The recently introduced concept of remission criteria for schizophrenia
(1) represents a major opportunity for clinicians and consumers. The proposed remission criteria consist of two components: a symptom-based criterion (low scores on diagnostically relevant symptoms) and a time criterion (duration of 6 months). Using longitudinal data from a local health technology assessment database in a geographically defined area, we attempted validation of the symptom-based criterion in terms of 1) cross-validation with clinician-reported and patient-reported functional outcomes and 2) sensitivity analysis with regard to the exclusion of depression and suicidality from the remission criteria.
Method
Data were collected in a local catchment area (N=250,000) from the local Cumulative Needs for Care Register for patients with severe mental illness, which had been in operation since 1998
(2) . Conforming to current legal requirements, patients were informed that anonymized routine clinical data may be used for the purpose of regional health technology assessment and given the choice to “opt out,” in which case their data were not used. We used the Camberwell Assessment of Need
(3), the Brief Psychiatric Rating Scale (BPRS)
(4), the Global Assessment of Functioning Scale (GAF) split into its psychopathology (GAF symptoms: group range=1–95) and impairment (GAF symptoms, group range=1–95) components
(5), a single item on satisfaction with services (satisfaction), two items on quality of life with housing and social relationships (combined into a single item: social quality of life), and two items on quality of life with physical and mental health (combined into a single item: health quality of life). The Camberwell Assessment of Need, the BPRS, and the GAF were scored by clinicians; satisfaction, social quality of life, and health quality of life were scored by the patient on 7-point Likert scales and have been validated previously
(2) . The number of Camberwell Assessment of Need unmet needs was used in the analysis (group range=0–9).
After the first assessment, the assessments were repeated whenever there was an important change in the treatment plan or, if no such change was present, with intervals of 1 to 2 years. We report here on 317 subjects with a clinical diagnosis of nonaffective psychotic disorder (DSM codes 295, 297, and 298) in the register, who since 1998 had had at least two assessments (median number of postbaseline assessments: 3.0, interquartile range: 2–4; median follow-up: 1,132 days; interquartile range: 521–1,757), and who could be classified at baseline and at least one follow-up according to the symptomatic remission criterion. The median interval between assessments was 462 days (interquartile range: 315–736 days, range: 34–2,034), and this was not associated with whether or not the symptomatic remission criterion was met at the time of the assessment (multiple regression B=18.2, p=0.62). Compared to the other 661 subjects in the register with severe mental illness who were not included in the analyses because of different diagnostic grouping, single assessments only, or missing data at remission, our study group of 317 was similar in terms of Camberwell Assessment of Need unmet needs (multiple regression B=–0.29, p=0.18), GAF psychopathology (multiple regression B=–1.49, p=0.53), and GAF impairment (multiple regression B=–0.94, p=0.67).
The cross-validation assessed whether a change in remission status over time would be associated with important changes in clinician-reported and patient-reported functional outcomes. To this end, the patients were identified who at baseline did (N=145, 46%) and did not (N=172, 54%) fulfill the symptomatic remission criterion according to the seven items of the BPRS
(1) . These two groups were followed up for change in remission status, and those who had changed were compared with nonchanged individuals for change in functional outcomes. For that purpose, regression models were constructed with various functional outcomes (e.g., the number of Camberwell Assessment of Need unmet needs and the social quality of life score) as the dependent variable and remission status (0: not meeting criterion; 1: meeting criterion) as the independent variable, with adjustment for the baseline value of the functional outcome. Because there was more than one observation per individual, compromising the statistical independence of observations, the STATA XTREG multilevel random regression procedure
(6) was used to conservatively adjust standard errors in p values for clustering within individuals. The 317 individuals provided 841 postbaseline observations for the regression analyses, 6% provided one postbaseline observation, 34% two postbaseline observations, 26% three postbaseline observations, and 34% four or more postbaseline observations.
The sensitivity analysis assessed how stable the cross-validation was in terms of changing the remission criterion to include BPRS depression and suicidality. To this end, the same cross-validation analyses were carried out, with the additional requirement of including the BPRS depression and suicidality items in the symptomatic remission criterion (extended symptomatic remission criterion).
Results
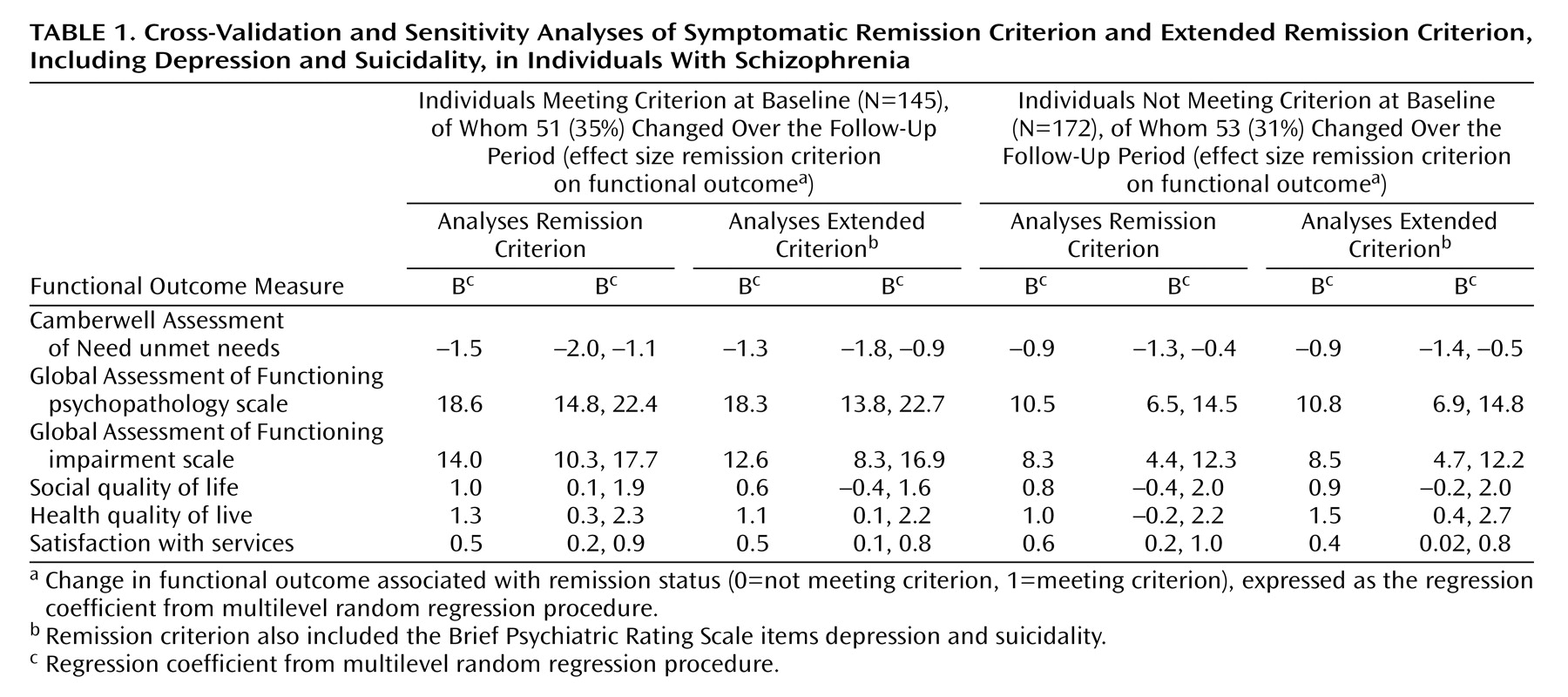
Of the 145 patients who did fulfill the symptomatic remission criterion at baseline, 35% moved out of remission over the follow-up. Conversely, of the 172 patients who did not fulfill the symptomatic remission criterion at baseline, 31% moved into remission. For the extended symptomatic remission criterion, including BPRS depression and suicidality, these rates were, respectively, 37% of the 120 patients meeting the criterion at baseline and 29% of 193 patients not meeting the criterion. Associations between change in remission status in the two groups and functional outcomes are summarized in
Table 1 . For both the group that did and the group that did not meet the symptomatic remission criterion at baseline, change in remission status was associated with strong differences in functional outcome compared to group members who did not change. For example, in meeting the symptomatic remission criterion at baseline, remaining in remission was associated with adjustment for any baseline differences, with 1.5 unmet needs less than the group that moved out of symptomatic remission, as well as nearly 20 points more on the GAF psychopathology scale and 14 points more on the GAF impairment scale. Similarly, for those not meeting the criterion at baseline, moving into symptomatic remission was associated—with adjustment for any baseline differences—with around one unmet need less than the group that did not move into symptomatic remission, as well as nearly 11 points more on the GAF psychopathology scale and 8 points more on the GAF impairment scale. Similar differences were apparent for the patient-reported functional outcomes. Changing the remission criterion to include the BPRS items of depression and suicidality did not introduce large or consistent changes to the results.
Of the patient-reported outcomes, satisfaction with services was sensitive to change in remission status, whereas quality of life outcomes appeared to be somewhat less sensitive.