Increasing recognition is being given to the public health burden of violence
(1) . Every year, over half a million people die from interpersonal violence, nearly double that from armed conflict
(2) . It is the sixth leading cause of death among people ages 15–44
(3) . In addition, many more people survive acts of violence than die from them and suffer physical injury and psychological consequences. Consequently, violence is estimated to be among the 20 leading causes of disability-adjusted life years worldwide
(4), and its contribution to worldwide disability is projected to increase in the next two decades
(5) . Evidence suggests that among the potentially modifiable risk factors for violent crime is severe mental illness. Studies of birth cohorts in Scandinavia
(6 –
8) and New Zealand
(9), psychiatric case registers in Australia
(10 –
12) and the United Kingdom
(13), and discharged psychiatric patients in the United States
(14) have indicated that psychoses are modest risk factors for violent offending. This research has estimated that the risk of an individual with psychosis committing a violent offense compared with a general population group of a similar age is between two and six times for men and two and eight times for women.
However, previous research has estimated the probability that an individual with a severe mental illness receives any violent conviction, not accounting for an individual repeat offender or the number of different crimes that make up a single conviction. In addition, and more important from a public health perspective, focusing solely on relative risk does not account for the absolute base rate of these crimes and gives an incomplete picture of the dangerousness of those with severe mental illness. Risk estimates underestimate the population impact of these patients to violent crime if individuals with severe mental illness offend more frequently than the general population. In support, recent evidence from Australia
(11) suggests that offenders with schizophrenia have two times more convictions over their lifetime than offenders without schizophrenia when matched for age and neighborhood. If, on the other hand, they offend less frequently, the relative risk will exaggerate the population impact. To clarify this issue, calculating the population-attributable risk of severe mental illness to violent crime—the proportion of violent crimes that can be attributed to individuals with severe mental illness—is necessary
(15) . By analogy, it is known that the relative risk of developing lung and pancreatic cancers is significantly higher in smokers, but the population-attributable risk of smoking differs substantially between them. It is estimated at 90% for lung cancer, but for pancreatic cancer, it is 33% because of the contribution of other risk factors, such as alcohol use
(16) .
In order to empirically investigate the population impact of severe mental illness on violent crime, we examined data from high-quality national hospital and crime registers in Sweden covering the period 1988–2000. We calculated the population-attributable risk: the number of violent crimes committed per 1,000 persons in the whole population that would not have occurred if the risk factor—severe mental illness—had been absent, and the population-attributable risk fraction, which is the proportion of violent crimes in the whole population that may be attributed to individuals with severe mental illness. Because the population impact was the focus of the study, we included all categories of violent crime—not just homicide—which is a relatively rare event compared to other types of violent crime. We discuss these findings in light of the assumption of these methods that there is a causal relationship between risk factor and outcome.
Results
Patient Characteristics
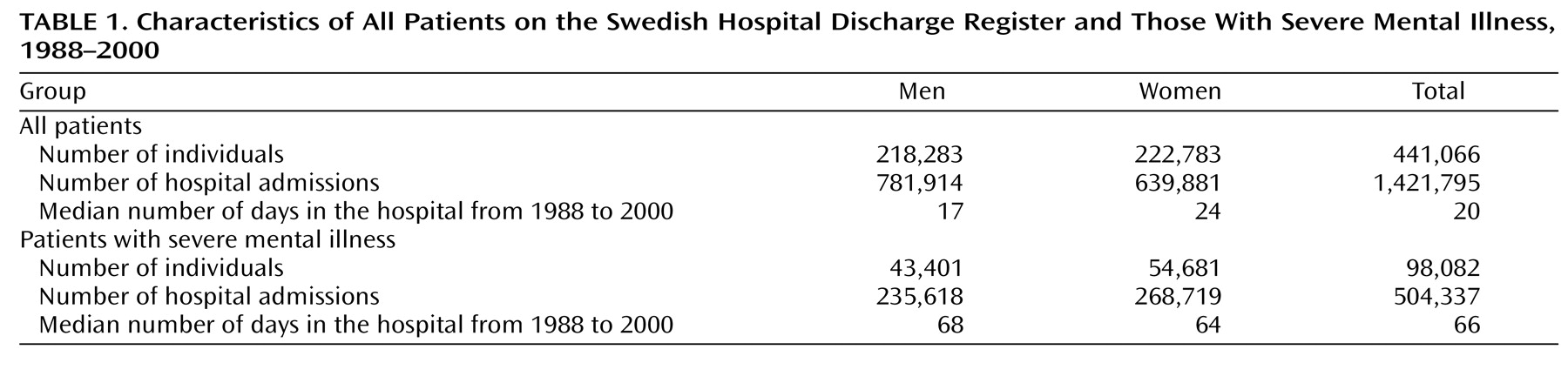
During the period 1988–2000, 98,082 patients with severe mental illness, or 1.4% of the general population, were discharged from the hospital (55.8% women) (
Table 1 ). These individuals were admitted to the hospital 504,337 times, with 5.1 admissions on average (SD=7.5, median=3, mode=1, range=1–184). The number of individuals with severe mental illness who committed at least one violent crime over the time period was 6,510. Therefore, of all patients with severe mental illness, 6.6% had a violence conviction. This compared with 130,421 individuals, or 1.8% of the general population, who had a violence conviction (
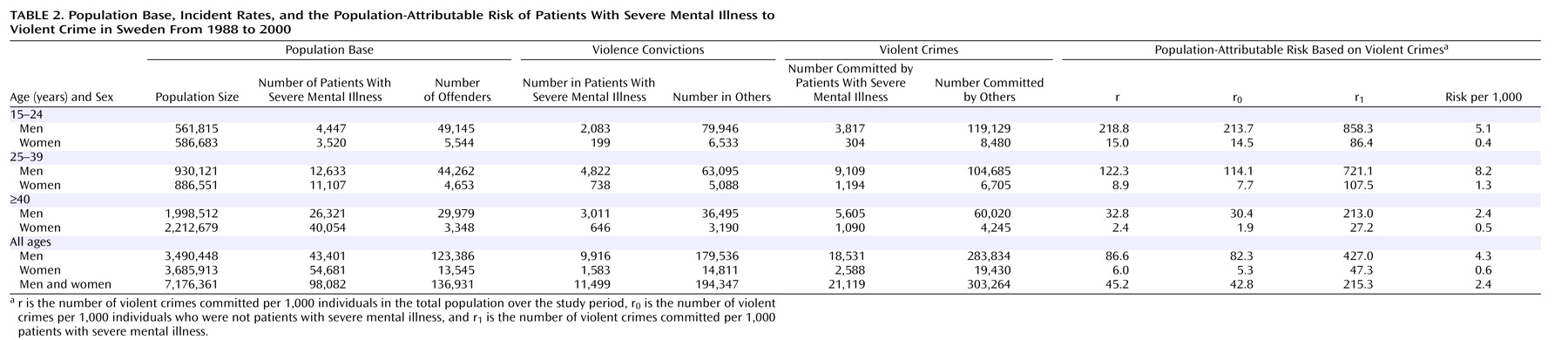
Table 2 ).
Those with severe mental illness committed 21,119 individual counts of violent crime (3.2 violent crimes per convicted individual with a severe mental illness) compared with 303,264 counts of violent crime in the general population (2.3 violent crimes per convicted individual in the general population). Among patients and others who offended, the pattern of repeat offending was similar: 19.4% of patients (N=1,266) were convicted on two or more occasions, compared with 15.6% (N=21,356) of the general population; 0.3% of all patients (N=21) were convicted at least 10 times compared with 0.1% (N=118) of the general population.
Odds Ratios
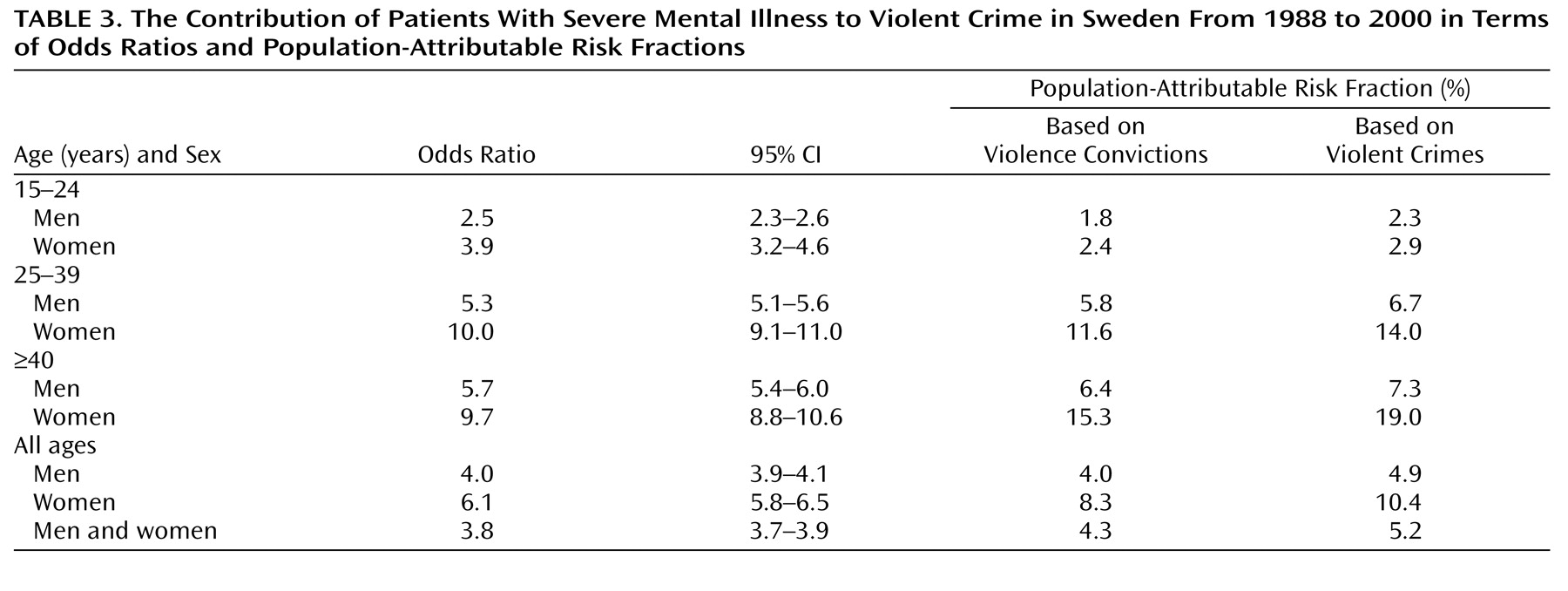
The overall crude odds ratio for patients with severe mental illness for violent convictions during the period 1988–2000 was 3.8 (95% CI=3.7–3.9). The odds ratio was higher in women than in men and higher in those 25 years and older than in those 15–24 years old (
Table 3 ).
Population-Attributable Risk
Forty-five violent crimes per 1,000 inhabitants were committed during 1988–2000. In comparison, 215 violent crimes were committed per 1,000 patients with severe mental illness. For those who had never been hospitalized with a diagnosis of severe mental illness, 43 violent crimes were recorded per 1,000 individuals. The population-attributable risk for patients with severe mental illness was 2.4, and the population-attributable risk fraction was 5.2%. In other words, patients with severe mental illness, as identified by hospital admissions, committed about 5% of all violent crimes.
Population-attributable risk fractions were calculated by age band and gender (
Table 3 ). The population-attributable risk fraction for both genders was lower in the 15–24 age band than in the older age bands. Six violent crimes were committed per 1,000 women in the general population, of which 0.6 could be attributed to patients with severe mental illness. Women with severe mental illness committed about one-ninth of the violent offenses than the men with severe mental illness (47 violent crimes per 1,000 female patients versus 427 violent crimes per 1,000 male patients). Women had higher population-attributable risk fractions compared with men, particularly for those ages 25–39 years and those 40 and over. The population-attributable risk fraction for women ages 40 and over was 19%.
We also calculated the population-attributable risk fraction by looking at the proportion of violent convictions (rather than individual counts of violent crime) that could be attributed to patients with severe mental illness (
Table 3 ). The population-attributable risk fraction was 4.3%. We also calculated the population-attributable risk fraction by looking at the proportion of violent criminals who were patients with severe mental illness. The population-attributable risk fraction was 4.8%. Because these two alternate methods of calculating the population-attributable risk fraction were not materially different from using individual counts of violent crime, subsequent analyses focused on individual counts of violent crime.
Schizophrenia and Other Psychoses
For schizophrenia, the crude odds ratio was 6.3 (95% CI=6.1–6.6), and for other psychoses, it was 3.2 (95% CI=3.1–3.3). We calculated the population-attributable risk and the population-attributable risk fraction for these patients. A total of 26,663 individuals were discharged from the hospital with schizophrenia, and 71,419 individuals were discharged with other psychoses. The number of violent crimes committed was 328 per 1,000 patients with schizophrenia and 173 per 1,000 patients with other psychoses. The population-attributable risk for patients with schizophrenia to violent crimes was 1.0 (out of 45) per 1,000 inhabitants in the population, and for other psychoses, it was 1.4. This corresponded to a population-attributable risk fraction of 2.3% for patients with schizophrenia and 2.9% for patients with other psychoses.
Thus, these population-attributable risk fractions and odds ratios point in different directions. Although the odds ratio was higher for those with schizophrenia than for those with other psychoses, the attributable risk fraction was higher for those with other psychoses.
Offense Type
Population-attributable risk fractions were broken down by category of offense. Higher population-attributable risk fractions were found for homicide and attempted homicide (18.2%) and arson (15.7%). Population-attributable risk fractions for threats and harassment was 7.5%; for assaulting an officer, 6.8%, for aggravated assault, 6.3%; sexual offenses, 4.9%; robbery, 3.6%, and common assault, 3.1%.
Discussion
This study calculated the population-attributable risk and attributable risk fraction of patients with severe mental illness in relation to violent crime. It did so by linking high-quality national databases for hospital discharges and violent convictions in Sweden, involving 98,082 patients who committed 21,119 crimes. Over a 13-year period, 45 violent crimes were committed per 1,000 inhabitants, of which 2.4 were attributable to patients with severe mental illness. This corresponded to a rate of approximately one violent crime per 1,000 inhabitants every 5 years that could be attributed to patients with severe mental illness. The attributable risk fraction of these patients to violent crime was 5.2%. Assuming that there is a causal relationship between severe mental illness and violent crime, one way of interpreting this attributable risk fraction is that violent crime would have been reduced by 5.2%, if, hypothetically, all those with severe mental illness had been institutionalized indefinitely.
This study has a number of limitations. First, we defined patients with severe mental illness by their status as inpatients. There were individuals with such illnesses who were not admitted to the hospital, although in Sweden, this is unlikely to exceed 10% of such patients
(25,
26) . Studying inpatients only, however, has the advantage of specificity and allows for estimation of the potential impact of any interventions. Second, this investigation has defined violent crime by officially recorded conviction data. Although this avoids the reporting biases associated with self-report and informant questionnaires for violence, it is an underestimate of the extent of violent behavior in society
(14) . However, the Dunedin Study
(9) found that this underestimate did not alter the odds ratios for violent behaviors in those with psychiatric disorders because the amount of violence underestimated was similar among those with psychiatric disorders and those without such disorders. A particular advantage of using Swedish conviction data is that it includes individuals who are sentenced by the court to psychiatric hospitals and who are cautioned or fined. In addition, Swedish data are not affected by plea bargaining, which can alter the final recorded conviction in some legal systems. Third, the method of population-attributable risk assumes causality. However, the relationship between severe mental illness and crime is more complex than simple causality, and nonmodifiable risk factors, such as age, gender, socioeconomic status, and previous criminality are important, as are other potentially treatable factors such as substance abuse, personality disorder
(27,
28), and medication compliance
(29) . Comorbid substance abuse, in particular, increases the risk of violent crime in those with severe mental illness
(8,
11,
14) . However, because substance abuse and severe mental illness are not independent of each other, we did not calculate the attributable risk separately for those with and without comorbidity because the focus of this study was the attributable risk of patients with severe mental illness, not of the psychosis itself.
This approach makes no assumptions about the timing of the offense. This means that individuals who were hospitalized after the offense occurred are included in population-attributable risk estimates. Although it is reasonable to assume that the severe mental illnesses that were included in this study are mostly lifelong, this might overestimate the contribution of severe mental illness to violent crime. But it may also underestimate the contribution because it assumes that all those with severe mental illness have been admitted to the hospital over a 13-year period. The chronicity of these conditions argues for the approach of population-attributable risk because including only the patients whose diagnoses preceded the offense misses significant numbers of individuals who were first diagnosed after assessment by forensic psychiatric services. This study did not estimate the unique contribution of psychotic symptoms to violent crime or examine the possible mechanisms of offending, but rather, it addressed from a public health perspective the potentially more relevant issue of the attributable risk of patients with severe mental illness. Calculation of the attributable risk for psychotic symptoms would require further adjustment by potential confounders, which would further reduce the risk of violence uniquely attributable to severe mental illness. A final possible limitation is the generalizability of this data to other countries. Although Sweden is average for Western Europe in terms of the rate of violent crime per head of population, it has lower rates of homicides (around 100 homicides per year in a population of 9 million) than countries with more liberal gun ownership laws, such as the United States. This will alter the attributable risk for homicide, which is likely to be lower in countries such as the United States, but it is unlikely to substantially modify the overall attributable risk for violent crime, which is mostly accounted for by much more common crimes, such as assault.
Population-attributable risk is not directly relevant to estimating the dangerousness of individuals with severe mental illness relative to others. Rather, relative risks do that, and we have reported odds ratios that are significantly higher in patients with severe mental illness compared with the general population. Because this study is based on 6,510 violent criminals with severe mental illness, it was larger than previously published work. For schizophrenia, the odds ratio was estimated to be 6.3 and similar to findings in other investigations of Australian
(10), Danish
(8), and Finnish
(7) patients. The odds ratios reported in this study, however, might be underestimates because there were individuals with severe mental illness who were not admitted to the hospital over the 13-year period but who nevertheless committed violent crimes.
The definition of violent crime used in this investigation was intentionally broad enough to include offenses that potentially cause significant physical disease and psychological distress. In addition, overall attributable risk fractions were calculated by type of offense. A relatively larger contribution of severe mental illness was observed for homicide and attempted homicide (18%) and arson (16%). Because these are higher-profile crimes, this would partly explain the impression given by the media of the high rates of violence in psychiatric patients
(30) . However, focusing solely on such crimes would not give a complete picture of the public health burden of violence because the base rates are so low, accountable for only 0.6% of the violent crimes in Sweden in the case of homicide and attempted homicide. There was no straightforward relationship between crime severity and attributable risk. For example, the attributable risk for threats and harassment (7.5%) was higher than that for aggravated assault (6.3%).
The contribution of female patients with severe mental illness to violent crime in Sweden was very small. The population-attributable risk of female patients with severe mental illness was 0.6 violent crimes per 1,000 women inhabitants over the period 1988–2000. In other words, less than one violent crime was committed per 1,000 women that was attributable to patients with severe mental illness over a 13-year period in Sweden. Although previous research has shown that female patients with severe mental illness have a higher relative risk of violent offending than male patients
(8), which was also found in the present study, this does not represent a significant public health burden. Nevertheless, violent offending in women was more attributable to severe mental illness than in men. This was especially the case for older women who committed violent crimes, and our investigation would imply that the courts could consider routinely screening such women for psychiatric illness.
This study found that the population-attributable risk fraction was lowest for the youngest age band of 15–24 years, at 2.3% for men and 2.9% for women. This is consistent with research that has reliably established that the two most important risk factors for violence are being male and being young
(23,
24) . When a subpopulation is concomitantly exposed to several risk factors for a certain outcome or disease, the attributable risk of each risk factor will be less significant. Therefore, in younger persons, violent crime was less attributable to the one risk factor, i.e., severe mental illness, as identified by hospitalization, which was examined in this study.
In conclusion, even if one assumes that the association between severe mental illness and recorded violent crime is entirely causal, this population study has demonstrated that the overall contribution of patients with severe mental illness to such crime was about 5% in Sweden between 1988 and 2000. Although this contribution varied by gender, age, and type of violent crime, this finding should generate a more informed debate on the contribution of persons with severe mental illness to societal violence.