Efficacy of Antidepressants in Bipolar Depression
The management of bipolar depression can be challenging. Antidepressants may be useful for short-term management of the depression, but their use over extended periods is controversial. It is not at all clear that antidepressants have a beneficial long-term therapeutic or prophylactic effect against depression in patients with bipolar illness, and antidepressant treatment may be associated with manic induction, cycle acceleration, and chronic irritable dysphoria.
There is evidence that antidepressants can be useful in brief treatment (that is, 4–10 weeks) of bipolar depression. In a review and meta-analysis of randomized, controlled studies of short-term antidepressant treatment for bipolar depression, Gijsman et al.
(1) found that symptoms were nearly twice as likely to improve in patients who received an antidepressant (fluoxetine, paroxetine, imipramine, or a monoamine oxidase inhibitor) than in those who received placebo or a mood stabilizer alone (lithium or olanzapine) (odds ratio=1.86; 95% confidence interval=1.49–2.30). Lithium alone, used aggressively (at blood levels ≥0.8 mM), was equal in efficacy to lithium used at low levels along with an antidepressant
(2) . Post hoc subanalyses of data from studies of major depression performed in the DSM-III era, when type II bipolar illness was diagnosed as major depression, also found that monotherapy with fluoxetine or venlafaxine was effective in treating depression associated with type II bipolar illness
(3,
4) . The response rates (defined as ≥50% improvement) in these studies were similar to those in studies of unipolar depression (63% for fluoxetine and 48% for venlafaxine).
The APA Practice Guideline for the Treatment of Patients With Bipolar Disorder
(5) does not recommend monotherapy with an antidepressant for bipolar depression. The guideline indicates that although combination therapy with lithium and an antidepressant may be appropriate in some circumstances, lithium or lamotrigine should be considered the first-line options for treatment of acute depression in a patient with bipolar disorder. This recommendation is supported by a more recent study of patients who had treatment-resistant bipolar depression that did not respond to combination therapy with an antidepressant and a mood stabilizer
(6) ; in these patients, the addition of lamotrigine was more effective than the addition of risperidone or inositol. In two placebo-controlled trials
(7,
8), lamotrigine was found to have significant efficacy. In several small controlled studies, lithium was shown to be more efficacious for bipolar depression than no treatment
(9) . Carbamazepine was found to be significantly better than placebo in a small controlled crossover trial
(10), and divalproex was found to be significantly more effective than placebo in a recent small controlled study
(11) . All of these studies support the Expert Consensus Guideline recommendation of optimizing treatment with lithium and anticonvulsants before using antidepressants
(12) .
Although atypical antipsychotics do not figure prominently in the guidelines on treatment of bipolar depression, there is some evidence that they may be useful. Although risperidone was found to be less effective than lamotrigine for treatment-resistant depression
(6) and olanzapine had a small effect size
(13), in one study, quetiapine had a large and significant effect on bipolar depression
(14) .
Adequate treatment of the depression is important. Perlis et al.
(15), studying a large cohort of patients with bipolar disorder (N=1,469) over a 2-year follow-up period, found that the biggest predictor of relapse was residual symptoms, and the majority of relapses were into depression (34.7% of the cohort, compared with 13.8% into mania or hypomania).
Long-Term Use of Antidepressants in Bipolar Disorder
For major depressive disorder, the standard of care is to continue antidepressant treatment as long as the risk of relapse is high. Although this standard has also been applied clinically to patients with bipolar depression, the evidence does not support this practice. The available evidence suggests that antidepressants do not generally have long-term preventive benefits in bipolar depression. Six double-blind randomized clinical trials have examined prophylaxis in bipolar disorder with antidepressants, all comparing imipramine with placebo or lithium. In all cases, imipramine alone or added to lithium was not more effective than lithium alone in preventing mood episodes. A review of randomized clinical trials
(16) examining the long-term efficacy of antidepressants—all of them tricyclics—found that they were not effective in prophylaxis for bipolar disorder.
The long-term effects of the newer antidepressants have been examined in two as-yet-unpublished randomized clinical trials. Researchers in the Stanley Foundation Bipolar Network randomly assigned depressed bipolar patients (N=127) to receive venlafaxine, bupropion, or sertraline in addition to standard mood stabilizers (R. Post et al., unpublished 2004 paper). In the overall results, similar proportions of patients in each treatment group had acute responses to the antidepressants (53.2%–59.7%), but those in the venlafaxine group experienced more manic or hypomanic switches (15.1%, compared with 5.4% with bupropion and 6.7% with sertraline). Remission without any manic switch at 1 year occurred in 17.9% of patients taking venlafaxine, 27.4% of those taking sertraline, and 38.1% of those taking bupropion. In a fraction of patients who achieved and maintained euthymia for 2 months (15%–20% of the initial combined cohort of 384 patients in two separate long-term studies [
17,
18 ]), continuation of antidepressants was associated with a lower risk of relapse into depression (35%–36% in the two studies), compared with discontinuation of the antidepressants (68% and 70%). This subanalysis was not randomized, however; the decision to stop or continue antidepressant treatment was naturalistic, and thus the generalizability of these findings is unclear.
In a second ongoing randomized trial
(19), patients who were experiencing recovery with a mood stabilizer plus an antidepressant for acute bipolar depression underwent open random assignment to continue or discontinue the antidepressant while staying on the mood stabilizer. An interim analysis of the 66 patients recruited into the study at the time suggests that there is no added benefit to remaining on antidepressants for long-term treatment. In a subgroup analysis, patients with rapid-cycling bipolar disorder who continued antidepressant treatment had greater depressive morbidity at 1-year follow-up than those who discontinued antidepressants.
In the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD), a large naturalistic study, an initial analysis of 33 patients who received antidepressants for an episode of depression and were followed prospectively over 12 months showed no benefit to continuing antidepressants
(20), and time in remission did not differ from that of patients who discontinued antidepressants (T.B. Pardo et al., unpublished 2004 paper). Among patients who discontinued antidepressants, the risk of depressive relapse was not increased
(20) . This subanalysis, like the Stanley Foundation subanalysis mentioned above
(18), was a nonrandomized, naturalistic study. Unlike in the Stanley Foundation analysis, however, in the STEP-BD analysis the data were adjusted for potential confounding factors, such as history of rapid cycling.
Thus, in all randomized trials conducted thus far, there is no evidence that continuing treatment with antidepressants can prevent depression. In naturalistic trials, a small fraction of patients (usually less than 20%) may benefit from ongoing antidepressant treatment.
The APA practice guideline does not directly address the issue of continuation treatment with antidepressants. The best studies with an adequate design and sample size examining long-term use of pharmacologic agents in relapse prevention are those in which lamotrigine has been investigated. Since the risk of developing a depression is greater if the most recent bipolar episode is a depressive one
(21), the most meaningful studies may be those that examine patients who have had a recent episode of depression. Calabrese et al.
(22) compared lamotrigine and lithium monotherapy and placebo for relapse prevention in 463 patients with bipolar I disorder who had experienced a recent depression. They found that lamotrigine was superior to placebo in terms of delaying the onset of another depression and in duration of a depression-free period. While lamotrigine was not significantly superior to lithium, lithium’s depression prevention effect also did not separate from placebo.
Antidepressants in Children and Adolescents
Psychopharmacologic management of bipolar disorder in children and adolescents poses a greater challenge than in adults. There is little evidence-based research on the use of antidepressants for pediatric bipolar disorder. However, these patients first present with symptoms characteristic of major depression, and often the initial treatment is antidepressant therapy. Geller et al.
(35,
36) followed 79 children (average age at recruitment into the study, 10.2 years [SD=1.6], followed 2-5 years) who had a diagnosis of major depressive disorder and found that 32% had switched to mania by an average age of 11 years (80% of them prepubertal) and 50% by the age of 21 years. Cicero et al.
(37) found in a retrospective chart review of children with bipolar disorder that the diagnosis was made 2 years earlier on average in those who were treated with antidepressants than in those who were not. However, this finding may simply indicate that in children with bipolar disorder who present with an initial episode of depression, the onset of bipolar illness occurs at an earlier age.
Summary
For patients such as the woman featured in the vignette, there is little evidence to support continued antidepressant treatment. Rather, the evidence from the literature suggests that, for this patient, the antidepressant may be contributing to her current dysphoria and middle insomnia. The stronger clinical trials in the literature support the use of lamotrigine
(8,
9), lithium
(7), carbamazepine
(10), and valproic acid
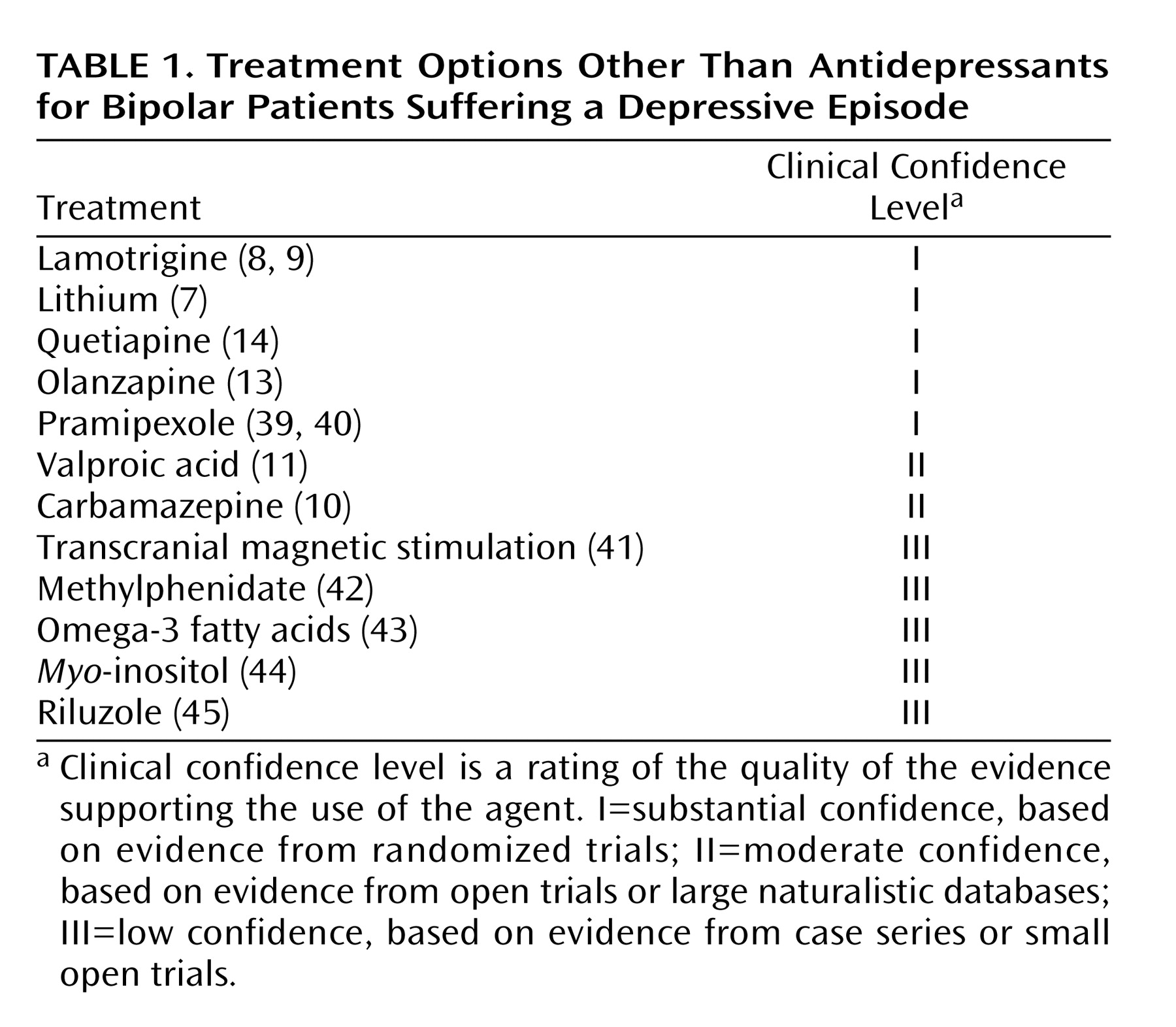
(38), in that order. Additional treatment options are presented in
Table 1, although for some of these, long-term safety and efficacy data are not yet available. In the case presented, I would recommend slowly tapering the antidepressant while making sure that the patient receives an adequate dosage of one of these mood stabilizers. If she develops another episode of depression while being treated with a mood stabilizer, antidepressant therapy could be briefly reinitiated.