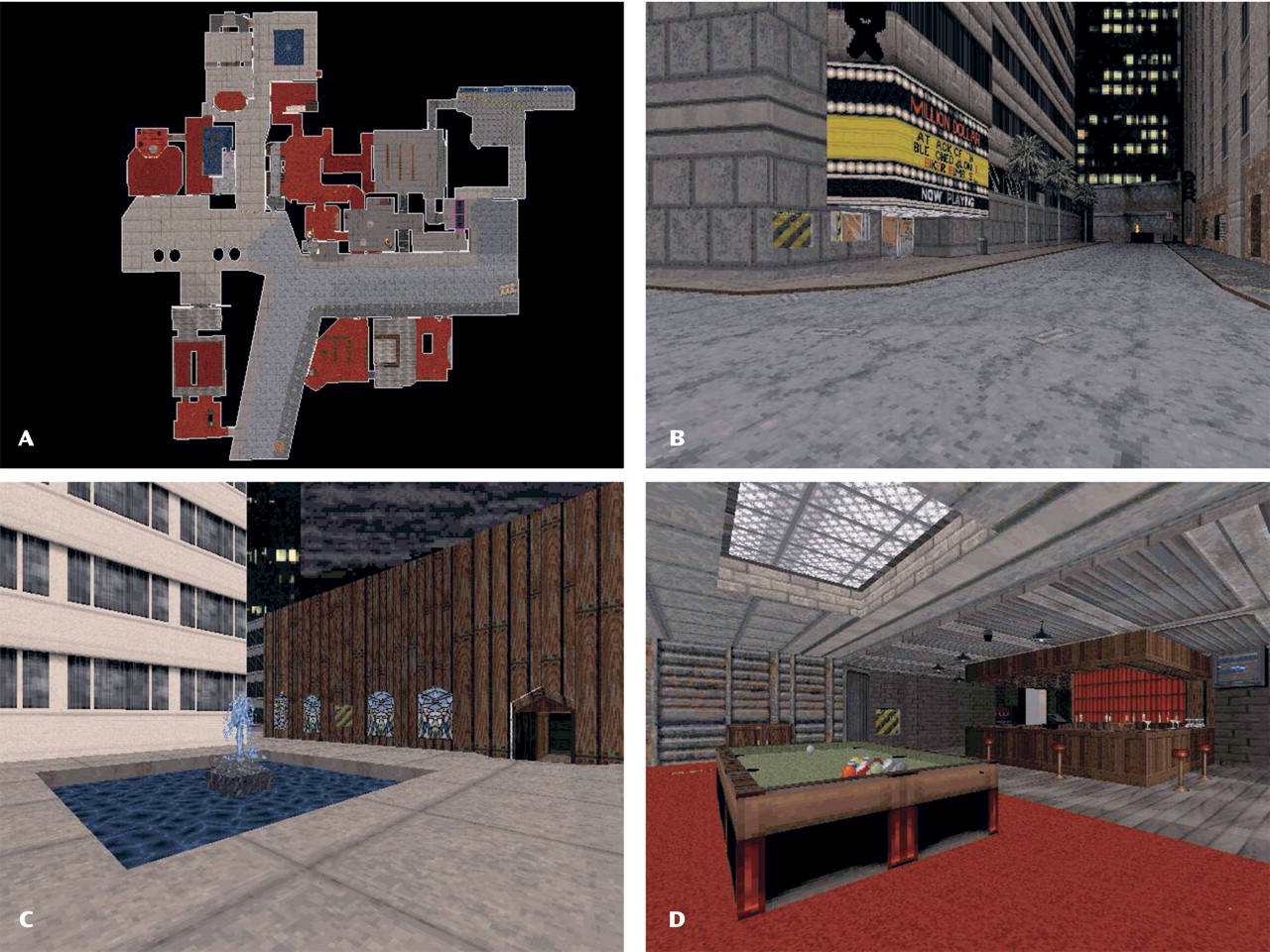
The depressed patients performed significantly worse than the healthy comparison subjects on a novel virtual reality measure of spatial memory, which uses a navigation format based on virtual reality
(13) . This difference was manifested through a lower number of locations found in the task. An important finding was that, while performance on the navigation task was correlated with performance on the Spatial Working Memory task, the patients and comparison subjects did not differ in performance on the Spatial Working Memory test. Differences detected on the virtual reality task suggest that it may be a sensitive measure of hippocampal-related spatial memory deficits and may more clearly elucidate the relationship between depression and this cognitive domain. Thus, despite the fact that the present task is more involved than existing measures, such as the Spatial Working Memory task, it has the advantage of detecting performance deficits in depressed subjects. Prior research has demonstrated a robust correlation between engagement of the hippocampus and the dependent measure used in this study
(14) . Because of the role of the hippocampus in this task
(11 –
14) and studies suggesting hippocampal volume reduction in depression
(4 –
7), it is reasonable to speculate that the patient deficit being measured is dependent on altered hippocampal function, which was not detected on the Spatial Working Memory test. However, while this task has previously been shown to involve the hippocampus and require normal function of the hippocampus, we cannot be certain that the differences on this task that we observed in the depressed patients are due to altered function of the hippocampus (as opposed to other brain areas that could be involved). The incorporation of additional control measures that target various structures within the medial temporal lobe will be necessary to more clearly delineate the neuroanatomical structures involved in the task performance. Nevertheless, our results suggest that spatial memory performance on a virtual reality navigation task may represent a quantifiable endophenotypic measure to assess possible hippocampal deficits in patients with depression
(1,
16) . This hypothesis can be further confirmed by applying spatial memory tests with a virtual reality navigation format to euthymic patients, unaffected first-degree relatives of depressed patients, and medication-free bipolar patients, in order to assess the cognitive effects of mood stabilizers, and by correlating performance with structural and functional neuroimaging measures of relevant structures, such as the hippocampus.