Clinical experience suggests that shame is central to persons with borderline personality disorder
(1) . Yet shame is often neglected because accompanying behaviors, such as hiding or concealment, make it difficult to detect and because it may be obscured by its possible consequences, including anger. Clinicians have argued that in borderline personality disorder, shame is the emotion most strongly linked with chronic suicidality, self-injurious behavior, anger, and impulsivity
(2,
3) . It has even been proposed that borderline personality disorder may be a chronic shame response
(4) . However, to our knowledge, no quantitative empirical studies have examined the level and impact of shame among individuals with borderline personality disorder.
Shame is usually experienced as aversive and is accompanied by a feeling of being exposed and devalued. It has been defined as a social but inner experience of self as an unattractive social agent, under pressure to limit possible damage via escape or appeasement
(5) . The subjective experience of shame is often associated with observable shame behaviors, such as blushing, lowering the head, avoiding eye contact, and the impulse to hide and escape
(5) . Often, shame elicits secondary emotional responses, such as anger or rage, which serve to conceal or cope with feelings of shame. Thus, shame-proneness is related to anger and high impulsivity
(6), which are common problems in borderline personality disorder. Individuals may use safety behaviors to avoid situations that may provoke shame, such as seeking help or social encounters. This may be a major problem in clinical settings, since shame has been shown to be related to nondisclosure in treatment
(7) . State shame, the situation-specific and often relatively transient emotion, should be differentiated from shame-proneness, a person’s tendency to experience shame in various situations.
Shame and guilt need to be distinguished as well. According to Lewis
(8), shame implies a focus on the global self, whereas guilt arises when the focus is on a specific behavior. Accordingly, guilt often leads to reparative, adaptive, and empathic behavior, whereas shame has been linked to anger attacks
(6), avoidant and less empathic behavior
(9), self-stigma
(10), and suicidality
(11) . In many studies, shame has been positively correlated with psychopathology and interpersonal difficulties. In contrast, guilt is often unrelated to psychopathology
(12) .
Cognitive research has shown that a person’s self-concept is characterized both by explicit, consciously accessible self-related cognitions and by implicit and automatic self-related cognitions that are not necessarily congruent. For example, a person who is prone to shame may explicitly say, “I am embarrassed,” a statement that is, at an implicit level, usually accompanied by a variety of affects and memories of having been shamed that the individual may not be aware of. Since individuals are likely to conceal shame-related cognitions because of the very nature of shame, it is useful to use both explicit and implicit measures to assess shame
(5) . This is particularly important in borderline personality disorder, because implicit as well as explicit cognitive processes influence emotional regulation (or dysregulation). According to the cognitive model, schemata—that is, basic cognitive structures in memory—automatically and implicitly guide our perceptions and interpretations of the self and the world
(13) . Similarly, from a psychodynamic perspective, implicit and unconscious shame-related memories and fantasies are crucial, especially in borderline personality disorder
(14) . A person with high implicit or unconscious shame-proneness is therefore likely to be particularly emotionally vulnerable or dysregulated.
The Implicit Association Test (IAT) is a measure of automatic or implicit attitudes
(15) . Originally used to measure prejudice, it has recently been used to measure implicit self-concept
(16) and dysfunctional cognitive schemata, especially in anxiety disorders
(17) . The IAT uses reaction time measurements to determine the relative strength of implicit associations between concepts (e.g., self versus best friend) and attributes (e.g., shame versus anxiety), based on the notion that quicker processing speeds equate with stronger associations. The IAT has been shown to have strong reliability and validity in assessing the association of the self with anxiety-related stimuli
(18) . It has also been found to discriminate between persons with different phobias
(17) . One key advantage of the IAT is that the results are not influenced by self-representational strategies that may influence explicit measures
(15), a quality that is particularly important in the assessment of shame.
This study was designed to test three hypotheses:
1. Shame-proneness and state shame, as assessed by self-report measures, are higher in women with borderline personality disorder than in women with social phobia and healthy women. Persons with social phobia can be considered a particularly relevant clinical comparison group because fears of being humiliated and devalued constitute a core characteristic of social phobia.
2. Women with borderline personality disorder have a more shame-prone implicit self-concept than women with social phobia or healthy women, as evidenced by a stronger association of the self with shame (relative to anxiety) in the IAT.
3. Explicit shame and shame-proneness as well as a strong implicit association of self with shame (relative to anxiety) in the IAT are associated with low self-esteem, low quality of life, and high anger-hostility.
Method
Participants
Sixty women with borderline personality disorder were recruited at the Department of Psychiatry and Psychotherapy, University of Freiburg, Germany, and the Department of Psychiatry, Meissenberg, Zug, Switzerland, and were assessed 1 week after admission to an open ward for an inpatient program of dialectical behavior therapy. Typically, patients were admitted because of frequent self-injuries or emotional instability and anger attacks that did not respond to outpatient treatment. None of the participants had been admitted for suicide attempts. All 60 women met DSM-IV criteria for borderline personality disorder as assessed by the appropriate section of the Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II; 19). Axis I comorbidity was assessed with the Mini-International Neuropsychiatric Interview
(20) . All admitted women with borderline personality disorder who met inclusion and exclusion criteria and were willing to participate were assessed consecutively.
Thirty female outpatients with social phobia were recruited at the Department of Psychiatry and Psychotherapy, University of Freiburg, and at the Department of Clinical and Cognitive Neuroscience, Central Institute of Mental Health, Mannheim, Germany. All 30 women met DSM-IV criteria for social phobia, and axis I and II comorbidity was assessed with the SCID-I
(21) and SCID-II. Exclusion criteria for both the borderline personality disorder and social phobia groups included a history of schizophrenia, bipolar I disorder, or mental retardation; for the social phobia group, comorbid borderline personality disorder was an exclusion criterion.
Sixty healthy female comparison subjects were recruited in Freiburg and carefully screened for a current or lifetime diagnosis of any axis I or II disorder.
All 150 study participants were 18 to 50 years of age, and all gave written informed consent after the procedures had been fully explained to them. The study was approved by the ethics committee of Freiburg University. All subjects had German as their native language and had completed at least 9 years of school.
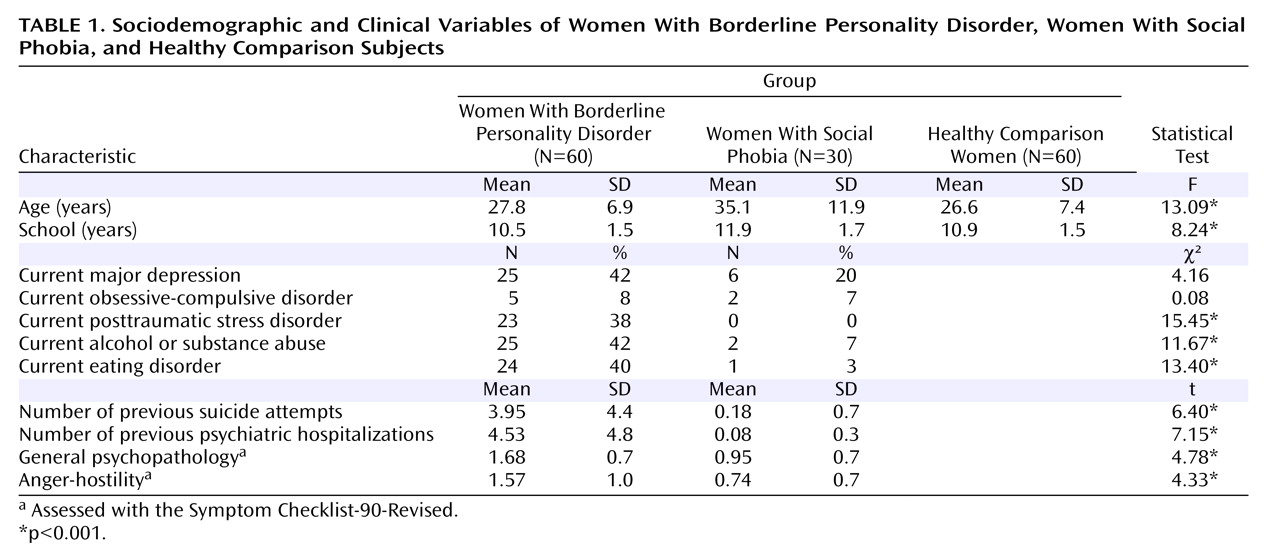
Demographic and clinical data are presented in
Table 1 . Women with borderline personality disorder had more axis I comorbidity than women with social phobia, which was reflected in significantly more frequent suicide attempts and psychiatric hospitalizations and more severe general psychopathology. Fourteen of the women with social phobia (47%) had one or more comorbid personality disorders, including avoidant (N=13), dependent (N=2), and obsessive-compulsive (N=3) personality disorders. Axis II comorbidity in women with borderline personality disorder was not assessed. Ten women with borderline personality disorder (17%) had a comorbid social phobia.
Measures of Shame and Anxiety
Tangney and colleagues’ Test of Self-Conscious Affect–3 (TOSCA-3; 22, 23; German version by N. Rüsch, R. Brück, unpublished) is a scenario-based self-report questionnaire measuring proneness to shame, guilt, detachment, and externalization. We used a short version validated by Tangney and colleagues that consists of 11 instead of 16 negative social scenarios. One scenario, for example, is as follows: “You attend your coworker’s housewarming party and you spill red wine on a new cream-colored carpet, but you think no one notices.” For each scenario, four possible reactions are presented; for this scenario: “You would wish you were anywhere but at the party” (indicating shame-proneness); “You would stay late to help clean up the stain after the party” (guilt-proneness); “You think your coworker should have expected some accidents at such a big party” (detachment); and “You would wonder why your coworker chose to serve red wine with the new light carpet” (externalization). For each scenario, all four reactions are rated from 1=not likely to 5=very likely, yielding sum scores between 11 and 55.
State shame was assessed with the Experiential Shame Scale developed by Turner (ESS; 23, 24; German version, N. Rüsch, R. Brück, unpublished), an 11-item self-report questionnaire that captures physical, emotional, and social aspects of momentary shame. Item examples, all rated from 1 to 7, include “Physically, I feel . . . pale/flushed,” “Emotionally, I feel . . . content/distressed,” and “Socially, I feel . . . like being sociable/hiding.” The State-Trait Anxiety Inventory (STAI; 25; German version, 26) was used to measure both state anxiety (STAI-X1) and trait anxiety (STAI-X2). The ESS and the STAI-X1 were administered immediately after the IAT.
Implicit Association Test
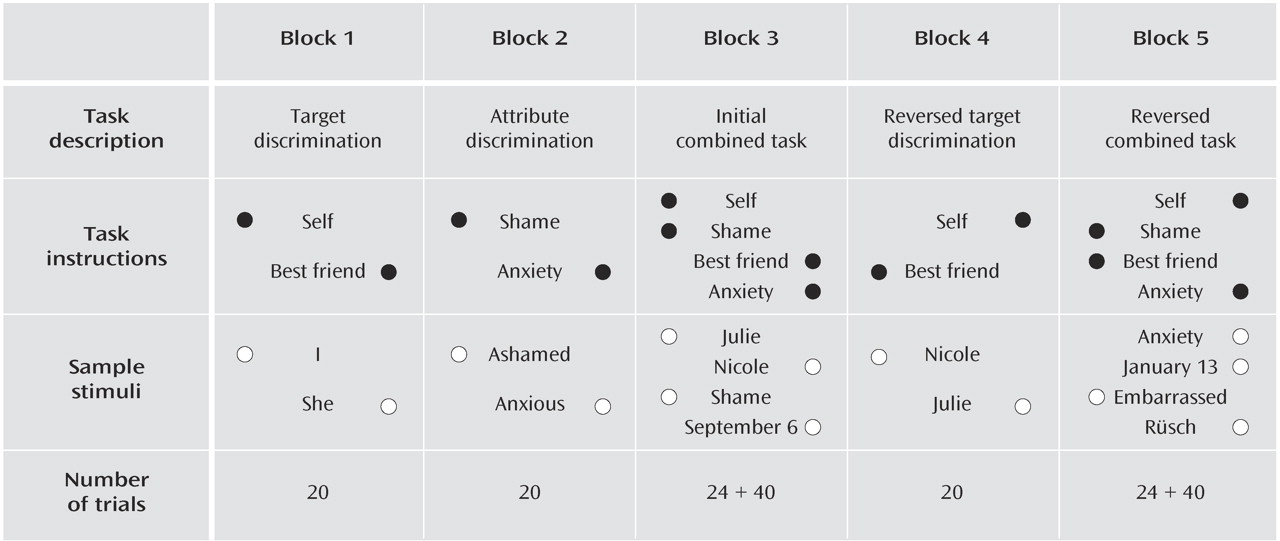
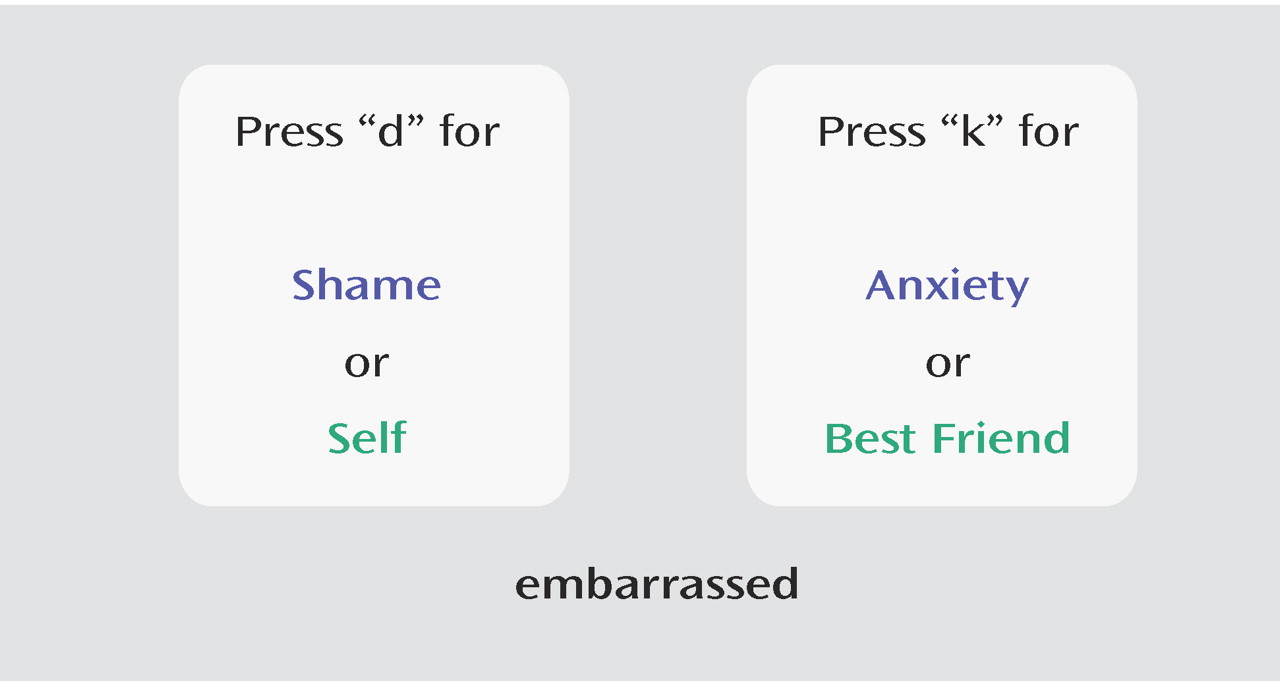
In the IAT, participants classify consecutive words into superordinate categories. The target categories were “self” versus “best friend,” and the attribute categories were “shame” versus “anxiety” (
Figures 1 and
2 ). The idea of the task is that verbal stimuli are classified more quickly when the target and attribute category pairings (e.g., self/shame) match the individual’s automatic associations with the target categories versus when the target and attribute category pairings are mismatched. For example, in our study a subject who implicitly associated herself more strongly with shame than anxiety was expected to respond faster when the target concept “self” and the attribute dimension “shame” were assigned to the same response key as compared with the pairing “self” and “anxiety.” During the IAT, a series of words were presented in the center of the screen that fell within the categories represented either on the left side or the right side of the screen (
Figure 2 ). The subject’s task was to press the left response key to indicate that the word fell into the categories represented on the left side, and the right response key to indicate that the word fell into the categories on the right side. There were five trial blocks in all (
Figure 1 ). In blocks 1 and 2, the presented words had to be classified as an exemplar of either the target categories (e.g., when the word “she” was presented, the subject had to select either “self” or “best friend”) or the attribute categories (e.g., for the word “anxious,” either “shame” or “anxiety”). Within each block, the target (or attribute) categories were assigned to one of two response keys. In block 3, the first critical block, pairs of a target and an attribute category (e.g., “self” and ”shame” on the left, “best friend” and “anxiety” on the right, as shown in
Figure 2 ) were assigned to each of the two response keys. In block 4, the key assignment of the target categories was switched as compared to block 1—for example, in block 1 “self” was on the left and “best friend” on the right, and in block 4, “self” was on the right and “best friend” on the left. In block 5, the second critical block, the pairing of target and attribute categories was inverted as compared with block 3.
The IAT is a measure of the relative strength of associations. Therefore, an equivalent comparison category for shame was required. Anxiety was selected as a reference for shame, since both are negative emotions. Thus, we controlled for the possibility that subjects may associate themselves with negative emotions in general rather than with shame in particular. We used the following stimuli for each category: For “self” (“I”) versus “best friend” (“she”), three additional personal stimuli (first name; last name; date of birth) were used. In our version, the German term we used for the category “best friend” (“Beste Freundin”) designates a female friend only. Because all our subjects were female, they were asked to choose a female best friend in order to avoid gender effects. For shame, the stimuli were “shame,” “ashamed,” and “embarrassed,” and for anxiety, they were “anxiety,” “fear,” and “anxious.”
The IAT was administered on a personal computer. Stimulus presentation was controlled by a program (kindly provided by A. Greenwald, personal communication) using Inquisit software
(27) . The order of blocks 3 and 5 was counterbalanced across subjects. The IAT score was calculated according to the improved scoring algorithm
(28), resulting in a measure that represents the difference in reaction time between the critical blocks 3 and 5 divided by the standard deviation of all reaction times for blocks 3 and 5. Negative values represent a stronger association between self and anxiety (relative to shame), and positive values indicate a stronger association between self and shame (relative to anxiety).
A technical failure caused the loss of IAT data for two of the women in the social phobia group. One woman in the borderline personality disorder group was unable to complete the IAT because of impaired vision.
Measures of Self-Esteem, Quality of Life, and Psychopathology
General self-esteem was measured with a 10-item self-esteem scale that yields an average score between 0 and 3 (29; German version, 30). Quality of life was assessed by the SmithKline Beecham Quality of Life Scale (31; German version, N. Rüsch, R. Brück, unpublished), a 28-item self-report questionnaire that assesses various constructs, including psychological and physical well-being, social relationships, activities, and work, with scaling and average score from 1 to 7. Depression was measured with a 15-item version of the Center for Epidemiologic Studies Depression Scale (CES-D Scale; 32; German version, 33), in which items are scaled from 0 to 3. General psychopathology was assessed with the Symptom Checklist-90-Revised (SCL-90-R; 34; German version, 35), which yields an average score of general psychopathology and a score of anger-hostility, both ranging from 0 to 4. Data from the SCL-90-R were not available for women in the healthy comparison group.
Statistical Analysis
All analyses were conducted with SPSS, version 11.5 (SPSS, Chicago). Group means were compared using analyses of variance (ANOVAs) and two-tailed t tests for three and two groups, respectively. Between three groups, post hoc comparisons were performed with the Scheffé test to correct for multiple comparisons. To keep type I error from multiple comparisons at a reasonable level, only findings at the p<0.01 level were considered significant in all analyses.
Results
Between-Group Differences in Self-Report Measures
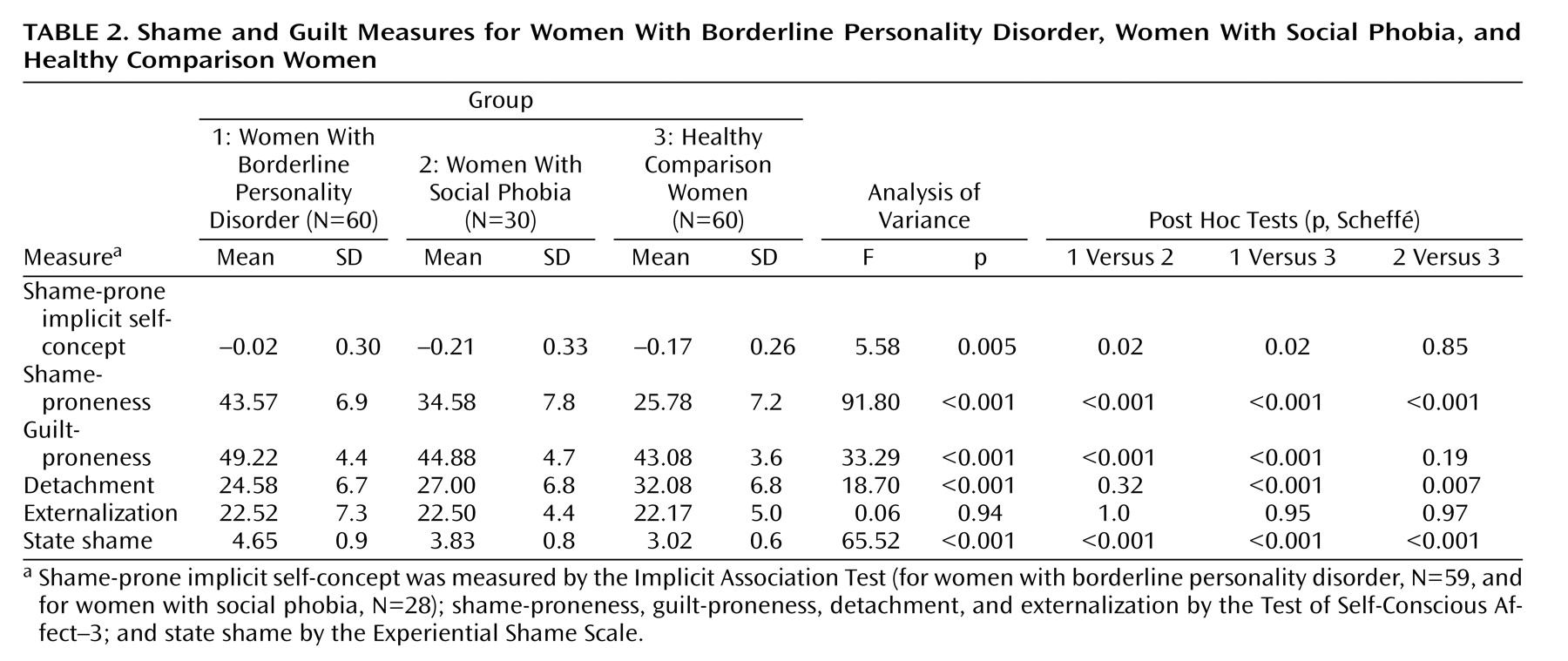
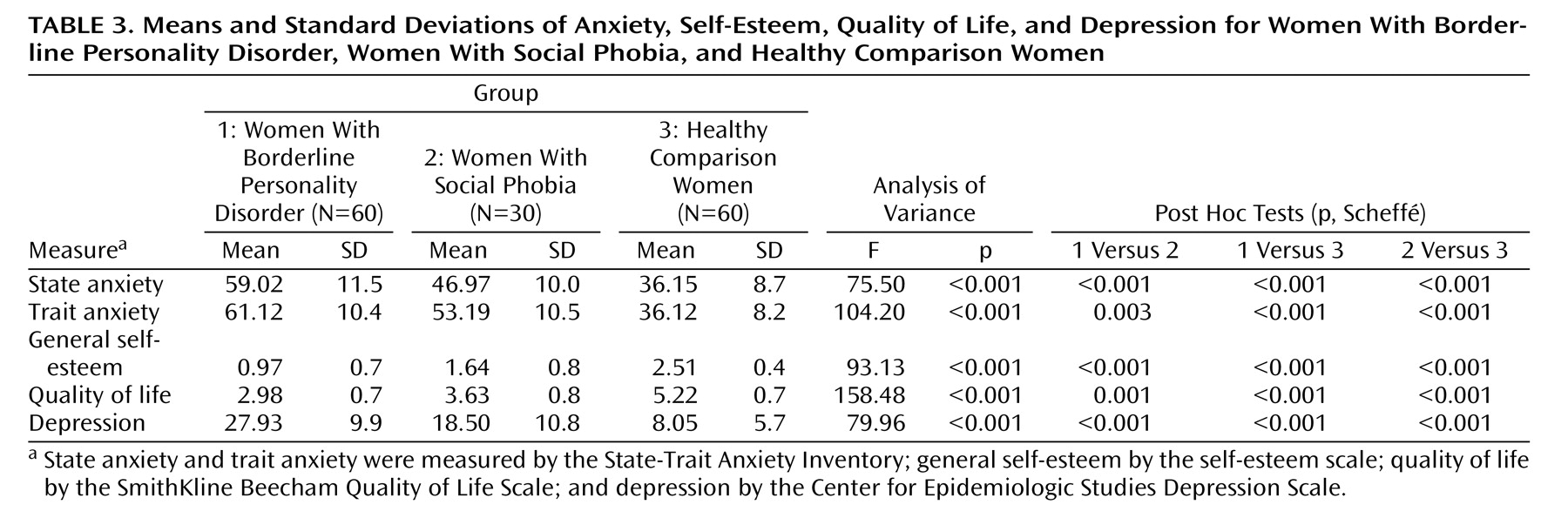
To test our first hypothesis, that shame-proneness and state shame in self-report measures are higher in women with borderline personality disorder than in women with social phobia and healthy women, we conducted a series of ANOVAs. Overall, women with borderline personality disorder reported significantly higher levels of shame, guilt, and anxiety than women with social phobia, who in turn showed higher levels than healthy women (
Tables 2 and
3 ). The group difference in guilt-proneness was no longer significant after shame-proneness was controlled for in an analysis of covariance, which suggests that the group difference in guilt-proneness was due to shared covariance with shame-proneness and that “shame-free” guilt-proneness was similar in all three groups. By contrast, even when controlling for guilt-proneness, the three groups differed significantly in “guilt-free” shame-proneness (F=42.00, p<0.001).
With regard to self-esteem, quality of life, and depression, women with borderline personality disorder were most impaired, followed by women with social phobia and healthy women (
Table 3 ). Anger-hostility was significantly higher in women with borderline personality disorder than in women with social phobia (
Table 1 ).
Implicit Shame-Prone Self-Concept
Between-Group Differences
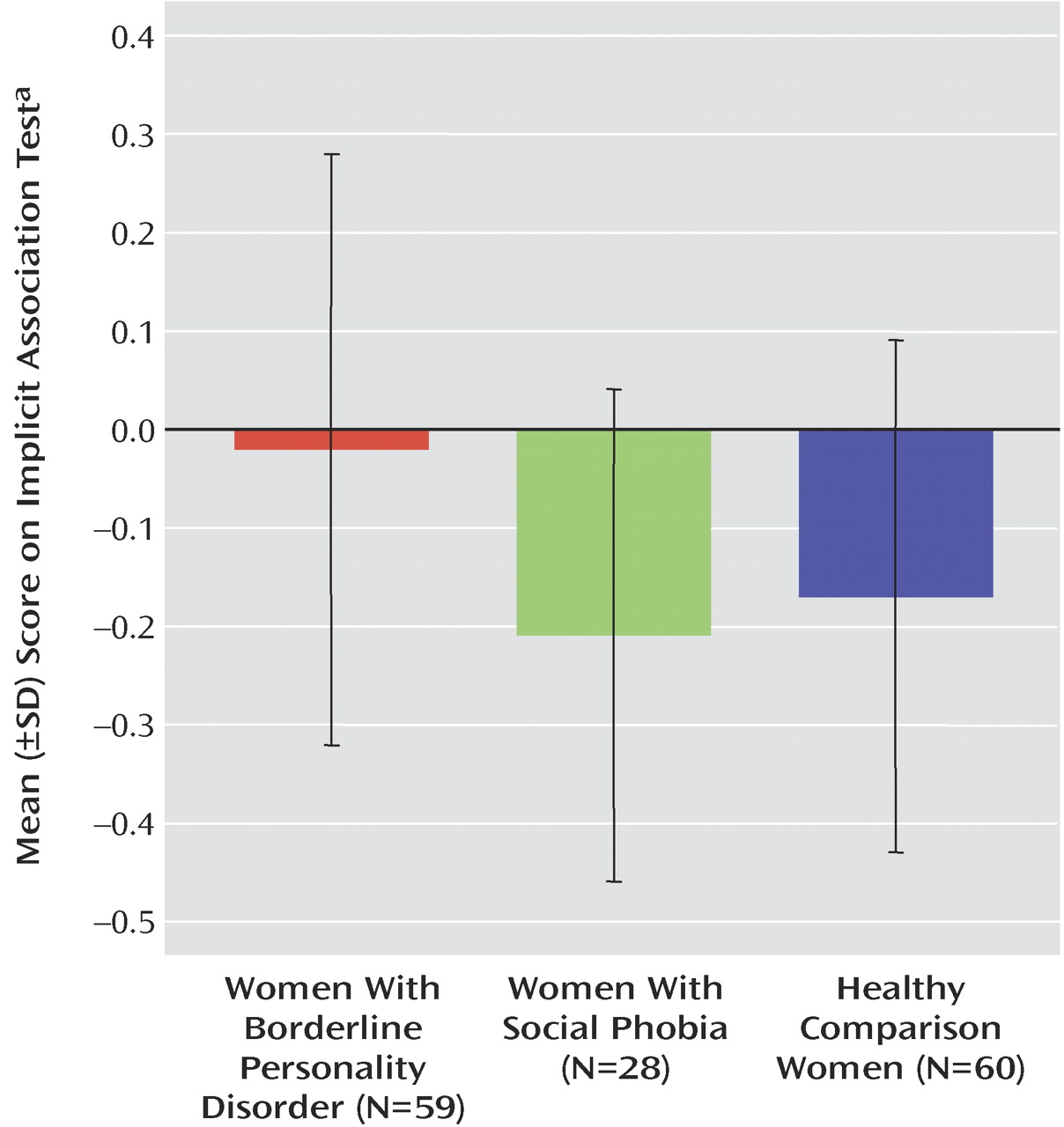
To test our second hypothesis, that self is more strongly associated with shame (relative to anxiety) among women with borderline personality disorder compared with women with social phobia and healthy women, we conducted a between-groups ANOVA (
Table 2 ). On average, women with borderline personality disorder had IAT scores that approached zero, indicating that they implicitly associated themselves equally strongly with shame and anxiety. In contrast, the mean IAT scores of women with social phobia and healthy women were negative, indicating that they implicitly associated themselves more strongly with anxiety than with shame (
Figure 3 ). In addition, women with social phobia had nonsignificantly lower IAT scores (indicating a more anxiety-prone self-concept) than healthy women.
Correlations Between IAT and Self-Report Measures
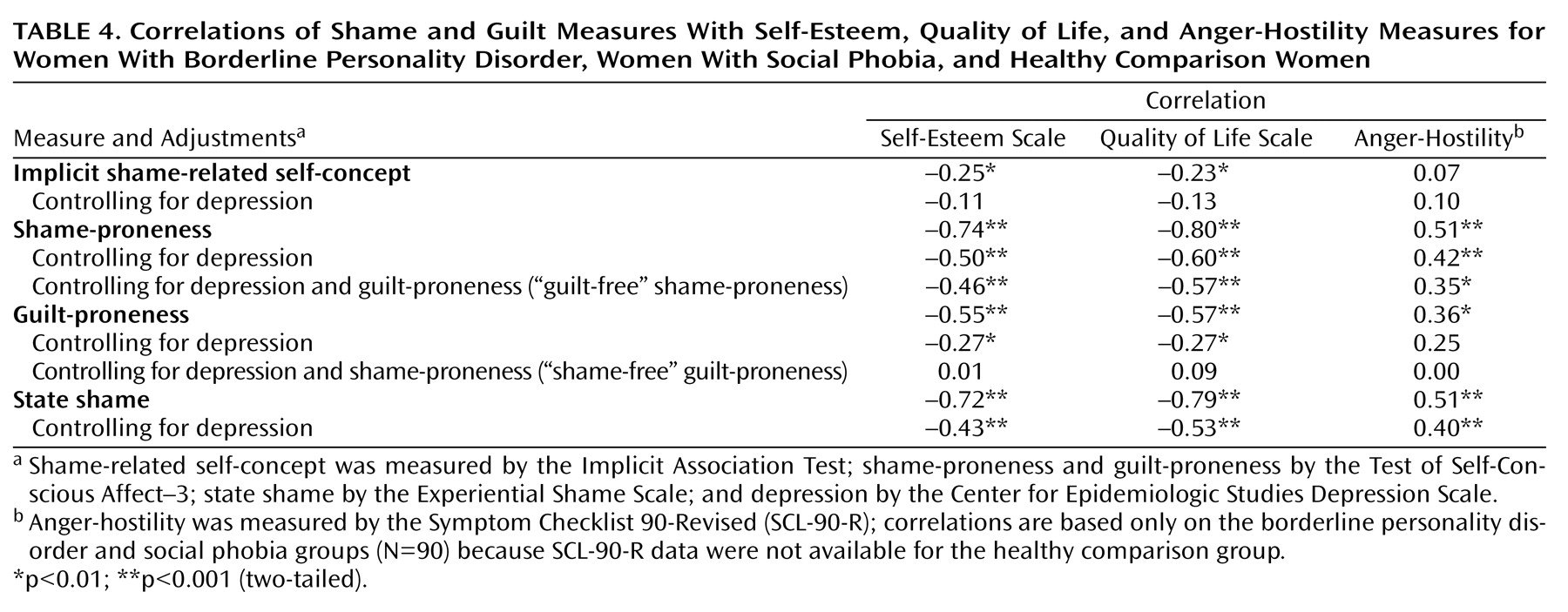
To test our third hypothesis, we calculated zero-order Pearson correlations between the IAT score and scores for self-esteem, quality of life, and anger-hostility (
Table 4 ). A shame-prone implicit self-concept (relative to anxiety) was significantly negatively correlated with general self-esteem and quality of life. However, these correlations were no longer significant after depression was controlled for. There was no significant correlation between the IAT score and anger-hostility.
We also determined how explicit measures of shame and anxiety were related to scores on the IAT. To make the questionnaire measures comparable to the IAT, which provides a relative measure of shame- and anxiety-related implicit self-concept, we calculated relative self-report indices. For this purpose, difference and ratio scores were derived from the standardized z-scores of the respective state (ESS – STAI-X1; ESS/STAI-X1) and trait (TOSCA-3 – STAI-X2; TOSCA-3/STAI-X2) measures. There were no significant correlations between the IAT score and the state or trait self-report measures of shame relative to anxiety.
Correlations Between Shame and Guilt Questionnaires and Self-Esteem, Quality of Life, and Anger-Hostility Measures
Continuing to test our third hypothesis, we assessed the relation of explicit shame and guilt measures to self-esteem, quality of life, and anger-hostility measures by calculating zero-order correlations and partial correlations, controlling for depression (CES-D Scale score) as a possible confounding factor (
Table 4 ). Both shame-proneness (TOSCA-3) and state shame (ESS) were negatively correlated with self-esteem and quality of life. After controlling for depression, guilt-proneness (TOSCA-3) was only weakly negatively correlated with self-esteem and quality of life. Among women with borderline personality disorder and women with social phobia, after controlling for depression, anger-hostility (SCL-90-R) was positively correlated with both shame-proneness (TOSCA-3) and state shame (ESS), but not significantly correlated with guilt-proneness. To examine correlations with “guilt-free” shame-proneness (TOSCA-3), we controlled for guilt-proneness and depression in partial correlations (
Table 4 ) and found that “guilt-free” shame-proneness remained significantly negatively associated with self-esteem and quality of life and significantly positively related to anger-hostility. However, “shame-free” guilt-proneness was no longer associated with self-esteem or quality of life after controlling for shame-proneness and depression (
Table 4 ).
Discussion
In this study, shame-proneness, state shame, and shame-related implicit self-concept were assessed in women with borderline personality disorder as compared with women with social phobia and healthy women. The results supported our first hypothesis, that women with borderline personality disorder score higher in shame and shame-proneness than both women with social phobia and healthy women. This finding is consistent with the clinical experience of shame being a core emotion in borderline personality disorder
(2,
4,
14,
36) . By comparing women with borderline personality disorder and women with social phobia, our study design was conservative; women with social phobia are likely to be shame-prone because of fears of humiliation and devaluation, which are core DSM-IV features of the disorder. Given empirical research suggesting that guilt can be an adaptive emotion and is not necessarily related to psychopathology
(12,
23), our finding that women with borderline personality disorder did not have higher levels of “shame-free” guilt-proneness than the comparison groups is plausible.
Consistent with our second hypothesis, at an implicit level women with borderline personality disorder associated themselves as strongly with shame as with anxiety. In contrast, women with social phobia and healthy women had stronger implicit associations between self and anxiety than between self and shame. The small size of the observed group differences is not surprising because the IAT is a relative measure of strengths of associations (shame versus anxiety) and because both anxiety and shame were higher on self-report measures in the borderline personality disorder group than in the other two groups. Given our finding that women with borderline personality disorder associate themselves equally strongly with shame and anxiety and show high levels of anxiety and shame as well as anger-hostility in self-report measures, it may be characteristic of persons with borderline personality disorder to experience emotional difficulties across a wide range of negative emotions. By contrast, persons with social phobia may have more circumscribed, anxiety-related emotional difficulties. The general lack of correlations between IAT scores and explicit measures of shame and anxiety supports the notion that explicit and implicit aspects of shame reflect different levels of cognitive and emotional processing and should be assessed separately
(5) .
Our findings also confirmed our third hypothesis, that shame may be an especially debilitating emotion in that it was associated with low self-esteem, low quality of life, and high anger-hostility. The latter correlation suggests that shame-proneness may contribute to anger and hostility, which are common in borderline personality disorder. A shame-related implicit self-concept as assessed by the IAT was negatively correlated with both self-esteem and quality of life, supporting the validity of this IAT as well as the notion that a shame-prone implicit self-concept has a negative impact on the individual.
Implicit associations are thought to represent automatic structures in memory and to underlie maladaptive cognitive schemata. Through the influence of implicit cognitive schemata on both perception and behavior, persons with a shame-prone self-concept may demonstrate low self-esteem and high anger and impulsivity. In borderline personality disorder, the strong implicit association of self with shame may result from traumatic and humiliating experiences in childhood. Our findings suggest that prominent features of borderline personality disorder are related to explicit and implicit shame, which is not easily consciously accessible. This result has implications for psychotherapeutic treatments, from both a cognitive behavior
(2) and a psychodynamic perspective
(14,
36) . The failure to recognize shame within the patient-therapist relationship and the central role of shame in the patient’s inner experience jeopardizes the success of any psychotherapy, whatever its theoretical background. Our empirical results highlight the importance of designing psychotherapeutic strategies that target both explicit and implicit aspects of shame.
This study has some limitations. Because only women were included, possible gender differences remain unclear. The fact that some women with borderline personality disorder suffered from comorbid social phobia may have blurred the distinction between the two groups. However, high comorbidity rates closely reflect clinical reality in borderline personality disorder and increase the external validity of this study. Finally, any conclusions based on the IAT are limited because this instrument does not provide an absolute measure of the implicit association between self and a single target concept. In future studies, one approach may be to use various IATs, thus allowing researchers to determine the association between self and anxiety (versus calmness) and between self and shame (versus pride). This might help to disentangle the specific associations between self and shame versus self and anxiety.
The role of inpatient versus outpatient status should be controlled as well as the level of impairment due to mental illness. The importance of shame for self-injurious behavior and for the experience of rage and anger needs to be further explored by comparing the respective patient subgroups. In this study, only four women with borderline personality disorder did not engage in self-injurious behavior, which is too small a sample for formal analysis. Longitudinal studies could inform us about whether shame and implicit self-concept change over time, since implicit fear has been shown to be amenable to change during therapy
(37) . Studying other clinical groups, such as patients with depression or schizophrenia, would enhance our understanding of the role of shame in different disorders.
In summary, our study provides the first empirical evidence of the prominence of shame in borderline personality disorder at explicit and implicit levels. Moreover, strong correlations between shame and core clinical concomitants of borderline personality disorder, such as poor quality of life, low self-esteem, anger, and hostility, were demonstrated. This lends empirical support to the clinical experience of shame being a core feature in borderline personality disorder and to ancient knowledge that shame can wreak havoc in an individual’s life—as exemplified, for instance, in Sophocles’ tragedy
Ajax (38) . Future research needs to further examine the role of shame in borderline personality disorder and its relation to anger and impulsive behavior as well as to develop psychotherapeutic strategies to address shame-proneness.