Neuropsychiatric symptoms of multiple sclerosis (MS) are prevalent and commonly overlooked. Neuropsychiatric symptoms are present in 60% of cases and are the first symptoms of MS in 2% of patients (
1). We present a case of a patient with long-standing psychiatric symptoms who was diagnosed with MS during an inpatient psychiatric admission for a bipolar disorder type 1 mixed episode with psychotic features. Additionally, we provide a brief review of the literature discussing psychiatric symptoms occurring comorbidly with MS.
Case
"Mr. H" is a 32-year-old man with a history of bipolar disorder type 1 and borderline personality disorder as well as alcohol, opioid, stimulant, and cannabis use disorders, severe in early remission. On a police custody order, he presented to the emergency department with visual hallucinations of blood and ghosts, hypersexuality, and persecutory delusions. He was admitted to inpatient psychiatry. This episode differed from his previous presentations due to new acute-onset hypersexuality, psychotic symptoms, and significant mood instability. Past presentations included insomnia, irritability, and dysphoria without psychosis. On admission, the patient had been abstinent from alcohol for 75 days, and a urine toxicology screen was negative for illicit substances. In the emergency department, a complete physical examination as well as a comprehensive metabolic panel test, CBC, a thyroid-stimulating hormone test, ECG, and urinalysis revealed no abnormalities.
From 2006 to 2015, the patient had at least 12 inpatient psychiatric hospitalizations, carried out six suicide attempts by overdose or self-inflicted laceration, and engaged in multiple high-lethality suicidal gestures, such as placing a firearm in his mouth. He began using alcohol at age 12, required morning alcohol drinking (eye-opener) by age 16, and had a history of delirium tremens. He started using cannabis at age 13, opiates at age 16, and cocaine and hallucinogens at age 20. Medication trials included antipsychotics such as aripiprazole, risperidone, and ziprasidone. Additionally, he had been prescribed valproic acid, for mood stabilization, and paroxetine. All medication trials were discontinued due to metabolic side effects and lack of efficacy. His medications at the time of his hospital admission included paliperidone palmitate (156 mg intramuscular monthly) (last administered 2 weeks before admission), topiramate (50 mg twice daily), and lithium (300 mg nightly).
Once admitted to inpatient psychiatry, the patient was placed on constant staff observation and was amenable to treatment with carbamazepine after lithium refusal. The carbamazepine dosage was increased until the levels were therapeutic. The patient's symptoms of hypersexuality and mood liability improved, although his psychotic symptoms remained. Antipsychotics were initially withheld, given his recent administration of long-acting paliperidone palmitate. However, this was reconsidered because his visual hallucinations remained. Before starting treatment with antipsychotics, the patient developed acute-onset urinary incontinence, right eye pain, and decreased peripheral vision. Ophthalmology and neurology were consulted, and he was diagnosed with optic neuritis and new-onset MS.
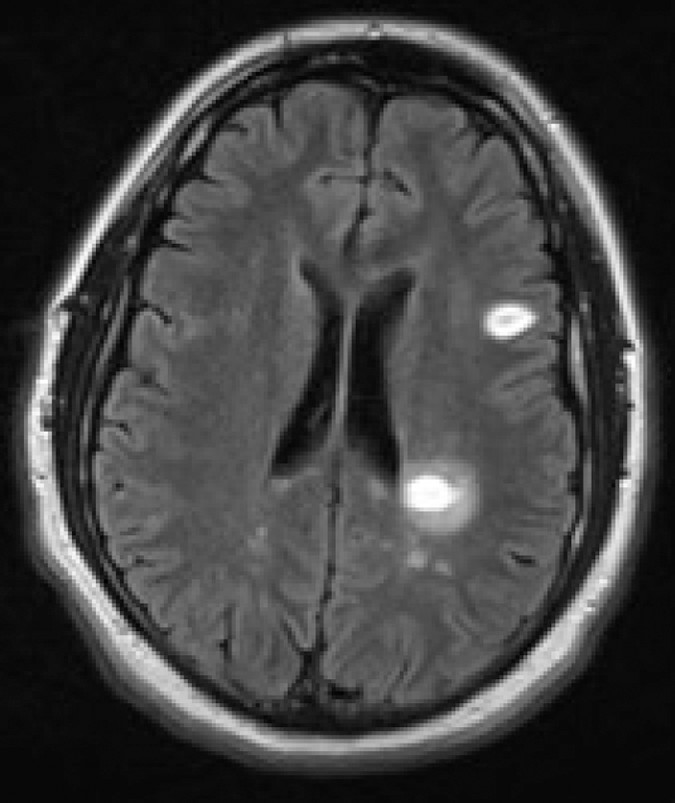
The patient was transferred to neurology. Neuroimaging revealed multiple cortical and cervical cord hyperintensity lesions (
Figure 1). Steroids were deferred during this hospitalization due to concerns of steroid-induced psychosis. The patient was treated with five sessions of plasma exchange. With these interventions, his psychosis, visual disturbance, and urinary incontinence resolved. After his discharge from the hospital, his diagnosis was characterized as relapsing-remitting MS. In outpatient treatment, his symptoms of urinary incontinence and vision loss recurred while he was maintained on teriflunomide (
2). Therefore, discussions were held between neurology and psychiatry regarding the risk of mania if treatment with steroids was started. Given the patient's past improvement of psychotic symptoms with treatment of MS, he was prescribed high-dose intravenous methylprednisolone for 5 days. He did not experience worsening of psychiatric symptoms and was successfully transitioned to monthly natalizumab infusions. At his most recent outpatient follow-up appointment, the patient remained psychiatrically stable.
Discussion
MS is the most common chronic neurologic condition affecting young adults (
3). Along with its significant prevalence, it can be present with a myriad of psychiatric conditions. Diaz-Olavarrieta et al. (
4) reported a 95% prevalence of psychiatric symptoms in patients previously diagnosed with MS. Specifically, patients reported experiencing dysphoria (79%), agitation (40%), anxiety (37%), irritability (35%), apathy (20%), euphoria (13%), disinhibition (13%), hallucinations (10%), and delusions (7%). Psychiatric symptoms were also observed more frequently during periods of quiescence (
4).
Bipolar disorder and MS are commonly comorbid, with most cases of mania developing later in the course of MS (
5). In contrast, in our patient worsening manic and psychotic symptoms were the heralding symptoms of MS. There are reported cases of MS presenting with exclusively psychiatric symptoms in patients who were diagnosed with MS by MRI during an organic workup for new-onset psychosis (
6). These patients also met criteria for bipolar disorder, similar to our patient, which included persecutory delusions, auditory hallucinations, and affect lability.
The above case is unique given the patient's stabilization and resolution of psychotic symptoms after MS treatment. The patient has not required psychiatric hospitalization and has been maintained on carbamazepine without an antipsychotic. It is noteworthy that in the aforementioned case reports, patients who presented with only psychiatric symptoms in the context of MS were middle age and female and had treatment-resistant symptoms and required extensive postdischarge care (including either 24-hour home supervision or care on a locked nursing home unit), and they had no abnormal findings on physical examination. It is also noteworthy that our patient presented with physical examination findings after his psychiatric symptoms worsened (
6). Future investigation into the discrepancy between physical examination findings, biological sex, age at onset, and long-term stability would be of clinical relevance. Our patient's postdischarge sobriety and his ongoing participation in psychotherapy likely contributed to his stability. His sobriety is notable given his history of addiction. His affective stability may be a contributing factor in his sobriety.
High-dose intravenous steroids were used during outpatient management despite the increased risk of manic or hypomanic symptoms that occur in patients with bipolar disorder and a history of substance abuse (
7,
8). This decision was made given our patient's past improvement of psychotic symptoms when treating MS. Only two case reports, to our knowledge, have shown worsening of psychiatric symptoms during treatment with teriflunomide and natalizumab (
9,
10). Therefore, it was deemed unlikely that these treatments would have worsened our patient's overall condition.