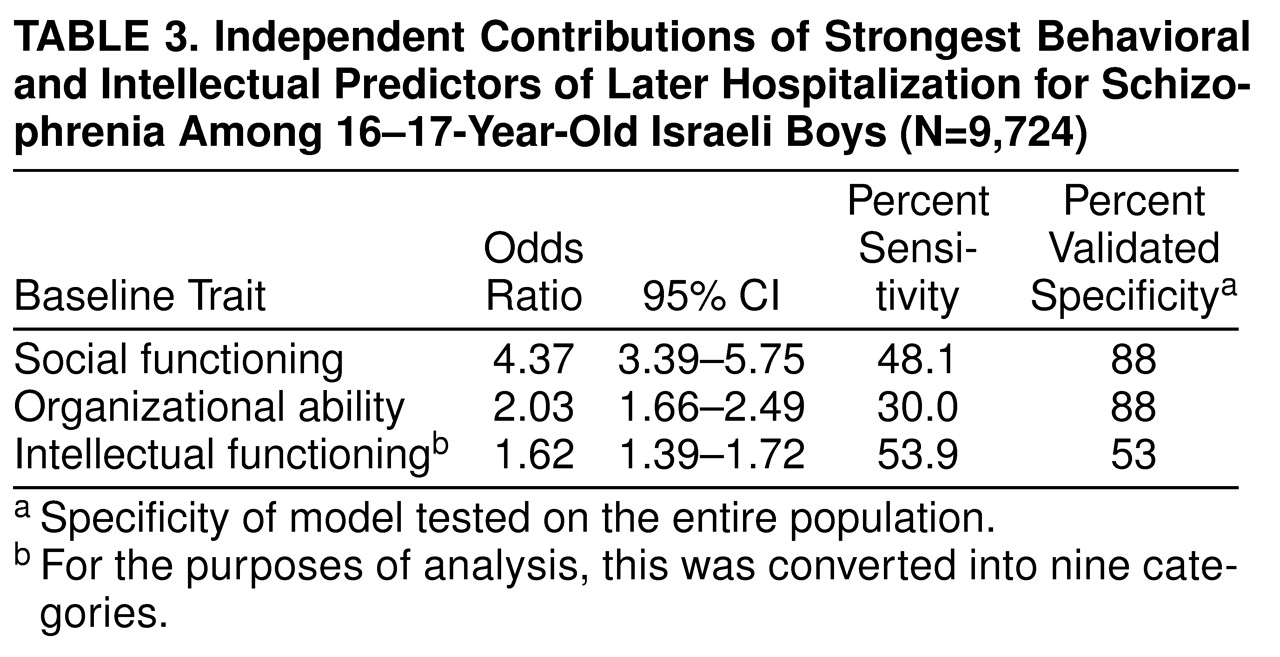
The predictive model was further refined by using conditional logistic regression, which found that the strongest predictors of future schizophrenia were poor social functioning (Wald χ
2=69.2, df=1, p=0.0001; odds ratio=2.9, 95% CI=2.22–3.94), poor organizational ability (Wald χ
2=42.7, df=1, p=0.0001; odds ratio=1.4, 95% CI=1.09–1.81), and low intellectual functioning (scaled) (Wald χ
2=7.5, df=1, p=0.006; odds ratio=1.5, 95% CI=1.30–1.83). With a cutoff point of 0.5, the model had an overall rate of correct classification of 87.5% (sensitivity=75.0%, validated specificity=99.7%, model χ
2=117.1, df=3, p=0.0001) and a positive predictive value of 71.6%. The positive predictive value was calculated by using the sensitivity and validated specificity values, assuming a prevalence rate of 1% for schizophrenia. The independent contribution of each predictor variable is presented in
Table 3.
To further test the model, the study population was randomly divided into two halves, and the same logistic regression procedure was conducted on each half. The resultant regression coefficients were used to classify the other half of the group and vice versa
(43). Both models identified social functioning, organizational ability, and intellectual functioning as the variables best predictive of future schizophrenia. The sensitivities ranged from 74.2% to 75.9%, and specificity was not affected.
Moreover, the model was applied to the entire healthy population, after excluding individuals diagnosed by the draft board preinduction assessment as suffering from a psychiatric illness, subsyndromal psychiatric manifestations, severely abnormal behavior, or mental retardation. This procedure yielded a sensitivity of 74.7%, a specificity of 99.7%, a correct classification of 99.6%, and a positive predictive value of 42.7% (calculated according to the cohort prevalence values).
To test for linearity of the relationship between risk for schizophrenia and test scores, an additional variable was added to the model aimed at assessing departure from linearity
(40). The results indicated that there is a linear relationship between risk of schizophrenia and intellectual functioning (i.e., no significant departure from linearity, Wald χ
2=2.6, df=1, p=0.11) but no linear relationship between risk of schizophrenia and behavioral variables (social functioning: Wald χ
2=25.4, df=1, p=0.0001; organizational ability: Wald χ
2=19.7, df=1, p=0.0001).
To distinguish whether the prediction model identifies future occurrence of schizophrenia in apparently healthy individuals or in individuals already experiencing prodromal symptoms, the data were reanalyzed as a function of the time that elapsed between the draft board testing and the first hospitalization. If the model was identifying prodromal or mildly symptomatic individuals, the model’s predictive ability should differ as a function of time elapsing between testing and hospitalization (i.e., the model’s predictive ability should be better for patients hospitalized closer to the time of testing). To assess this assumption, the group was divided into two on the basis of the median time difference between testing and first hospitalization. The two groups were therefore composed of patients hospitalized 1 to 4 years after testing and patients hospitalized 4 to 10 years after testing. A conditional logistic regression was conducted on each of the groups. There was only a 5% difference in sensitivity between the groups and no difference in specificity, indicating that the model has a similar predictive ability regardless of the time lag between testing and first hospitalization. These results, which suggest no difference between the groups, were further confirmed by comparing the means of the two groups on the predictor variables by using independent group t tests, which revealed no significant differences.