Metabolic syndrome is a collection of risk factors that are associated with increased morbidity and mortality due to cardiovascular disease
(1) . Schizophrenia has long been associated with elements of the metabolic syndrome, and numerous studies have found increased mortality because of cardiovascular disease
(2 –
4) . Several possibilities have been suggested to explain these associations in schizophrenia, including poor diet, lack of exercise, cigarette smoking, and stress, as well as abnormalities of the hypothalamic-pituitary-adrenal axis
(5 –
7) .
In recent years, treatment with antipsychotic medications has been recognized as an additional risk factor for the development of metabolic abnormalities
(8) . Clozapine was approved by the Food and Drug Administration in 1989, yet it remains the only antipsychotic medication with established efficacy in treatment-resistant schizophrenia patients
(9) . Despite its efficacy, growing evidence suggests that clozapine has a substantial effect on metabolic parameters. In a meta-analysis of over 80 studies examining weight gain
(10), clozapine treatment was associated with an average gain of 9.8 lb over 10 weeks—the most of any antipsychotic drug. More case reports of clozapine-associated glucose abnormalities have been submitted to the Food and Drug Administration
(11) and published
(12) than for any other antipsychotic drug. Reports have also associated clozapine treatment with the development of hypertriglyceridemia
(13), increased total cholesterol levels
(14), and hypertension
(15) .
The purpose of this study was to assess the prevalence of the metabolic syndrome among a group of outpatients receiving clozapine. The National Cholesterol Education Program’s definition of the metabolic syndrome was chosen for our study purposes because of its ease of use in clinical practice
(16) . The National Cholesterol Education Program’s fasting glucose cutoff level was updated to reflect the American Diabetes Association’s new cutoff point of 100 mg/dl
(17) . With these criteria, the metabolic syndrome is defined as having three or more of the following: a waist circumference >102 cm for men and >88 cm for women; a fasting blood triglyceride level ≥150 mg/dl; a high-density lipoprotein cholesterol level <40 mg/dl for men and <50 mg/dl for women; blood pressure of ≥130 mm Hg systolic or ≥85 mm Hg diastolic; and a fasting blood glucose level of ≥100 mg/dl.
Method
Outpatients receiving clozapine for at least 6 months at the University of Rochester Medical Center Department of Psychiatry were approached for study participation. After they received a complete description of the study, written informed consent was obtained. This study was approved by the University of Rochester Medical Center Research Subject Review Board. Ninety-three outpatients consented to participate in the study. Pharmacy and medical records were reviewed to obtain demographic, clinical, and drug treatment data. To examine whether use of adjunctive agents poses additional risk for metabolic abnormalities, co-prescription data were gathered from pharmacy records for analysis.
The subjects subsequently received blood pressure and waist circumference measurements. Waist circumference was measured midway between the lowest rib and the iliac crest with the subjects standing using a tape with a spring-loaded mechanism to standardize tape tension during measurement. Smoking status was assessed at the time of measurement on the basis of a “yes/no” question: “Have you smoked within the past year?” Family history of diabetes was also assessed at the time of measurement on the basis of subject reports of any first-degree relative with diabetes. A history of diabetes for each subject was determined by a review of medical records. Subjects without a documented history of type 1 or type 2 diabetes received a fasting blood glucose test. The subjects diagnosed with diabetes before study enrollment were scored as satisfying the fasting blood glucose level criterion of ≥100 mg/dl. All subjects received a fasting blood lipid profile, including triglyceride, total cholesterol, and high-density lipoprotein measures.
For comparison purposes, a matched comparison group was drawn from the most recent version of the National Health and Nutrition Examination Survey (NHANES). NHANES is a federally sponsored database containing detailed health information about 11,039 Americans. A matched group of 2,701 individuals was selected for comparison purposes. The group was matched for age (between 17 and 55 years old), body mass index (≥19 kg/m 2 ), and race/ethnicity (white, African American, Hispanic American, or “other”). Rather than selecting the NHANES comparison subjects to match each clozapine subject based on the covariates, the effects of the covariates were controlled by performing analyses based on subgroups stratified covariates. This approach enabled the use of all available comparison subjects from the NHANES database to increase statistical power.
Logistic regression analyses were performed to determine if study variables were associated with the presence or absence of metabolic syndrome. In addition, appropriate interactions were added to the logistic models to examine whether differential associations existed among the variables between the two subject groups. We used t tests to determine whether continuous variables, such as years of clozapine treatment, were associated with the metabolic syndrome. Chi-square analysis was employed for testing the associations of categorical variables, such as the use of bendzodiazepines, antidepressants, and mood stabilizers. All tests performed were two-sided, with a significance level of alpha=0.05 unless otherwise noted.
Results
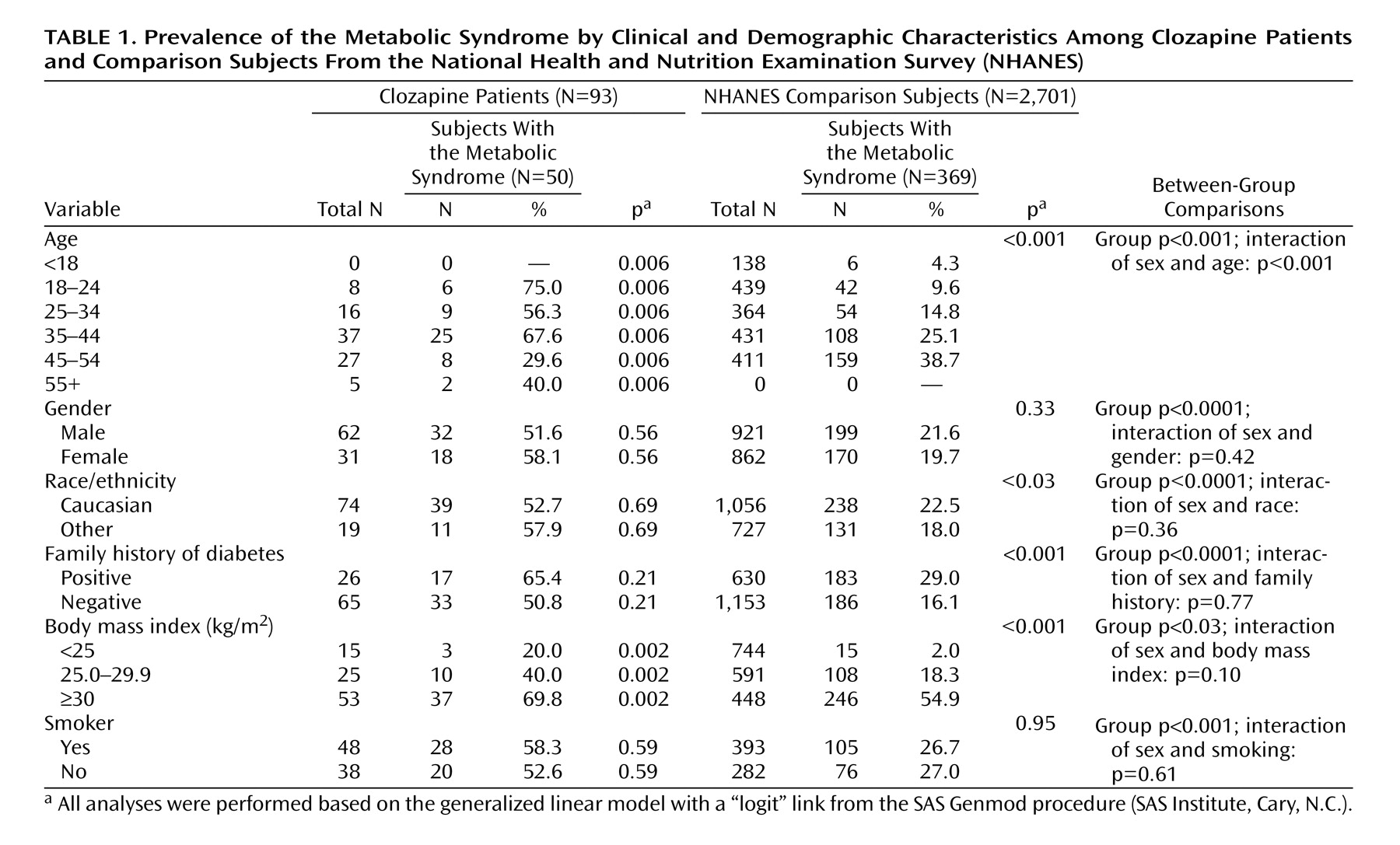
The mean age of the clozapine subjects was 34.4 years (SD=8.7), and 66.7% were men (
Table 1 ). For race/ethnicity, 74 (79.6%) were Caucasian, 15 (16.1%) were African American, two (2.2%) were Hispanic, and two (2.2%) were “other.” The mean body mass index was 31.9 kg/m
2 (SD=7.5). All subjects received a DSM-IV clinical diagnosis of either schizophrenia (N=60, 64.5%) or schizoaffective disorder (N=33, 35.4%) from their treating psychiatrists. A positive family history of diabetes was noted in 26 (28.0%) subjects. The subjects had received an average dose of clozapine of 432.5 mg/day (SD=164.9) for an average duration of 5.9 years (SD=3.6). The mean total duration of exposure to antipsychotic drugs was 15.7 years (SD=8.0).
Within the NHANES comparison group, the mean age of the subjects was 33.5 years (SD=11.9), and 47.9% were men. For race/ethnicity, 1,580 (58.5%) were Caucasian, 813 (30.1%) were African American, 170 (6.3%) were Hispanic, and 138 (5.1%) were “other.” The mean body mass index for the NHANES subjects was 27.8 kg/m
2 (SD=6.5), and 992 subjects (36.7%) had a positive family history of diabetes (
Table 1 ).
A total of 50 (53.8%) clozapine patients met criteria for the metabolic syndrome, compared to 369 (20.7%) subjects within the NHANES group (χ 2 =47.84, df=1, p<0.001). Given the high proportion of subjects with a body mass index less than 25 kg/m 2 in the NHANES group, a secondary analysis was conducted of the NHANES group, excluding the subgroup with a body mass index of <25 kg/m 2 . The prevalence of metabolic syndrome among NHANES subjects with a body mass index of ≥25 kg/m 2 was 34.1%, a rate that remained significantly lower than that of the clozapine group (χ 2 =20.03, df=1, p<0.001).
As shown in
Table 1, significant associations were found between the presence of the metabolic syndrome and both age (p<0.001) and body mass index (p<0.0001) in the clozapine group. Also, a marginally significant association was found with duration of clozapine treatment (χ
2 =3.50, df=1, p=0.06). No association was found with the use of adjunctive medications, smoking, or other clinical or demographic variables. Within the NHANES group, age, race/ethnicity, family history, and body mass index were significantly associated with the presence of metabolic syndrome (age: χ
2 =136.34, df=1, p<0.0001; race: χ
2 =5.34, df=1, p=0.02; family history: χ
2 =40.43, df=1, p<0.0001; body mass index: χ
2 =282.67, df=1, p<0.0001).
When we compared the prevalence rates of metabolic syndrome with respect to clinical and demographic variables, age was noted to have a differential effect on the prevalence rates between the two groups (χ
2 =136.34, df=1, p<0.0001). However, this finding became nonsignificant when the duration of clozapine exposure was controlled in the analysis (χ
2 =3.13, df=1, p=0.08). NHANES subjects missing pertinent data were excluded from the respective analyses, resulting in data from a group of less than 2,701 appearing in
Table 1 .
Discussion
To our knowledge, this report presents the first controlled study of the prevalence of metabolic syndrome among patients receiving clozapine treatment. Comparison with a matched NHANES sample demonstrated that patients receiving clozapine have significantly higher rates of the metabolic syndrome than the general population. However, comparisons with patients taking other antipsychotic medications is not possible because individual prevalence rates associated with specific antipsychotic drugs have not been published to date. Despite the high prevalence rate noted in this study, the study did not allow determination of the degree to which clozapine was responsible. Study limitations include the lack of a nonmedicated schizophrenia control group, a lack of random assignment, and a lack of longitudinal follow-up. NHANES data are also subject to sampling errors, as well as errors associated with the use of self-report data, although NHANES maintains high data integrity standards to minimize such errors.
The high prevalence of the metabolic syndrome in this study has serious long-term health implications. Based on the analysis by Lakka et al.
(1), patients with the metabolic syndrome in this study would be expected to have a two- to threefold increase in cardiovascular disease mortality and a twofold increase in all-cause mortality. This increased risk must be balanced with the potential benefits of clozapine. In addition to its superior efficacy for patients whose disease is refractory to conventional antipsychotic drugs, clozapine is currently the only medication approved by the Food and Drug Administration for the treatment of suicidal behavior. A modeling study calculated that wider use of clozapine could save an average of 53 lives per year worldwide
(18) . Large-scale epidemiological studies are necessary to determine the long-term impact of clozapine on morbidity and mortality in schizophrenia.
Many adults with schizophrenia receive little or no medical care. Such care is important, given the risk of metabolic abnormalities associated with schizophrenia itself and with antipsychotic medications in general
(2,
5,
8) . In response to these issues, current schizophrenia treatment guidelines recommend regular monitoring of body mass index, lipid levels, fasting blood glucose levels, and blood pressure
(8) . Regular monitoring may be especially critical for patients taking clozapine, given the high prevalence of metabolic abnormalities reported in this study and others.