American psychiatry is beginning a review process that will culminate in a revision of our diagnostic manual. An early step in the DSM-V planning process was the publication of
A Research Agenda for DSM-V (1) . One goal of the agenda was to stimulate research and thinking that might support the development of a new paradigm for diagnosis and classification. The chapter titled “Basic Nomenclature Issues for DSM-V”
(2) provided a brief analysis of mental disorder and called for further conceptual work in this area.
This article extends the work begun in the agenda by offering both a broader and a more detailed analysis, focusing specifically on issues that underlie the idea of a medical-psychiatric nomenclature itself. The current paradigm for the medical model in psychiatry is arguably more complicated than the four models discussed in the agenda.
In the first part of this essay, we summarize six critical dimensions of psychiatric classification. In the second part, we use these dimensions to compare and contrast a range of leading models of psychiatric disorder. In the third part, we make some suggestions for how psychiatrists and their critics should conceptualize the complicated problem of classification during the development of DSM-V. In agreement with the cautious approach adopted by the authors of the “Basic Nomenclature” article, our purpose is one of explication and exploration, not resolution.
Dimensions of Categorization
Theories about scientific categories, such as psychiatric disorders, can be complex because they often contain a range of assumptions about what counts as real, valid, relevant, and useful. They also often assume different notions about the nature of causal processes in psychiatric illness. Many of these differences can be summarized in a modest list of overlapping dimensions.
Causalism Versus Descriptivism
Should psychiatric disorders be categorized as a function of their causes ( causalism ) or their clinical characteristics ( descriptivism )?
From the time of Koch’s postulates, medical thinking has commonly assumed that the ultimate test of a “true disorder” was the discovery of a discrete and unique cause. However, the application of this criterion to psychiatric illness has been problematic. For example, does ignorance regarding the causes of major depression or autism mean that they are not legitimate medical disorders? In contrast to the causal position, many professionals hold that an accurate description of a condition’s signs, symptoms, course, and typical outcome are sufficient to legitimize its status as a disorder
(3) . Pragmatically speaking, when psychiatrists cannot agree on what counts as a satisfactory causal hypothesis, a descriptive approach allows them to agree on what counts as a legitimate disorder.
At least three different approaches can be taken to the role of
causalism in psychiatric nosology. One position, best described as “temporizing,” suggests that “We will have to settle for descriptive approaches until we understand the real causes of psychiatric illness.” The second position, a “robust descriptivism,” rejects
causalism in principle as a useful nosologic approach for psychiatry, asserting that the causal structure of psychiatric illness is so complex, resulting from the actions and interactions of many individual causes, each typically of small effect, as to be useless to solve nosologic questions. The causal model, they would argue, rooted in infectious diseases with one clear etiologic agent, is simply inappropriate for complex conditions such as psychiatric disorders. A third, intermediate position argues that despite the complexity of the causes of psychiatric illness, one particular class of casual factors (e.g., genes, neurochemistry, structural brain changes) might, for practical reasons, be given priority when we make particular nosologic decisions
(4) .
Essentialism Versus Nominalism
Are categories of psychiatric disorder defined by their underlying nature ( essentialism ), or are they practical categories identified by humans for particular uses ( nominalism )?
An essentialist believes that psychiatric disorders exist independent of our classifications and the job of nosologists is to discover their inherent natures and classify them accurately. Essentialist models have been powerfully applied to other areas of human endeavor; for example, in chemistry, individual elements such as gold or oxygen appear to be entities that share the same underlying properties
(5) . Advocates of essentialism claim that legitimate psychiatric disorders are, like gold and oxygen, part of the inherent structure of the universe and taxonomies should represent that structure as it exists in itself.
There are two approaches to nominalism. A
radical nominalist argues that we must pick our categories for their use, with no expectation that they will reflect deeper truths about the world. A
moderate nominalist, by contrast, agrees that there is some structure of psychiatric illness in the world but there is no one unique categorization that stands above the others on a priori grounds
(6,
7) .
Advocates of moderate nominalism suggest that the world is heterogeneous, and therefore, classification requires highlighting some features of the world and minimizing others. The development of a classification system involves discovering facts about disorders that allow us to lump, split, weight, and order them for particular purposes
(8) . Moderate nominalists agree that we discover things about psychiatric disorders rather than invent them, but they also argue that there are multiple ways to divide up the disorders, and no one way has universal priority for all purposes. Categorization requires decision as well as discovery.
Objectivism Versus Evaluativism
Is deciding whether or not something is a psychiatric disorder a simple factual matter (“something is broken and needs to be fixed”) ( objectivism ), or does it inevitably involve a value-laden judgment ( evaluativism )?
Proponents of objectivism argue that evaluations of good and bad are not relevant to deciding whether something is broken. Objectivists would agree that evaluating a condition as bad is what motivates our interest in studying it, but once that initial evaluation is made, we can proceed to study the condition factually—in a value-free manner. A key aspect of the objectivist approach is the notion of
natural function . For example, eyes are designed by evolution for seeing, and legs are designed for walking, and if those natural functions cannot be performed, then something is broken
(9) .
Although it is possible for objectivists to tell a convincing story about what counts as a natural cognitive-emotional function, it is difficult to confirm that story. For example, does paranoid personality disorder represent a breakdown in natural psychological function, or it is a normal variation in design that is maladaptive in certain contexts
(10) ? Without hard evidence regarding the design of the emotions and social cognition, intuitions about what counts as “dysfunctional suspiciousness” might depend on value judgments about what counts as normal and adaptive
(11) .
By contrast, the evaluative position holds that both health and illness are inherently value-laden concepts. Being depressed because one has forgone meaningful relationships in favor of working long hours to get promoted might be a natural state, but we may try to disrupt that state with antidepressants to create a less natural state that we value—happiness. These thinkers believe that the regulatory role played by our notion of health guarantees that values cannot be eliminated from the practice of psychiatry, and it is a mistake to pretend otherwise
(12) . Disease, disability, and suffering are evaluated as bad, and their badness is understood in relation to some model of health.
How do we respond to historical claims that slaves who had a compulsion to run away and advocates for change in the former Soviet Union were mentally ill? An objectivist would claim that those classifications contained bad values and progress was made when those values were eliminated. Their opponents would claim that the elimination of bad values is not the same as becoming value-free, and progress has been made by adopting better values. Proponents of the evaluative approach would also point out that “values” do not have to be inchoate, fuzzy, or undefinable. For example, in the DSM-IV-TR appendix, the Global Assessment of Relational Functioning Axis can be seen as an attempt to operationalize psychiatric values.
Internalism Versus Externalism
Should psychiatric disorders be defined solely by processes that occur inside the body ( internalism ), or can events outside the skin also play an important (or exclusive) defining role ( externalism )?
Advocates of internalism hold that events inside the body are critical for understanding and defining disorders and external events are at most of secondary importance
(13) . Such internal variables might include frontal lobe deficiencies, lowered levels of serotonin, altered proteins, an inability to tolerate a negative affect, or a lack of appreciation that other people have a unique subjective perspective. Both modern psychiatry and psychology have largely adopted an internalist perspective in their focus on events inside the body or
inside the head .
Externalists come in two sorts. Radical externalists hold that understanding internal events is less relevant than understanding what is happening or has happened outside the skin. This approach is seen in the historical constructs of reactive depression or psychogenic psychosis and the current diagnosis of posttraumatic stress disorder, conditions in which external events are seen as definitional. Such an approach is also seen in eating disorder research in which these syndromes are considered to be reactions to harsh societal demands for an unrealistic feminine body shape. Cross-cultural approaches are also firmly externalist. Externalist thinkers are inclined to view internal nature as a constant and, therefore, attribute differences between people to environmental influences.
More moderate externalists adopt an interactive approach in which what goes on inside the head cannot be isolated from an organism’s interaction with the world
(14) . Just as in general medicine, a moderate externalist would see heart disease in cigarettes and French fries, in psychiatry, a moderate externalist would be interested in finding out about precipitants in order to understand a case of depression and believe that the precipitants hold some relevance for treatment in the long term. Although they view external factors as being much more than secondary considerations for understanding disorders, moderate externalists still accept that internal events are important individual difference variables. For example, the effects of trauma may be mediated by internal vulnerability factors or by internal protective factors. External events alone do not explain outcomes.
Entities Versus Agents
Should psychiatric disorders be considered to be “things” people get, or are they inseparable from an individual’s personal subjective makeup?
A diamond is an entity. Entities are things that are generally uniform from case to case. Entities also exist in networks of lawful relationships that can be scientifically described. A person is an agent. Agents are dynamic. They have purposes and intentions that make them unique.
The entity viewpoint has become ascendant in American psychiatry since the publication of DSM-III. To illustrate, major depression is considered to be some pathological thing that patients get. It invades their lives and cannot be diagnosed until the normal process of grief has been excluded. By contrast, DSM-I, as influenced by Adolf Meyer, was more amenable to an agentic viewpoint because most disorders were conceptualized as individual “reactions” and, in many cases, the expression of one’s character. From the agentic perspective, each psychiatric disorder as manifest in an individual patient is relatively unique.
Those who adopt an entity perspective typically view individuals as
vehicles for pathological syndromes and engage in scientific research that seeks to discover what makes syndromes the same from case to case. In contrast, proponents of the agentic perspective attempt to focus on persons more than on patients
(15) . They would be more likely to claim that someone diagnosed with chronic dysthymia who views himself as a deep person and actively rejects moments of lighthearted happiness is more than a vehicle for some entity called
dysthymia .
Categories Versus Continua
Are psychiatric disorders best understood as illnesses with discrete boundaries ( categorical ) or the pathological ends of functional dimensions ( continuous )?
Proponents of the categorical viewpoint in psychiatry argue that discrete categories, such as gophers and chipmunks, are defined by nonarbitrary boundaries between those inside and outside the category. Members and nonmembers of a discrete category are said to be qualitatively distinct. For these thinkers, carving nature at the joints means finding the discrete parts or “bones.”
Proponents of the categorical or “taxonic” approach hold that medical conditions, such as infectious diseases, cancer, and degenerative neurologic disorders, are discrete categories. Not only are they distinct from each other as illnesses but each one of them is clearly distinct from the state of health. Psychiatric disorders, they claim, should be seen in this same way. Kendell and Jablensky
(16) proposed that these kinds of categories should be called “valid” and suggested that they are rare in psychiatry.
Proponents of a continuum viewpoint, by contrast, note that a category such as “tall” is not an objective class. There exists an objective continuum called height that runs from low to high, but on this continuum, the difference between short and tall is quantitative. It is a difference of degree rather than a difference in kind. For continuum proponents, identifying a category is more like slicing a meatloaf.
Proponents of the continuum perspective point to medical disorders, such as hypertension and osteoporosis, as more realistic models for psychiatric disorders. Like these conditions, they argue that psychiatric disorders can be best defined as transition points on a continuum of physiological or mental functioning.
Some continuum thinkers would claim that the lines between disorders and nondisorders are inherently arbitrary
(17) and what are really there are the underlying continua. They are often called “dimensional” model proponents. Others would say that the boundary, while fuzzy, can be meaningfully defined by that region on a continuum in which specific values are reliably associated with harm
(18) . They would say that groups of cases that lie on a high or a low end of a continuum can be considered to be “legitimate” groups and should not be devalued as “arbitrary.”
Models of Psychiatric Disorder
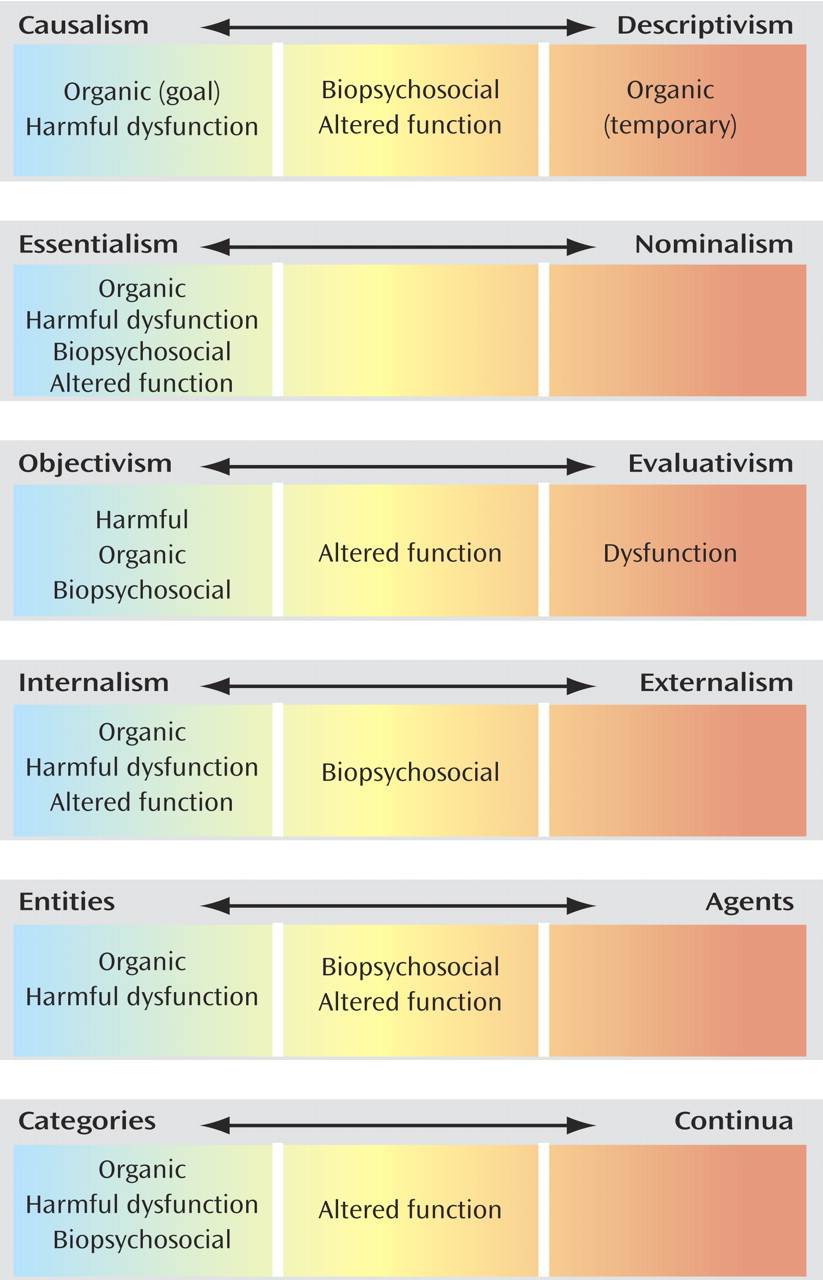
In the next two sections, we review some prominent models of psychiatric disorder, characterizing the key features of these models with respect to the dimensions articulated above. These models are likely to be familiar to readers and illustrate the conceptual dimensions in applied form. We first describe four versions of the medical model termed, respectively, the organic disease model, the altered function model, the biopsychosocial model, and the harmful dysfunction model. We outline in
Figure 1 the positions these models adopt on the six dimensions described above. In the second section, we describe several alternative models of psychiatric disorder.
Four Versions of the Medical Model
The Organic Disease Model
This version of the medical model arose in association with the germ theory of disease and gained widespread acceptance by the mid-19th century. As applied to psychiatry, this organic disease model states that psychiatric disorders are due to pathological processes in specific parts or systems of the brain. Both the historical and current advocates of this model stress the affinity of psychiatry to neurology and typically view psychiatry as “applied brain science.” They view neurologic disorders, such as general paresis of the insane, Alzheimer’s disease, and Huntington’s disease, as good models for psychiatric disorders and emphasize the discontinuity between disease states and variations in normal functioning. The underlying pathological process is often considered to be the essence of the disorder.
The Altered Function Model
Several trends in medicine in recent decades have highlighted limitations of the organic disease model. “Diseases” such as essential hypertension, osteoporosis, and multifactorial hypercholesterolemia have been characterized and are now a major focus of treatment. Such conditions seem to fit poorly into the organic disease model because they are not discrete, apparently reflecting one end of a “normal” physiological continuum. Physicians also began to manage conditions from pregnancy to “tennis elbow” that reflect normal alterations of functioning that could, under some circumstances, develop into health risks
(19) . These new “conditions” also did not fit well into the framework of the organic disease model, which assumed that each disorder had an abnormal etiology and/or a clear-cut pathology. These and other trends gave rise to an
altered function model in which some “condition of altered functioning is a threat to health,” making future suffering, death, or disability more likely.
The Biopsychosocial Model
Another shortcoming of the organic disease model is that many psychiatric conditions cannot be reduced to an unambiguous biological pathology. The medical model’s focus on syndromes defined by some underlying pathology, however, is not exclusive to the organic model. It is also integral to the psychodynamic models that focus on unconscious processes, self-structures, and defense mechanisms and the cognitive models that focus on dysfunctional thoughts and beliefs.
Rather than limiting itself to one domain of causality, Engel’s biopsychosocial model highlights the possibility of considering a plurality of casual factors, including those external to the organism. It gained widespread prominence just after the reemergence of the organic model in the late 1970s and held that even when biological factors are clearly shown as the primary causal variables, psychological and social factors still have a role to play in successful treatment
(20) . The biopsychosocial model also provided theoretical support for the development of a descriptive psychopathology that could be accepted by those holding different theories about the nature of the underlying pathology and focusing on patients as persons.
The Harmful Dysfunction Model
In the 1960s, Szasz
(21) argued that there is no such thing as a legitimate mental illness. Adopting a view akin to a narrow organic disease model, Szasz claimed that in the absence of unambiguous biological causes, the identification of psychiatric disorders reflected value judgments about undesirable beliefs and behavior. He claimed that “undesirableness” was typically articulated from the perspective of a particular social class (the middle class) and a particular political-cultural viewpoint (Western individualism). Szasz argued that problems in living were being misclassified as illnesses.
In response to these challenges, Wakefield
(22 –
24) articulated the harmful dysfunction model. Its purpose is to help professionals differentiate legitimate psychiatric disorders (such as conduct disorder) from unpleasant conditions that are not disorders (such as adolescent rebellion). According to the harmful dysfunction model, an attribution of a mental disorder has two components, the first of which is
harmfulness, meaning that the behavior is maladaptive for the individual. “Maladaptive” refers to a devalued condition or a problem in living. The second component is
dysfunction, meaning that something has gone wrong with the organism’s cognitive-emotional-perceptual machinery. The organism is not functioning the way in which evolution designed it to function.
In this model, the presence of an objective pathological process (dysfunction) is necessary but not by itself sufficient for the attribution of a disorder. The attribution of harm is also necessary. To illustrate, two individuals might experience a similar degree of elevated anxiety and the same number and severity of panic attacks. However, one individual channels the anxiety into achieving important goals and interprets the panic attacks as signals to slow down, whereas the other person uses the anxiety as a reason to avoid striving for goals and considers the panic attacks to be random events that reinforce a sense of futility. Whereas the first avoids harmful consequences, thereby remaining healthy, the second individual experiences harmful consequences, thereby becoming disordered.
Comparing the Medical Models With Respect to the Dimensions
Although descriptions of medical models are rarely explicit about assumptions regarding classification, inferences about those assumptions can be made. Based on these inferences, we have sorted the four medical models with respect to the dimensions. Congruent with psychiatry in general, all of the models view categories of psychiatric disorder as things to be discovered (
essentialism ). The organic disease, harmful dysfunction, and biopsychosocial models have traditionally sought to discover discrete categories, whereas the altered function model has supported continua or categories. The biopsychosocial model is less committed to viewing disorders as occurring inside the patient than the other three models. With slight variations, the existence of internalistic essentialist categories could be considered a common assumption of these four medical models. Although none of the medical models appear to adopt nominalism, they differ with respect to whether they hold that disorders should be defined by their causes or by their symptom pictures and whether the presence of a “disorder” is a matter of fact or also involves a negative value judgment. A visual representation of the medical models with respect to the dimensions of categorization can be found in
Figure 1 .
Alternative Models of Psychiatric Disorders
In the following section, we describe several alternative models of psychiatric disorder that adopt positions on the dimensions of categorization not taken by the medical models just described. These models form a varied lot, and the arguments for them can be complex. We will be more illustrative than complete in our descriptions.
Two Different Uses of Nominalism
Recent debates about the nature of psychiatric disorders have focused a great deal of attention on the essentialism-versus-nominalism dimension, with some cogent arguments favoring the adoption of more nominalist assumptions. We will describe two nominalist analyses that have emerged in these debates. In the first, nominalism is used as a strategy of criticism based on the assumption that nominal categories are scientifically illegitimate. In the second, it is argued that the scientific approach supports nominalist approaches to classification.
Dimensional Models
Through the years, many thinkers have questioned whether a categorical model of disease entities is an appropriate framework for psychiatric classification
(25) . They point out that certain categories of psychiatric disorder are inherently heterogeneous and overlapping. Because the categories of psychiatric disorder are not discrete kinds, such as gold and oxygen, they are not considered to be legitimate “natural kinds.”
Recent proponents of this “category skepticism” argue that the categories postulated by architects of psychiatric diagnostic systems are “arbitrary” and “manmade,” whereas various underlying dimensions, such as
neuroticism, are considered to be akin to the architecture of universal human nature and grounded in biology, not culture
(26 –
28) . The most fertile recent ground for these category skeptics has been the personality disorders. They believe that the categories of personality disorder do not carve nature at the joints, but the underlying dimensions do. These “dimensional” thinkers are nominalists about categories and essentialists about continua.
Although they are a diverse group, the dimensional proponents state that a category of personality disorder is a family of personality types with differing degrees of severity. For example, because only four of eight criteria are required for diagnosis, there are many different ways to have a compulsive personality. They claim that psychiatrists are asked to make a decision about whether a personality disorder is present or absent, and in this process much information is lost . Compulsiveness, they note, is not really an either/or phenomena; it really exists in degrees.
The Practical Kinds Model
Proponents of the practical kinds model claim that the notion of a “case” in medicine implies a group of some kind. They agree that we lose information about individuals when we classify them into groups but also suggest that we gain information about individuals by classifying them as the same kind of thing. We learn more about “schizophrenia” by studying commonalities between particular cases of schizophrenia; it increases our ability to successfully treat people in that group. This definition of a “good group” might also apply to depression, antisocial personality disorder, and panic disorder.
In contrast to the dimensional model proponents, advocates of the practical kinds model claim that we should not judge what counts as an adequate psychiatric disorder with reference to something such as gold, a category considered to have an unambiguous essence along with discrete boundaries. Beginning with Darwin, many biologists stopped thinking of species as if they were like elemental categories in physics and chemistry
(29 –
31) . Darwin considered a species to be a population of individuals that vary from each other and that typically have fuzzy boundaries. Both Zachar
(32) and Ghaemi
(33) suggest that psychiatry should adopt a concept of a group that is more akin to a Darwinian species than a chemical element. In addition to an exponent of practical kinds, proponents of ideal types
(34), prototypes
(35), and exemplars
(36) also advocate a nominalistic approach.
The practical kinds proponent specifically says that most psychiatric disorders are heterogeneous things, and decisions about where to draw the lines between cases and noncases require a judgment that has to weigh many factors. Over time, different priorities may come in and out of favor with respect to making these judgments.
If a psychiatric disorder, such as depression, is considered to be a cognitive-emotional state that inhabits a particular region on a larger
continuum of mood, psychiatrists obviously have to decide where to draw lines
(37) . In addition to discriminating depressed from nondepressed individuals, they can draw lines between mild and severe cases. The practical kinds model holds that additional information external to the mood continuum itself might also lead psychiatrists to distinguish chronic and acute cases or anxious and nonanxious cases. There are many possible good groups to identify relative to this continuum.
If a disorder belongs to a
discrete category, that category can still be heterogeneous or “broad”
(38) . Practical considerations often motivate psychiatrists to define narrower categories that are coherent enough to be considered distinct from each other. For example, in some theories, a genetic category called “schizophrenia spectrum disorder” is often decomposed into coherent groups, such as schizophrenia, schizoaffective disorder, other nonaffective psychoses, and schizotypal personality disorder. Decisions about where to draw lines are still made.
The practical kinds model claims that although choosing DSM categories requires an evaluation that considers a multitude of priorities, we can still choose them on rational grounds. These grounds will include both scientific and practical values, such as predicting treatment, maximizing true positives and minimizing false negatives, being clinically informative, and reducing stigmatization. Given all the competing interests involved, psychiatrists should not expect to identify a single scheme of categories that works for all purposes or satisfies all potential users.
Two Approaches Advocated by Medical Model Critics
To provide a fuller picture of the relevant landscape, we will also describe two models that adopt positions on our dimensions at variance with those taken by the medical models. To differing degrees, these models are more externalist and agentic than those previously reviewed in this article.
The Interpersonal Model
Contrary to any of the medical models, an interpersonal systems model is staunchly externalistic. Most fundamentally, this model views disturbed behavior as arising from disturbed relationships. Rather than deriving from psychopathology in individuals, psychiatric disorders are seen to develop dynamically from pathology in interpersonal contexts. The notion of patients being containers of internal psychological states is minimized, whereas the view of them as persons trying to adapt to their social worlds is maximized
(39) . The context or the interpersonal system is both locus of pathology and the cause of pathological behavior.
Taking this model further could involve defining relationships themselves as disordered. The idea here is that some kinds of marital and child-parent problems cannot be reduced to the psychopathology of one or both participants; rather, they emerge in the unique relationship between them
(40) .
The Narrative Approach
The narrative approach, probably the most “radical” here considered, claims that a focus on the causal
explanation of disorders minimizes the importance of
understanding disorders. “Understanding” refers to interpretation and the discovery of meaning. Proponents of the narrative approach
(41,
42) believe that information about conditions such as depression, bipolar disorder, and schizophrenia is not contained in lists of diagnostic criteria or in DSM text but can be found in narrative accounts. Examples of narratives include works by writers such as William Styron
(43) . Also important are case study reports by patients and mental health professionals, such as the famous memoir of Schreber
(44) and related commentaries
(45,
46) . These formats are supposed to bring disorders to life in contrast to the lifeless lists contained in diagnostic manuals.
Focusing on patients’ experiences, the narrative approach also claims that psychiatric disorders can be distinguished with respect to how patients understand themselves and their relationships. There are, for example, narcissistic scripts, paranoid scripts, and dysthymic scripts, all of which can be described systematically. To illustrate, the person with chronic dysthymia tells “poor me” stories in which they are burdened, others are lucky, and the future looks bleak. Rigid adherence to this narrative partly constitutes dysthymia.
The narrative approach is more widespread than is often recognized. Any theoretical model that considers the role of the self in psychopathology has at least one foot in the narrative camp, primarily because understanding the self involves personal stories
(47) . The same is true for theories that conceptualize psychiatric conditions in the context of normal developmental issues, such as identity and autonomy
(48) .
Implications for DSM-V
We have outlined what may seem to be a confusing array of dimensions along which to view models of psychiatric disorder and then reviewed a range of leading models. In line with our descriptive goals, we have tried to present these dimensions and models in a balanced manner. The critiques of models reviewed here were made to clarify differences between opposing poles on the dimensions of categorization.
Although this essay has focused on a taxonomy of “psychiatric disorders,” in agreement with Haslam
(49) and McHugh and Slavney
(15), we do not in fact believe that the same conceptual approach is likely to be ideal or even appropriate for all psychiatric conditions. For example, some classes of psychiatric disorder may now or in the future be more usefully studied from an essentialist perspective, whereas others may be more appropriately viewed nominalistically. Before closing, however, we provide our own evaluation of the six dimensions.
Causalism Versus Descriptivism
We are deeply skeptical that most psychiatric disorders can be unambiguously classified as a function of their causes because these disorders are profoundly multifactorial in origin. We reject as unrealistic the “temporizing” causal model because, as one of us has argued elsewhere, there are probably no more spirochetes left to be discovered for psychiatric illness
(50) . We may wish for single causes of large effect for psychiatric disorders that will permit us to have a clear, unambiguous etiologically based nosology. However, we regard such hopes as unrealistic. All evidence now suggests that psychiatric disorders typically arise as a result of multiple genetic risk factors added to and interacting with multiple environmental risk factors with no one risk factor being of overwhelming importance.
Although we are attracted to this “robust descriptivism,” we also see value in the intermediate position on causalism, which suggests that for practical reasons, certain classes of risk factors might be given priority in particular nosologic decisions.
Essentialism Versus Nominalism
We come down more on the nominalist side of this dimension, believing that most categories of psychiatric disorder are likely to be defined in response to human goals and purposes rather than simply discovered as entities out in the world. One possible advantage of accepting the nominalist position is that, as suggested by the practical kinds model, if there is no one “true” way to divide up the nosological landscape, then those creating a diagnostic system are free to use an approach that will maximize the use of their categorizations. Of course, this presents the problem of what kind of use should be emphasized. However, confronting this problem head on may be ultimately a more realistic approach than arguing that there is one “true” set of psychiatric diagnoses that we just have to work harder to detect and classify.
Objectivism Versus Evaluativism
Here we are more ambivalent. Some disorders, such as disorganized schizophrenia, in which reality perception is grossly impaired, are likely to resemble an objectivist model, partly because the value judgment that schizophrenia is harmful will be widely agreed upon. Other conditions, such as some forms of alcohol abuse, are likely to be more consistent with an evaluative perspective, and debates about the presence of an objective dysfunction will be more prevalent.
Internalism Versus Externalism
This dimension more than others is open to empirical inquiry. Here the results have suggested that both internal and external events are operating for virtually all psychiatric disorders although in differing degrees. In line with our position on the causal versus descriptive dimension, practical use should influence how much one or the other pole of this dimension is emphasized—and that will vary considerably from disorder to disorder.
Entities Versus Agents
Here we might suggest the following maxim: any good clinician will have to attend to the unique aspects of each case. These unique aspects also include personal factors. For better or worse, however, the diagnostic exercise is one of describing and categorizing entities. The medical model holds that studying and treating “things” called psychiatric disorders can make the world a better place. If psychiatry is going to pursue this goal in a systematic fashion, it has to define common objects of study.
Categories Versus Continua
Our intuition is that although certain psychiatric disorders may turn out to be discrete categories, this will be the exception and not the rule. For example, one of us
(37) failed to find discrete boundaries around the psychiatric disorder of major depression. Confirming the presence of a discrete category is also open to empirical inquiry
(49) . For the bulk of disorders, however, osteoporosis will prove a better model than pneumococcal pneumonia. Like Kendell and Jablensky
(16), we believe that these kinds of “useful” categories are invaluable, even though use varies from context to context.
Conclusions
In a discussion of the factors justifying constructs for psychiatric disorders, one of us previously noted that many important empirical questions arise after choosing a construct for a disorder. The fundamental task of deciding between different constructs requires nosologists to use more than empirical data
(51) . It requires what DSM-IV-TR calls “judgment.”
This problem includes not only choosing between wide and narrow definitions of a condition, such as schizophrenia, but also choosing between disorders, such as antisocial personality versus psychopathy or chronic dysthymia versus depressive personality disorder, or whether to recognize a compulsivity spectrum. Equally relevant to DSM-V, it applies to choosing between DSM and ICD definitions of disorders. Cross-culturally, differences between something such as depression, as defined in the United States, and neurasthenia, as defined in China, present similar difficulties.
Deciding whether the “chosen” constructs are best understood as entities, agents, internal, external, etc., further complicates an already thorny problem. The same is true for negotiating between an altered function model and a harmful dysfunction model or deciding whether to adopt a dimensional model. These are important issues and developing informed preferences for the various conceptual options requires more than conducting the right series of experiments.
Of course, it is unwise to prejudge what can and what cannot be formulated as an empirical question. The history of science is replete with stories of insightful researchers who found ways of testing questions that were previously considered untestable.
Studies of insightful thinkers, such as Copernicus and Darwin, clearly indicate that good scientists regularly use a mixture of observation, empirical research, and scientific values to make inferences about the phenomena of interest to them. Philosophers sometimes call this process “inference to the best explanation.” Richters and Hinshaw
(10) describe it as follows:
There are no absolute standards for establishing the validity or truth value of [inference to the best explanation]. [It] can be evaluated only as more or less justified on the basis of criteria such as consistency with known facts, explanatory coherence, and plausibility relative to rival interpretations. Thus, the plausibility of an [inference] is always tentative and may change over time as a function of new knowledge…or the availability of new rival explanations.
We believe that a model of psychiatric nosology more congruent with actual practices would emphasize the importance of “inference to the best explanation.” Nosology at its best requires the constant interaction between empirical evidence and clear conceptual thinking. For psychiatric diagnosis, it is vital to understand the limits of empirical evidence and realize that struggling with conceptual and philosophical issues is a legitimate and, indeed, necessary part of the nosologic process.
As psychiatry embarks on a new revision of its diagnostic manual, it has to pay attention to the evidence and respect the results of empirical research. However, it should not expect that these results alone can ever answer all of the more basic conceptual questions explored in this article. Practical reasoning and good old-fashioned logic still have a role to play in the development of a scientifically based classification. It is our hope that the DSM-V development process will devote sufficient attention to these broader issues commensurate to their fundamental importance in the nosologic process.