How the mind loses its way in schizophrenia has puzzled psychiatrists since the syndrome was first described in the 19th century. Nearly every advance in experimental psychology has included attempts to describe hallucinations and delusions as deficits in specific steps of thinking in schizophrenia. Similarly, each new technique in brain imaging, from EEG through magnetic resonance imaging (MRI), has brought hope of revealing aberrations in the brains of persons with schizophrenia that could account for these hallucinations and delusions. Our inability to find a pathophysiology for schizophrenia that links a malfunction in the brain to a deviant cognitive process that would cause the patient’s thinking to lose its grasp of reality has far reaching consequences for the diagnosis of the illness and its treatment. When we bemoan the empiricism of DSM-IV or the failure of our pharmacological treatments to move beyond dopamine antagonism, we are talking about the limitations of our understanding of how psychosis happens. Indeed, unlike most branches of medicine, psychiatry cannot give patients a simple explanation of what is wrong with them. Six articles in this month’s issue are examples of current research in this area. Each of the articles considers a physiological deficit in the brain revealed by an imaging technique and attempts to link it to cognitive and clinical symptoms. None of the articles, separately or together, give us the all-encompassing picture of schizophrenia that we seek, but each tells us something of how a part of the brain functions abnormally and what the psychological consequence of the malfunction appears to be.
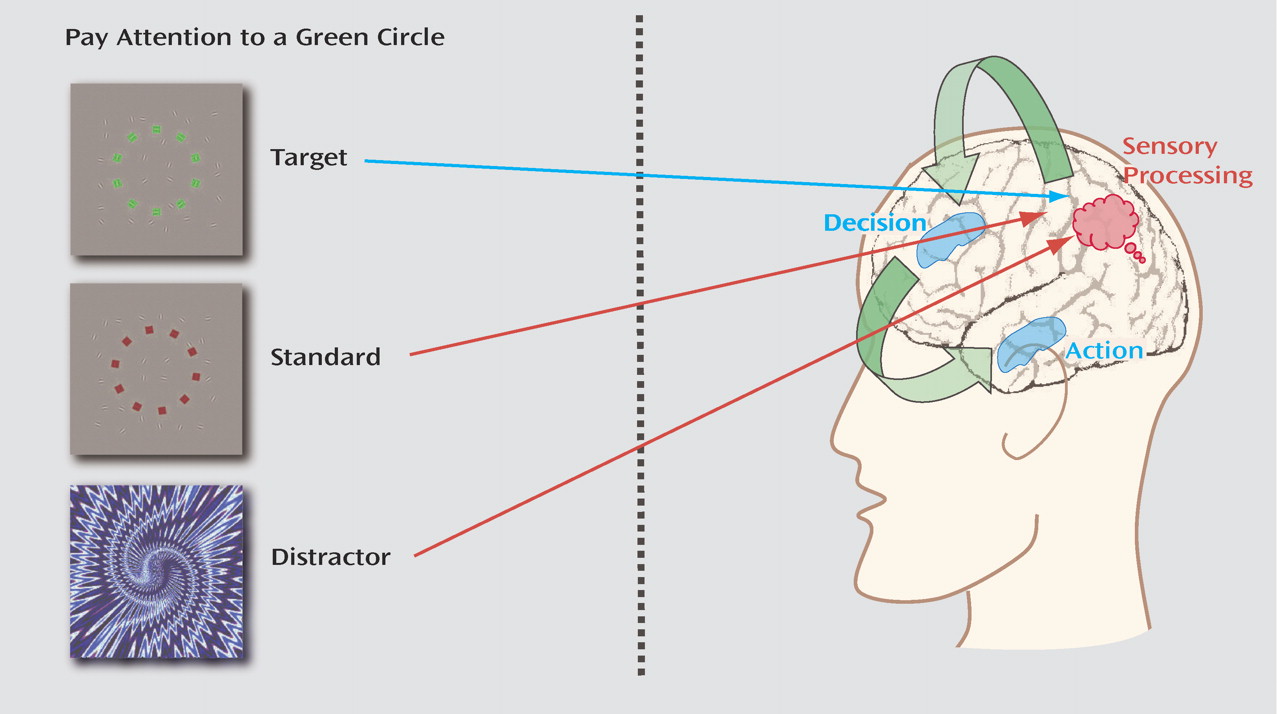
Persons with schizophrenia often cannot automatically discriminate important from unimportant information. Gur et al. (
Figure 1 ) tested whether the problem is the patients’ inability to select what they respond to (top-down processing) or whether it is caused by their inability to filter out responses to distracting stimuli (bottom-up processing). The subjects watched a screen for target symbols that required them to push a button while intermittent distracting pictures were also presented. Gur et al. found decreased blood flow in the frontal cortex and basal ganglia to the target stimuli in schizophrenia. This evidence, acquired using functional magnetic resonance imaging (fMRI), indicates that the brain is not as active in selecting stimuli in the frontal cortex for responses programmed by the basal ganglia. However, the distractor stimuli overactivated the blood flow in the inferior parietal lobe, indicating that neurons there were not as able to discriminate the distractors from the more important target stimuli. Thus, persons with schizophrenia have both problems in information processing.
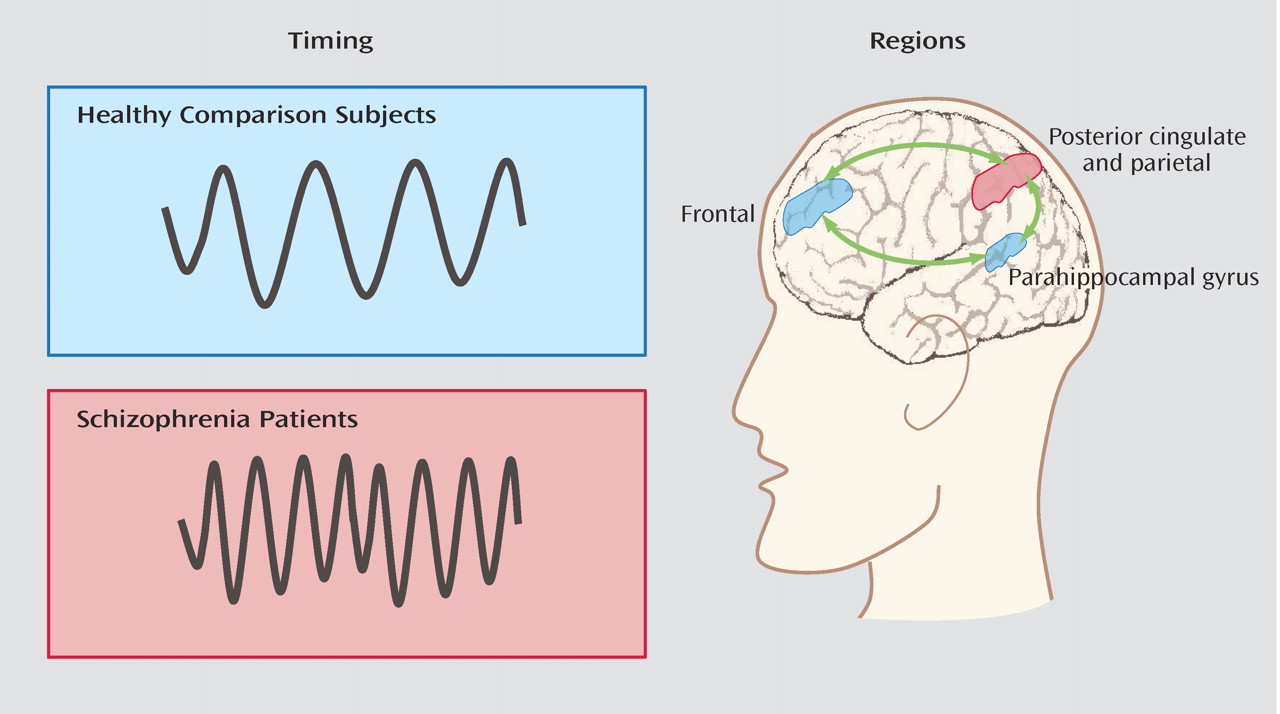
The brain idles in a default mode in which there is interconnected processing of activity among major centers in the cerebral cortex. Garrity et al. (
Figure 2 ) studied this default activity with auditory stimuli, both targets and distractors. They studied the activity of an interconnected network that includes the frontal, cingulate, parietal, and parahippocampal cortices. Although in normal comparison subjects, the network, as measured by its blood flow with fMRI, resonates slowly and regularly, in schizophrenia the activity is increased and more irregular and also correlates with positive symptoms. Garrity et al. conclude that the brain in schizophrenia is, within some portions, hyperactive and some parts hypoactive, but the entire circuit is unable to stabilize itself in the default mode.
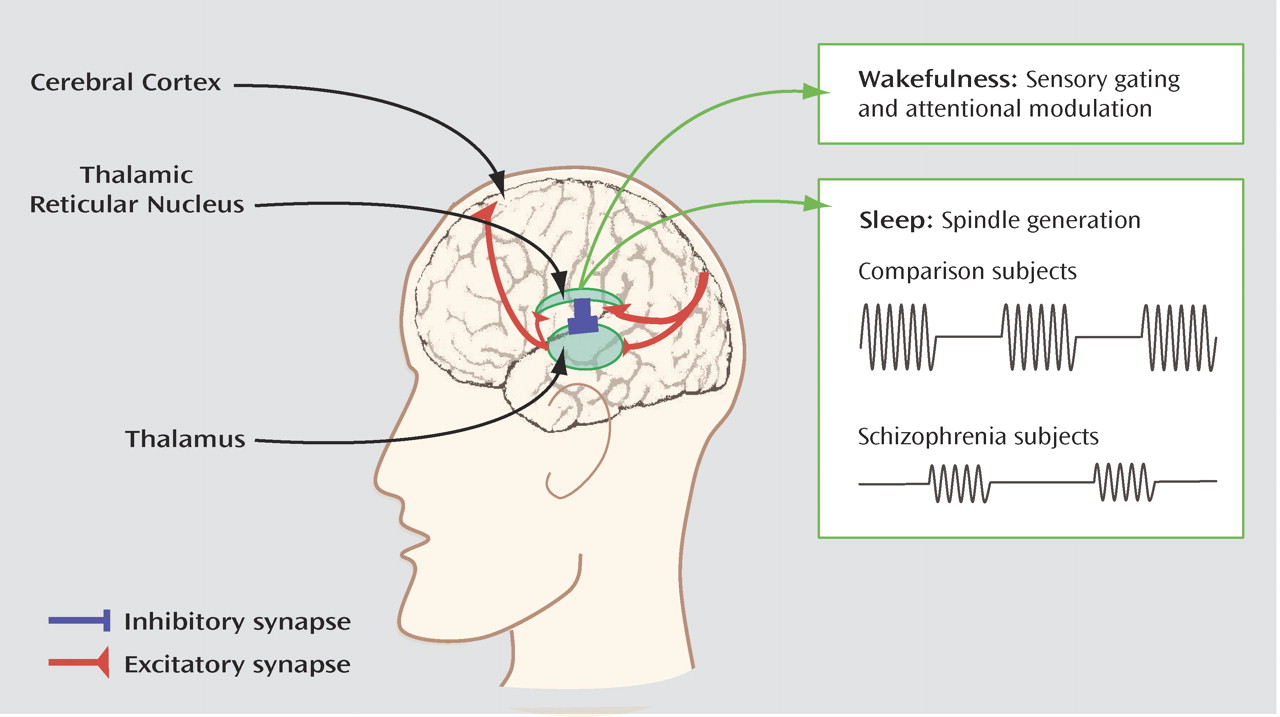
Ferrarelli et al. (
Figure 3 ) examined spontaneous brain activity when schizophrenia patients were asleep, thereby avoiding issues of reduced motivation and increased distractibility. By using a 256-channel EEG system, they found a specific deficit in sleep spindles—waxing and waning oscillations at around 12–15 cycles per second that occur over the central and parietal brain areas. Sleep spindles are generated by the thalamic reticular nucleus, a thin sheet of inhibitory neurons interposed between the thalamus and the cortex that would appear to be hypoactive in schizophrenia, even during sleep. Dysfunction of this nucleus has implication for the waking state, when it plays an important role in sensory gating and attentional modulation, functions that are impaired in schizophrenia.
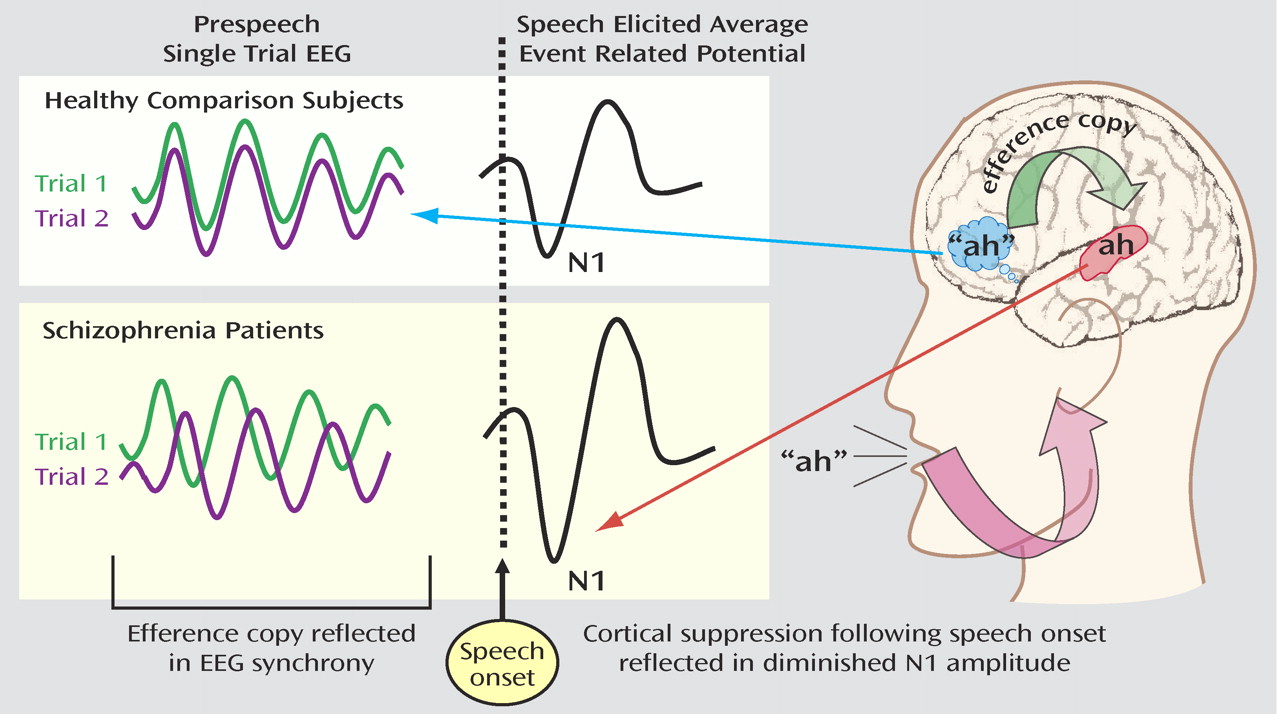
Inhibition is also the theme of the demonstration by Ford et al. (
Figure 4 ) of brain electrical activity before and during speech. Activity in the cortex becomes highly synchronized about 150 msec before the patient says “ah.” The “ah” itself results in activity, measured as the N1 wave of an auditory evoked potential. If the “ah” is generated by the patient’s speech, then the N1 is reduced. Ford et al. suggest that the preparation for speech activates inhibitory neurons in the cerebral cortex. The diminished N1 demonstrates that the activity of the cortex is inhibited, and this inhibition helps normal persons distinguish their own speech from others. Ford et al. hypothesize that malfunction of this system, demonstrated as failure of prespeech synchronization and the lack of inhibition of N1, results in failure of the persons with schizophrenia to distinguish their speech from that of others.
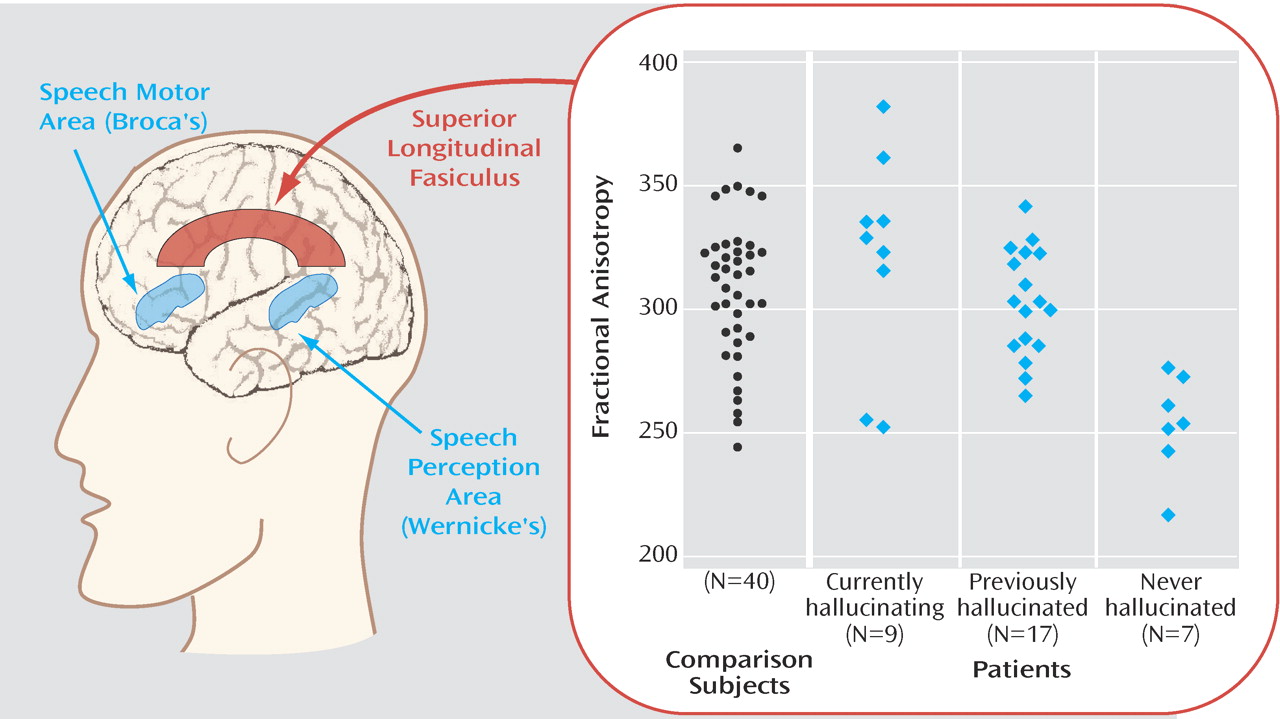
Shergill et al. (
Figure 5 ) use diffusion tensor imaging, a magnetic resonance technique that assesses the alignment of water molecules in myelin fiber paths (fractional anisotropy) as a measure of the integrity of the connections between neuronal areas. One finding is an overall decrease in schizophrenia, in relation to normal comparison subjects, of the myelin pathway between Broca’s motor speech area in the frontal lobe and Wernicke’s receptive speech area in the temporal lobe. Within the schizophrenia group, however, the pathway is closest to normal in patients who have active auditory hallucinations.
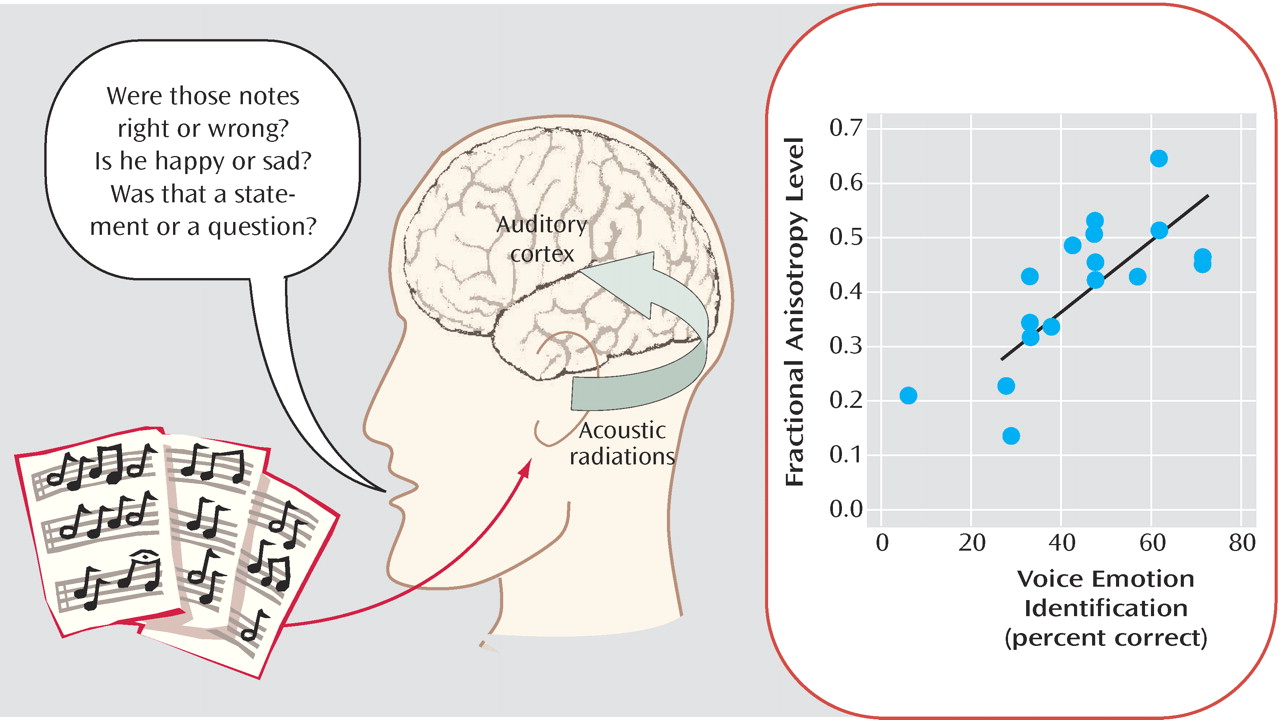
Leitman et al. (
Figure 6 ) also use diffusion tensor imaging to evaluate connections between brain regions—in this case, to determine why patients with schizophrenia have difficulty in evaluating other people’s emotions based upon the rhythm and tone of speech, termed “prosody.” The patients showed deficits not only in differentiating emotions, such as happiness versus sadness, but also in determining whether a common tune was played correctly or with altered notes. An inability to detect both emotions and incorrect tunes was related to a decrease in the integrity in the connections to the auditory cortex (“acoustic radiations”), indicating that the same types of “disconnections” that occur elsewhere in the brain occur also within simple sensory systems. In a follow-up study, Leitman et al. found that patients also had difficulty in differentiating questions versus statements based upon tone of voice alone, suggesting that deficits in the ability to detect prosody may interfere generally with the patients’ ability to interact socially.
Bleuler was among the first to point out that persons with schizophrenia are unusually aware of stimuli in their surroundings, which he ascribed to failure in an unknown inhibitory brain mechanism. Three studies reaffirm Bleuler’s initial observation that deficits in schizophrenia include problems in processing stimuli at the most basic levels: the failure to inhibit activation by distractors in the study by Gur et al., the failure to maintain stable default processing in the study by Garrity et al., and the failure of the inhibitory thalamic reticular nucleus to function even during sleep in the study by Ferrarelli et al. When we consider more complex psychological processes—discerning internal from external speech, as in the study by Ford et al.—the same sorts of elementary inhibitory processes seem to be involved. The conclusion is similar with EEG analysis, recently enhanced by dense multiple channel recording and new analytic techniques, and the measurement of changes in blood flow with fMRI. Blood flow in the brain changes very precisely in time and space in relation to neuronal activity. The magnetic resonance imager measures the new inflow of oxygenated hemoglobin by the change in the quantum state of the iron molecule inside the heme moiety. The two fMRI studies use a signal detection task that originally demonstrated abnormalities in schizophrenia over 30 years ago. The fMRI technique confirms that there is an abnormality in brain function elicited by the task and shows that it is a complex abnormality involving abnormal activation and inhibition in many brain regions.
Two studies use the magnetic resonance imager in the diffusion tensor imaging mode to look at myelin integrity. The finding of alteration in white matter complements earlier findings of reduced gray matter in schizophrenia. The finding of Shergill et al. that temporal-frontal pathways are relatively preserved in patients with auditory hallucinations is evidence that the strengths left to persons with schizophrenia sometimes exacerbate the signs of their illness. More intelligent patients have long been known to have more difficult and persistent paranoia. Here a more intact auditory system ends up to be the substrate of increased auditory hallucinations. Leitman et al. examine a wide range of abnormalities, from executive function to tone detection, and find that all of them are correlated with white matter problems in their appropriate areas, from the primary auditory cortex to the prefrontal lobes. Thus, different psychological abnormalities may have a similar type of tissue pathology, with the difference in psychological outcome simply reflecting the area of the brain involved. The parsing of schizophrenia neuropsychologically then becomes similar to the neurologist’s evaluation of a stroke: the vascular process is the same, but the consequence to the patient depends on which brain region is infarcted.
All six studies examined patients taking medication, and it is fair to ask if we are seeing pathology that is not corrected by medication or whether we are seeing the effects of medication. The authors make reasonable cases that uncorrected pathology, rather than medication effect, is the likely source of their findings. If so, the studies reaffirm to us the burden of illness that patients face in trying to approach even very simple tasks. Gur et al., for example, point out that distractors cause much larger areas of the frontal cortex to become activated in schizophrenia than in healthy comparison subjects. One explanation is that the patients, who ultimately perform as well as the comparison subjects on these simple tasks, must expend much more effort at higher executive brain levels to handle tasks that are handled more easily and automatically at lower sensory levels by the comparison subjects. It is sometimes helpful to tell patients something about how their brains may be malfunctioning. For example, one of my patients was in trouble with his family because he spent too much time with an audio synthesizer that produced ocean noises. I explained to him and his family that his control over the wave noises was substituting for his inability to control the noisy environment in his apartment house. They linked the use of the synthesizer to his becoming ill, whereas I saw it as his attempt at restoration. Together, he and his family reached an understanding of when he needed to use the wave sounds by himself and when he should attempt to interact with his family instead of relying on it to isolate himself.