The annual cost of treating child and adolescent mental illness was estimated at $11.6 billion in 1998
(1), not including costs incurred outside medical settings. Yet educational, juvenile justice, and child welfare agencies all incur costs related to childhood mental illness
(2), and children often use services from many agencies, to deal with many problems. Studies that examine service use for a limited set of providers (e.g., references
1,
3,
4) or focus on a single diagnosis or presenting problem
(5 –
7) will underestimate the broader community costs of early mental illness.
Four elements are needed to estimate the costs of childhood mental illness across service agencies: a representative population sample; assessment of psychiatric disorder that is independent of treatment records (to measure unmet service needs); information on costs across all relevant service systems; and information on the number of units of each type of service used by each study participant. This study meets these requirements for a population sample of 13- to 16-year-olds in the southeastern United States.
Method
Sampling Frame
The study used data from the Great Smoky Mountain Study sample, drawn from a predominantly rural 11-county area of North Carolina (population 180,000) that had an adequate mental health care system. The sampling frame was the student information management system databases of the 13 school districts in the area. A representative sample of 4,500 children, 1,500 each at ages 9, 11, and 13, was selected using a household equal probability design to select one child from each household.
Two-Stage Sampling
A two-stage sampling process was used to increase the number of mental health service users in the study sample while permitting estimates to be made for the whole population
(8) . All children who scored above a predetermined cut point on a behavioral screening questionnaire
(9), plus a 1-in-10 random sample of children who scored below the cut point, were recruited. Ninety-five percent of families contacted completed the screening questionnaire, and 80% of eligible families (1,073 of 1,346) agreed to participate in the interviews. In addition, all age-appropriate American Indian children living in the area were sought for recruitment irrespective of their screening questionnaire scores, and 81% (350/432) agreed to participate. Of the total sample of 1,423, three died early in the study and are omitted from these analyses. Eligible children and one of their parents were interviewed annually until the youths were 16 years of age. Institutional review board approval was obtained, and both children and parents provided informed consent.
The estimates presented in this article are based on data collected between 1993 and 2000 for each cohort at ages 13, 14, 15, and 16. The average response rate for each wave was 81.6%. The data are weighted back to population rates
(8) .
Approach to Cost Analysis
The first step in cost analysis is to determine the perspective, that is, to answer the question “costs to whom?”
(10) . We estimated the costs to the broad set of health care (primary and specialty), school, juvenile justice, and social service agencies that bear the financial brunt of adolescents’ emotional and behavioral problems. By including a comprehensive set of service agencies, we hoped to approximate a societal perspective
(11) . However, this approach omits many costs borne by families, including direct costs (e.g., travel) and indirect costs such as impact on parents’ ability to work and the child’s future earnings.
Key Measures
Three sets of measures were collected: psychiatric disorders, as a marker of need for services; the number and type of units of service utilized per child; and the cost of each unit of service.
Psychiatric diagnoses were made at annual interviews using the Child and Adolescent Psychiatric Assessment
(12) . Need for services was defined as the presence of either a diagnosis according to DSM-IV criteria
(13) or psychiatric symptoms associated with significant functional impairment at home or in school. Youths with impairing symptoms below the threshold for formal diagnosis were categorized as needing services because earlier work with these data
(14) showed that this group frequently has many symptoms across several diagnostic categories without any formal DSM-IV diagnosis and that they often have a poor prognosis without treatment. This group is roughly equivalent to those who would be given a DSM-IV not otherwise specified diagnosis. Children were categorized as needing services the first time they either met diagnostic criteria for a disorder or had impairing symptoms of a disorder. They were then counted as having that disorder at each of the subsequent data waves. Using this “persistent” definition reflects the chronic nature of psychopathology as well as common clinical procedure: mental health services (for example, stimulant medication for attention deficit hyperactivity disorder [ADHD]) are considered to be needed to maintain mental health after symptoms fall below the full diagnostic threshold.
Service use for mental health problems was identified using the Child and Adolescent Services Assessment
(15), an interview for parent and child that provides details on use of 39 types of service during the 3 months preceding the interview. For each type of service used, information is collected about the number of sessions, the length of visits, and the focus of treatment. The instrument also asks about family income and health insurance. For this article, 21 types of service covered in the interview were classified into seven categories: inpatient hospital, residential, outpatient, school, primary care, juvenile justice, and informal services. Services were excluded from these analyses if they involved no formal costs (e.g., talking to a sibling or parent) or if the primary object of the expenditures by the agency was an adult (e.g., social service investigations of abuse). To ensure that services are related to mental health concerns, the Child and Adolescent Services Assessment uses four safeguards: the measure is administered immediately after the Child and Adolescent Psychiatric Assessment to cue recall. The Child and Adolescent Services Assessment begins by reviewing all mental health concerns identified in the diagnostic interview; when querying about the general services settings, the questions are qualified with the phrase “for any of the kinds of problems that you told me about”; and when prompted for detailed service information, the interviewer is asked to identify the focus of treatment. Only service use related to mental health is coded.
Cost estimates for service units were obtained from a diverse range of national, state, and local resources. A full list of data sources and a detailed description of data collection methods are available in an online appendix at http://devepi.mc.duke.edu/mentalhealthcost.pdf.
When available, unit cost estimates were specific to the state, county, and year from which the utilization data were drawn, and cost estimates included direct costs, such as the salaries of health care providers, and indirect costs, such as administrative support. The consumer price index was used to index costs to the year in which the service was provided if historic unit cost data were unavailable. The figures for some service categories incorporate a range of cost estimates for each service in that category, reflecting cost variations across sources of information. All costs are reported in 2000 real dollars. Participants might use several services and might use a service more than once. We use “service events” to present the number of discrete observations in which a service was reported as being accessed.
Analyses
Cost estimates were calculated by multiplying reported service units by unit costs. The Child and Adolescent Services Assessment obtains service units through items inquiring about duration (in minutes) and number of visits. Cost estimates include average annual costs per individual and total annual costs per 100,000 population. If an individual reported service use at more than one time point, separate cost estimates were averaged for the individual to control for correlated data points. Three-month cost estimates, but not service utilization rates, could be weighted to annual estimates by multiplying estimates by four. A total sample cost estimate was generated by summing costs across all participants. The total sample cost was weighted to obtain an estimate for a population of 100,000. Service utilization rates were computed with logistic regression models using general estimation equations to account for both sampling design and within-subject correlation across multiple waves. Sampling weights were applied for estimates.
Results
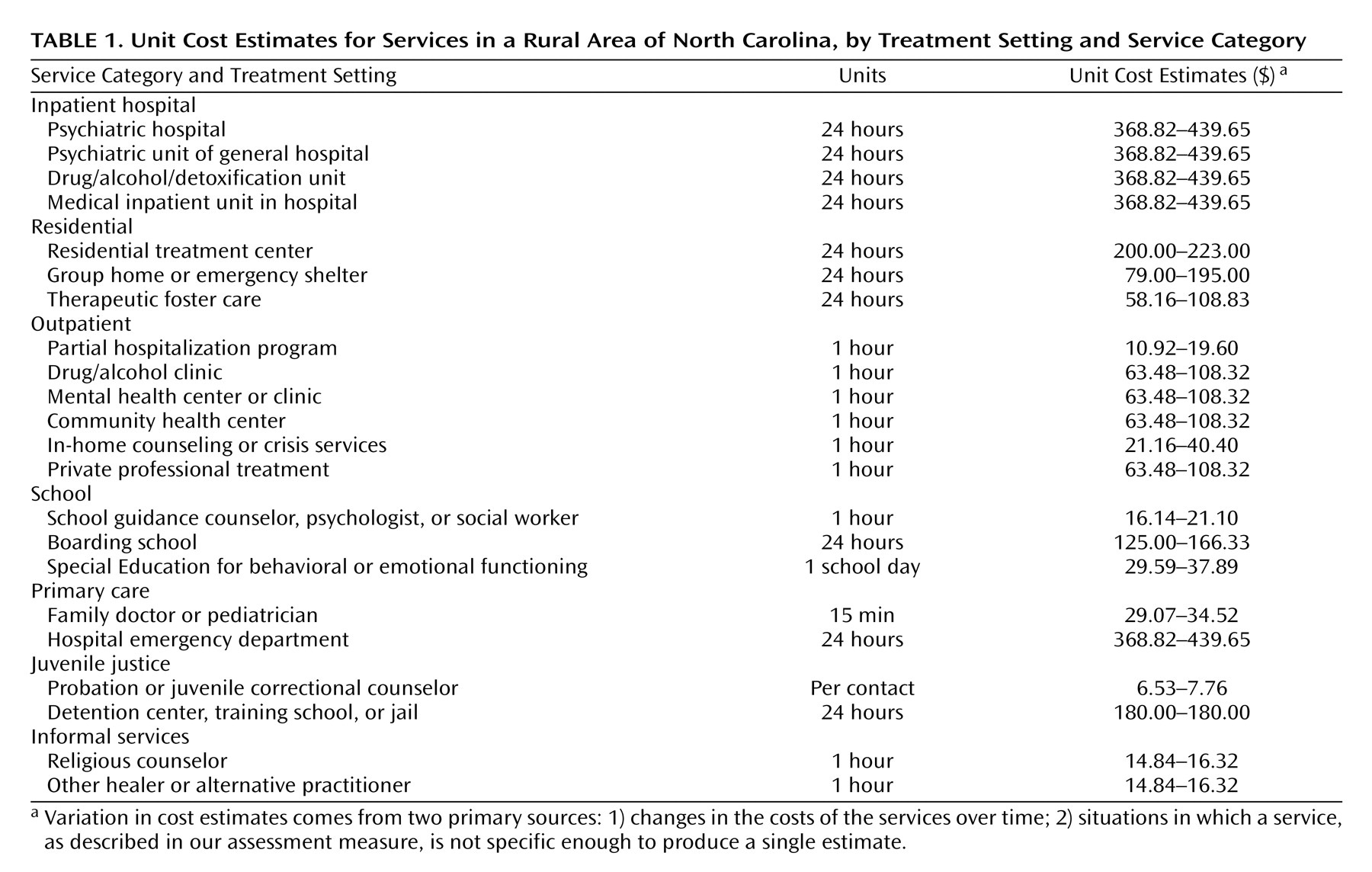
Table 1 lists the categories, services within each category, and unit cost range for each service. The likelihood of service use did not differ from cohort to cohort, so numbers of units of care and costs were aggregated across cohorts.
Utilization Rates and Costs by Service Category
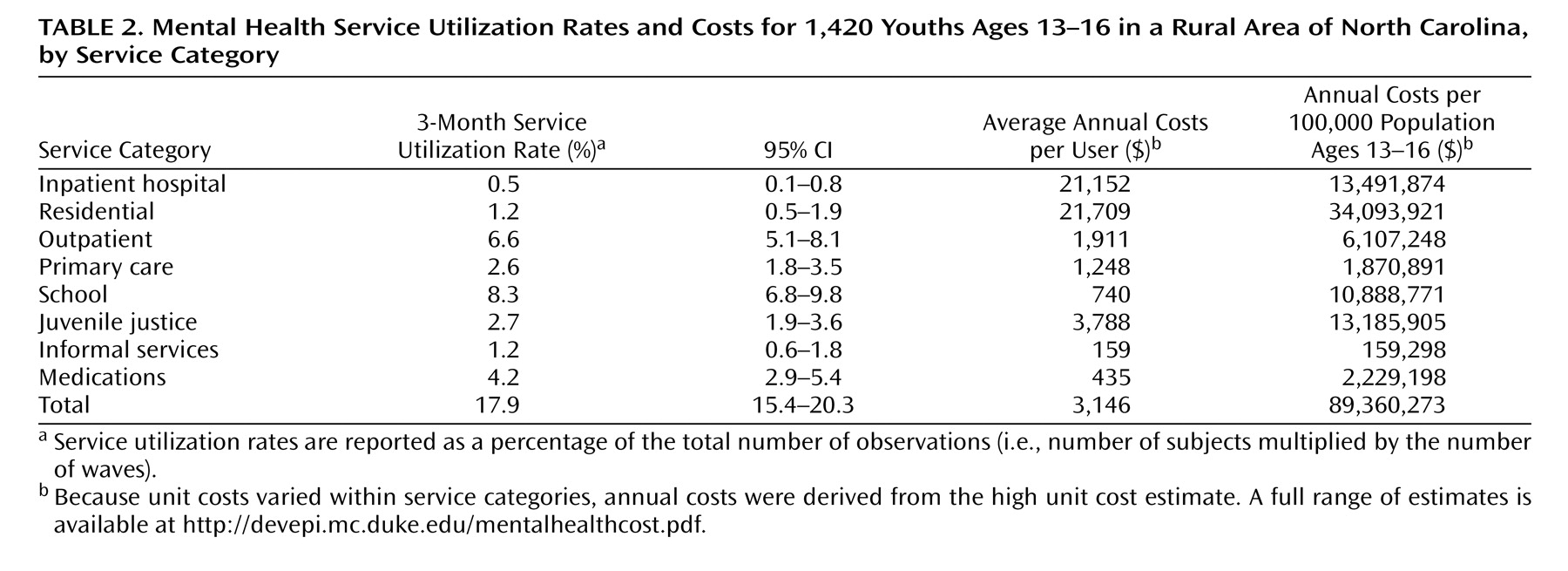
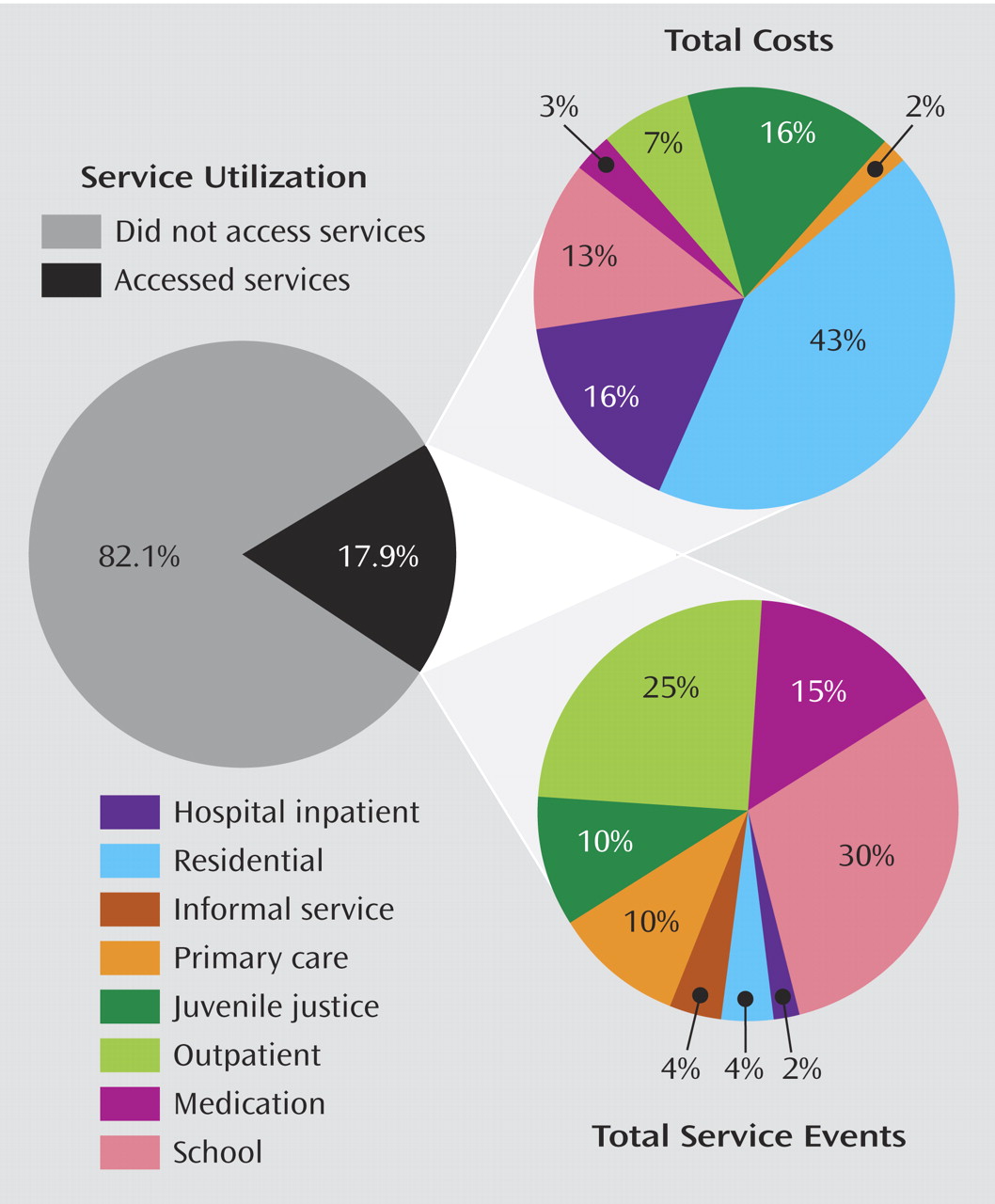
Table 2 presents mental health service costs and utilization rates by service category. Over 3 months, 17.9% of the sample used mental health services. School was the most common setting, followed by psychiatric outpatient, juvenile justice, and primary care settings. In general, rarely accessed services (e.g., inpatient and residential) were the most costly.
Figure 1 summarizes the relationship between service events and costs. It shows, for example, that only 4% of the sample used nonhospital residential services within a 3-month period but accounted for 43% of total costs, while mental health services were delivered in school settings to 30% of the sample for 13% of the total costs.
Details of demographic differences in costs can be found in the online appendix at http://devepi.mc.duke.edu/mentalhealthcost.pdf. The sample had almost equal numbers of boys and girls. Boys were nonsignificantly more likely to use services, but the costs of services for boys were 61% greater than those for girls (average annual costs, $3,803 versus $2,363), and boys were responsible for 70% of the total annual costs. Of the two primary racial/ethnic groups (Anglo and American Indian), Anglos were less likely to use services (17% versus 24%) and costs were about $1,500 less per user, but because they were the majority (90.4%) of the population, they were responsible for most (69.7%) of the costs. The proportion of adolescents using services increased with age (controlling for year), rising from 14.1% at age 13 to 17.3% at age 16. Average annual costs also increased, from $2,433–$2,996 at age 13 to $4,152–$4,725 at age 16.
Costs by Diagnosis
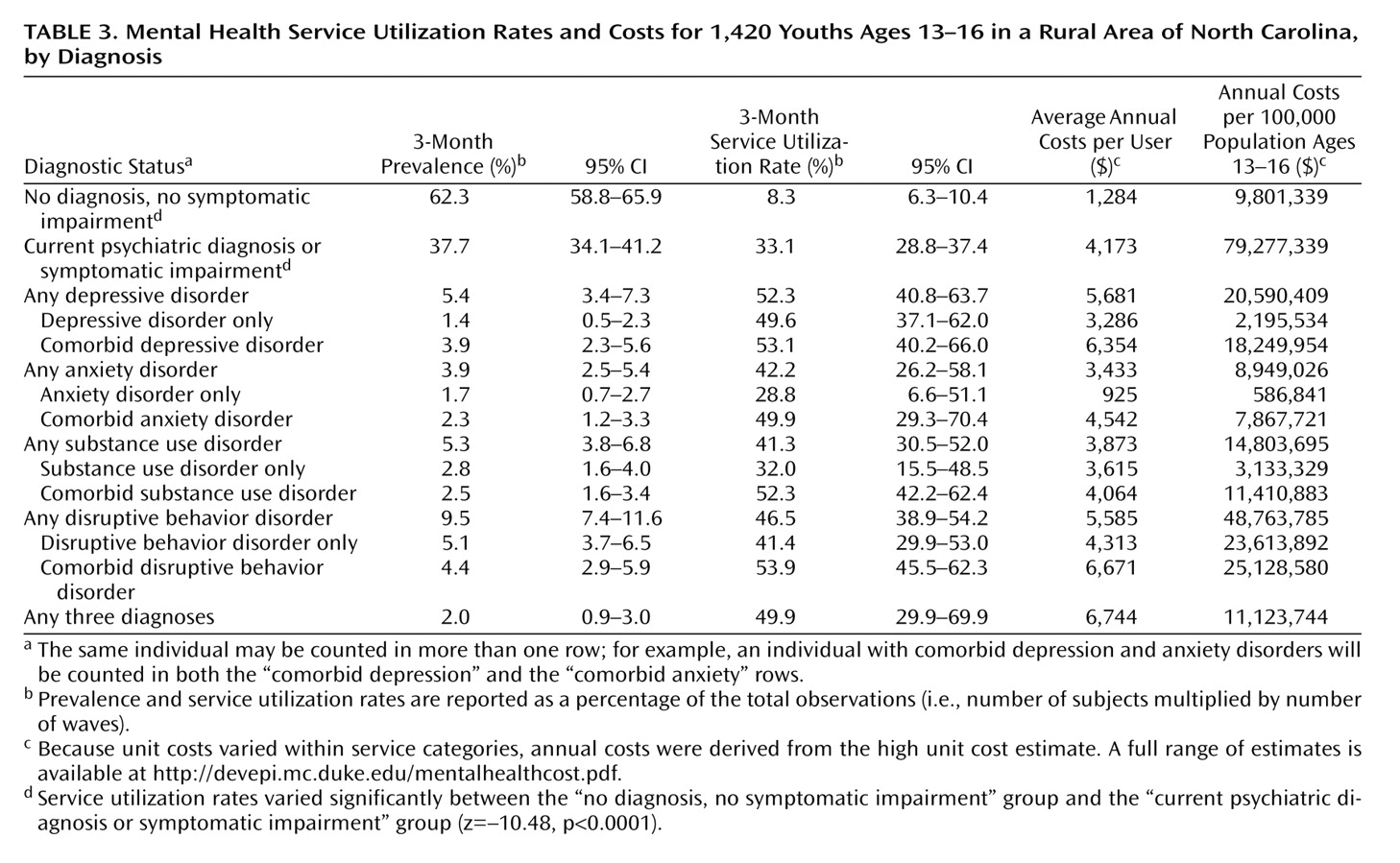
Table 3 illustrates how need for services affected costs. About one-third of adolescents (33.1%) with a need for services used services from any agency. Youths with a formal DSM-IV diagnosis incurred modestly greater costs than those with subdiagnostic impairment ($4,456 versus $4,034) and much greater costs than those without a psychiatric diagnosis or impairment ($1,284).
Among youths with mental illness, comorbidity has been shown to be the rule rather than the exception
(16) . In
Table 3, costs are presented for both single-disorder and comorbid cases in various diagnostic categories. Disruptive behavior disorders (conduct disorder, oppositional defiant disorder, and ADHD) accounted for the largest proportion of costs for single-disorder groups because of both higher prevalence rates and substantially higher costs in juvenile justice and inpatient services. Adolescents with multiple diagnoses incurred the greatest costs, and those with three or more diagnoses the greatest of all ($6,744). However, only 49.9% of even the latter group received any services. Overall, depression and disruptive behavior disorders accounted for the highest rates of service use and the largest proportion of total mental health costs.
Costs by Insurance Status
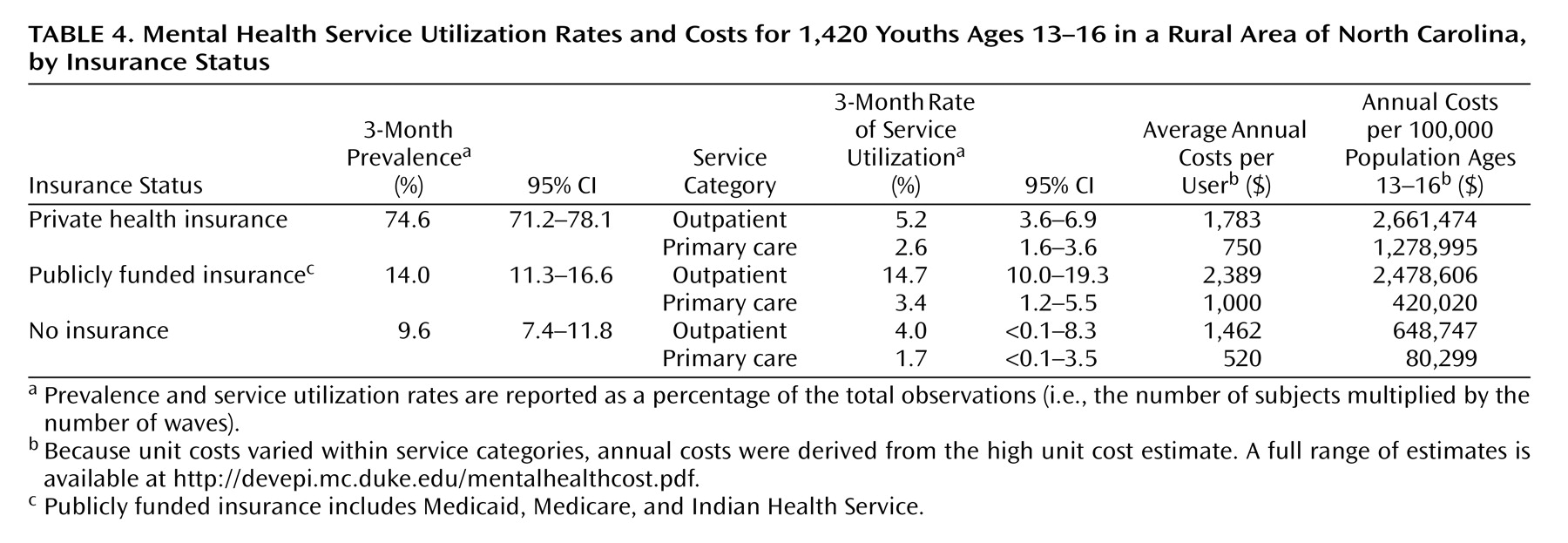
Table 4 compares primary and specialty mental health costs by the primary source of insurance funding. Private insurance was the most common source of funding for the sample (74.6%), followed by public funding (Medicaid, Medicare, Indian Health Service; 14.0%) and no insurance (9.6%). Participants with public insurance were more likely than either privately insured or uninsured children to use specialty mental health services. Yearly costs were greater for children with public funding for primary care services and specialty mental health services.
Discussion
This study is one of the first to look at mental health service costs across a full range of service settings and diagnostic groups. The costs of mental health services in this 11-county area extrapolates to national costs of $10.2 billion to $12.3 billion just for 13- to 16-year-olds. This is three to four times more than previous national estimates for the entire child and adolescent population, which were based largely on health insurance data alone.
A number of specific findings of this study are noteworthy. First, costs for outpatient specialty mental health services constituted about 7% of the total of mental health costs for adolescents. Juvenile justice services and inpatient services, such as inpatient hospitals and group homes, accounted for 67% of all costs. Second, schools were the most frequent service providers for adolescents and were responsible for 13% of the costs; thus, the burden of adolescent mental health problems was commonly borne by agencies that were not designed primarily to provide psychiatric or psychological services. Third, although the per-child costs were similar to those of other diagnostic groups, children with disruptive behavior disorders accounted for the greatest expenses of any diagnostic group because of the higher prevalence of these disorders in childhood. Fourth, less than one in three adolescents who had a need for services during the period examined received any services from any agency. Finally, the proportion of adolescents with service needs who received mental health care in the medical sector was similar for those with private health insurance and for those with no insurance. A higher proportion of those with public insurance received services.
This study contributes in several ways to the literature on the costs of treating adolescent mental illness. It uses a representative population sample and an annual detailed psychiatric assessment of each participant for 4 years as well as details of the type and amount of disorder-related services used across multiple agencies, and it generates costs from detailed investigations of the relevant agencies. Other studies have estimated costs for children with various types of health care funding (e.g., those on Medicaid or those with private health insurance [
1,
3,
4 ]) or children with specific disorders
(5 –
7), but none permitted estimates of costs of multiple service providers for individual cases across a whole population.
The study also presents average costs at both the individual and population levels. The Fort Bragg Demonstration Project
(17) estimated the average costs of services from medical and mental health agencies for children in contact with mental health services, and a Comprehensive Community Mental Health Services for Children and Their Families Program study
(18) of costs in Ohio for children at risk of out-of-home placement obtained cost data from most agencies. Annual estimates of the cost per treated child were between $5,000 and $6,000 in the Ohio sample and around $5,000 for the nonexperimental comparison group in the Fort Bragg study. The equivalent group of adolescents in Great Smoky Mountains Study (i.e., those in contact with specialty mental health services) generated much higher annual costs ($10,921), indicating that the failure to include a full range of service providers can lead to substantial underestimation of costs.
The cost estimates in this study are based on “persistent” diagnoses—that is, once a child was diagnosed, that diagnosis was carried to subsequent observations—to reflect the chronic nature of psychopathology and the clinical reality that patients often continue to be treated after symptoms subside and fall below the full diagnostic threshold. Analyses were also completed on two alternative assumptions: 1) subjects were counted in the diagnostic group only when they met full criteria for the diagnosis; and 2) subjects were excluded from further observations after a diagnosis was met and then was not met or resolved on a subsequent observation. In both scenarios, average annual costs were higher for subjects with a diagnosis and those without than costs computed using the “persistent” diagnosis (in scenario 1, costs were $5,664 and $2,942, respectively, and in scenario 2, $1,543 and $6,013, respectively). These assumptions also change the prevalence rates for the diagnostic conditions. As evidenced by these comparisons, service cost estimates generated with the “persistent” diagnosis should be considered conservative.
Limitations
Several limitations to this study need to be considered. The data are from a relatively rural area in the southeastern United States that may not be representative of the rest of the country in rates of mental illness, levels of service use, and costs per unit of service. However, there is evidence that rates of mental illness are very similar in this and other national and international population samples
(19,
20) and that the proportion of children receiving needed mental health care is similar in other areas of the United States
(21 –
25) and the United Kingdom
(26) . Also, the unit costs used in this study are highly consistent with figures from national and other local estimates (see the online appendix at http://devepi.mc.duke.edu/mentalhealthcost.pdf).
Although the study oversampled American Indians, it included very few African Americans, Latinos, and Asian Americans, because few members of these groups live in the 11-county area studied. Also, in this study, race/ethnicity, family income, and insurance status were confounded: although the prevalence of psychiatric disorders was similar across the sample
(27), Anglos were better off and more likely to have private insurance (and to have lower rates of service use), while African Americans and American Indians were more likely to be poor and to have publicly funded health insurance.
We used information from parents and children as the basis for our estimates of units of service use rather than from administrative sources such as Medicaid claims. The services that carry most of the cost burden, such as schools and the juvenile justice system, do not maintain records that permit extraction of costs of units of service for individual study participants. Medicaid claims data provide estimates of the cost of providing care from the perspective of the payer rather than the patient (e.g., references 3, 4, 28) and are limited to medical service providers. There is a large literature supporting the validity of self- and parent-reported psychiatric symptoms and service use compared with institutional records
(29 –
32) .
Three additional limitations have to do with factors that lay beyond the scope of this article. First, these analyses excluded many costs incurred by families with a mentally ill adolescent, such as additional child care, travel, out-of-pocket expenses, and lost work opportunities. Second, these analyses did not consider the appropriateness or adequacy of the services provided or their impact on the course of illness. Third, the age range of the sample was limited to early adolescence.
Conclusions and Implications
Notable efforts are being made in many states to provide an integrated system of care for children and adolescents with mental illness
(33,
34) . The data presented here reinforce the need for such integration. The adolescents who incurred the greatest costs had complex psychiatric profiles and were likely to need services from many sources. Rates of adolescent inpatient hospitalization have fallen since the 1980s
(35), but it is clear that expensive residential facilities were still seen to be necessary for a small proportion of youths with psychiatric disorders. However, much of the cost is being borne by non-mental health agencies.
These analyses identified a high level of unmet need: some 70% of adolescents with service needs received no help from any of the service sectors whose raison d’être is to provide services to children. Yet, even children who have neither a psychiatric diagnosis nor symptomatic impairment may need mental health care. Children with disabilities or recent trauma, for example, could benefit from counseling.
There is considerable evidence that the majority of adult psychiatric disorders are continuations or recurrences of chronic disorders that have their origins in childhood or adolescence
(36,
37) . Treatments that effectively manage many early-onset disorders are now available
(38,
39) . In this context, the level of unmet need, as well as the burden on service systems that were not designed to deliver expert mental health care, is a matter of grave concern.