Hearing impairment currently affects approximately one in 1,000 newborns and can occur as a result of many known genetic and environmental factors (
1). There is a higher incidence of auditory hallucinations in adults with hearing impairments (16%) than in adults without hearing impairments (6%) (
2). One explanation is deafferentation and the resulting cortical hyperexcitability in the context of sensory deprivation. The proposed mechanism for this perceptual dysregulation is a compensatory lowering of cortical activation thresholds in the absence of afferent input, thereby destabilizing the neural networks responsible for processing and contextualizing sensory information. This phenomenon is thought to underlie Charles Bonnet syndrome, in which individuals with visual impairment develop visual hallucinations. Differences in underlying mechanisms of auditory hallucinations may predict antipsychotic treatment response. In fact, antipsychotics may have limited therapeutic effects in patients with auditory hallucinations that are attributable to deafferentation. In such cases, treatment often focuses on improving auditory acuity (
3,
4). In addition to dopamine, various other neurotransmitters have been implicated in auditory hallucinations in the hearing-impaired population, including acetylcholine, glutamate, and gamma-aminobutyric acid (GABA) (
5).
Deafness-infertility syndrome (DIS) is an autosomal recessive form of hearing impairment resulting from a contiguous gene deletion at chromosome 15q15.3. This deletion involves the STRC and CATSPER2 genes, which are responsible for the structure of stereocilia in the ear (
6) and for sperm motility (
7), respectively. DIS is characterized by prelingual, nonprogressive sensorineural hearing loss in individuals who are homozygous for the deletion and by infertility in males. DIS was identified as a distinct syndrome in 2002 (
8); to date, research on additional phenotypic correlations has been limited given the low prevalence of DIS. To our knowledge, there are no reported cases of auditory hallucinations associated with DIS. We describe a case of a female with DIS who presented with neuropsychiatric manifestations.
Case Presentation
A 19-year-old female with an unspecified psychotic disorder, migraines, and bilateral sensorineural hearing impairment secondary to DIS was brought to our inpatient psychiatry unit after being found at the edge of a bridge by a bystander. The patient reportedly feared for her life because she was experiencing distressing auditory hallucinations.
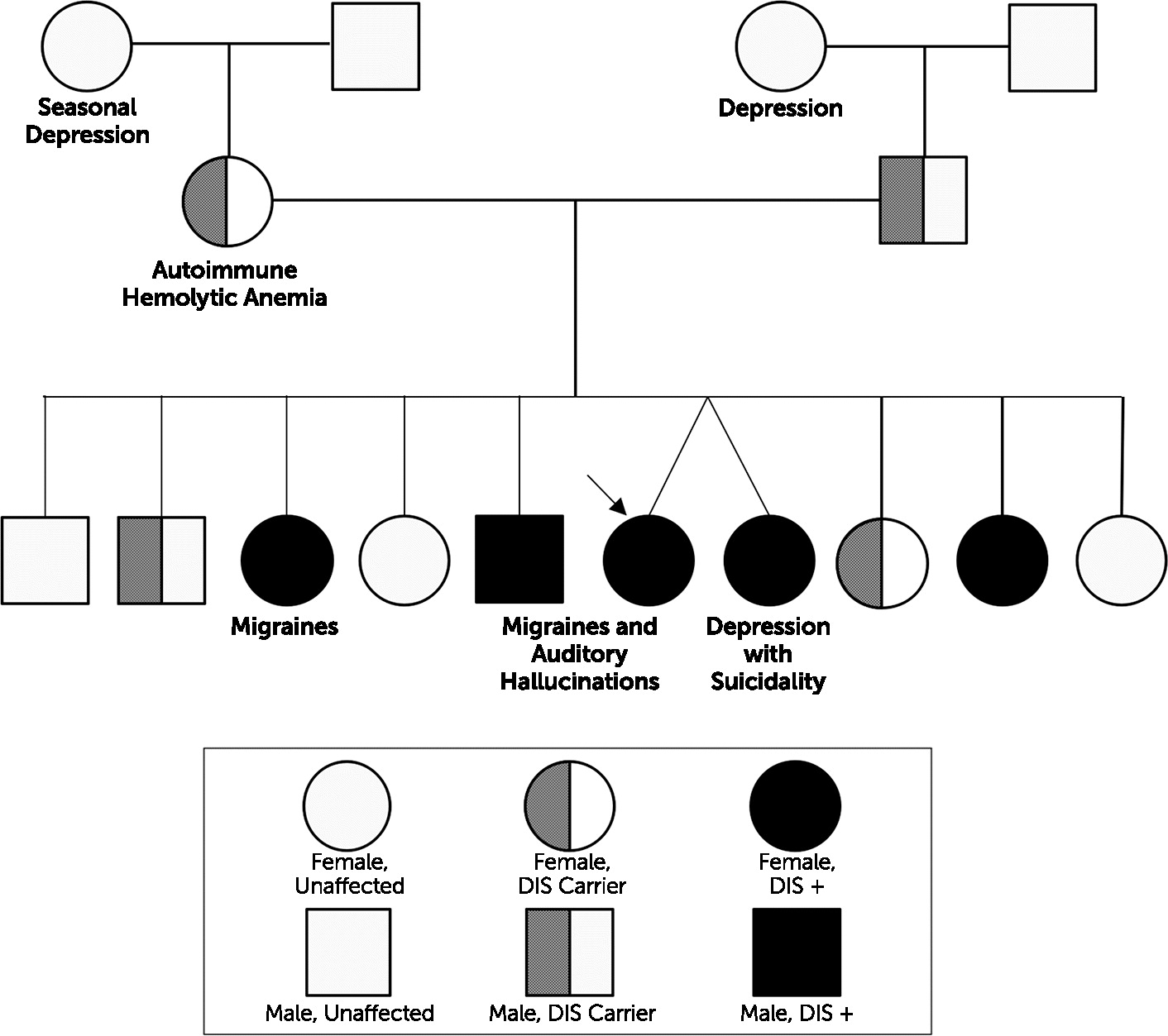
The patient was born to nonconsanguineous parents of mixed ancestry and shortly after was diagnosed with congenital bilateral sensorineural hearing loss requiring hearing aids. As a teenager, prior to the onset of her hallucinations, she developed migraines and dizziness of unknown etiology. This prompted an extensive genetic workup that was notable for a homozygous deletion on chromosome 15 spanning approximately 100,000 base pairs and involving the STRC, CATSPER2, and CKMT1B genes and possibly the PPIP5K1 gene. Additionally, a considerable neurological workup was done, including serum venous lactate, quantitative amino acid and acylcarnitine profiles, serum encephalopathy panel, and magnetic resonance imaging of the brain, which ruled out various metabolic diseases and causes of noninfectious encephalitis. Family history was notable for several family members with hearing impairment secondary to DIS, which was confirmed with genetic testing. Some of the patient’s family members who were affected by DIS experienced concurrent neuropsychiatric symptoms, including migraines, auditory hallucinations, and depression, since the onset of puberty (
Figure 1).
The patient developed auditory hallucinations at age 15; she had five psychiatric hospitalizations prior to this presentation and had been given diagnoses of bipolar disorder and generalized anxiety disorder. Before admission, she was taking lamotrigine 100 mg twice daily and quetiapine 150 mg twice daily. Prior medication trials included aripiprazole, lithium, buspirone, and hydroxyzine; aripiprazole 20 mg was effective in reducing her auditory hallucinations but was discontinued due to financial constraints.
On presentation, the patient described ongoing auditory hallucinations involving several distinct male and female voices that she heard in both ears and that sounded as if they were both inside and outside her head. She identified these voices as different from her internal monologue and typically described them as persecutory. These voices often commanded her to perform certain actions, such as walking in specific patterns, leaving her house, or injuring herself. She would obey these commands out of the fear that she and her family would be hurt if she did not comply. The patient expressed intermittent suicidal ideation without a plan and hopelessness regarding her intractable hallucinations. She denied persistent depressed mood, symptoms of mania or hypomania, substance use, and history of trauma. On examination, the patient was well groomed and cooperative with the interviewer and exhibited a linear thought process and full range of affect. Further workup, including thyroid stimulating hormone, folate, vitamin B12, and treponemal antibody, was unremarkable.
In the hospital, lamotrigine administration continued and quetiapine administration was stopped because of concerns for long-term weight gain. Risperidone was started and increased to 5 mg daily over the course of approximately 2 weeks, with a reduction in, but not complete resolution of, auditory hallucinations. Risperidone was not increased further because the higher dosages did not seem to provide additional therapeutic benefit. Additionally, it was thought that if the hallucinations were attributable to the patient’s genetic disease or the hearing impairment itself, rather than to aberrant dopaminergic transmission alone, then the hallucinations might not fully resolve with antipsychotics. By the end of the hospital stay, the patient was consistently denying suicidal ideation, appeared future oriented, and was less distressed by her auditory hallucinations. She was discharged without further modifications to her medications.
On follow-up with the patient 6 months after discharge, she reported two additional hospitalizations for worsening auditory hallucinations and paranoid delusions. Her delusions included the belief that a nondescript male was going to kill her, and these delusions would last for several hours to a day. Risperidone had been discontinued because of its ineffectiveness, and she was restarted on quetiapine 400 mg twice daily. She reported better effects with quetiapine but continued to have occasional breakthrough auditory hallucinations.
Discussion
The patient was diagnosed as having an unspecified psychotic disorder. This was a challenging case because the patient did not meet DSM-5 criteria for any other psychiatric disorder. Given an absence of mood symptoms, negative symptoms, thought disorganization, and prodromal symptoms typically associated with schizophrenia, mood disorders and schizophrenia spectrum disorders were effectively ruled out. Even occasional paranoid ideations were atypical in presentation, because the duration of symptoms lasted for less than 1 day and the patient immediately regained fair insight after resolution.
Although the pathogenesis of the patient’s auditory hallucinations remains unclear, there may be an association between these symptoms and a diagnosis of DIS characterized by chromosome 15 abnormalities. Notably, the neuropsychiatric symptoms reported by the patient were also reported by some of the patient’s siblings with a DIS diagnosis. It is also possible that these symptoms reflected additional gene deletions, rather than the effects of STRC and CATSPER2 deletions alone. Her genetic testing was notable for an additional deletion of the CKMT1B gene and possibly the PPIP5K1 gene, which have unknown clinical significance. More research is needed to characterize the role that this locus may have in psychiatric manifestations.
Given the reduction but not resolution of the patient’s auditory hallucinations despite multiple antipsychotic trials, these symptoms may not be attributable to abnormalities in dopaminergic transmission alone. One possible explanation for her refractory hallucinations could relate to deafferentation resulting from her congenital hearing loss secondary to DIS. However, the patient had worn hearing aids since early childhood and thus had already received the recommended treatment for deafferentation hallucinations. Neurotransmitters other than dopamine have been implicated in hallucinations, including acetylcholine, glutamate, and GABA. There are reports of auditory hallucinations, in particular, musical hallucinations, being successfully treated off label with acetylcholinesterase inhibitors, benzodiazepines, barbiturates, antidepressants, and antiepileptics, although none of these studies were placebo controlled (
5). Coebergh et al. (
5) suggested that acetylcholinesterase inhibitors may be helpful for patients with hearing loss and musical hallucinations. However, it is unclear how applicable this approach would have been to our patient because the study included patients with various other types of hearing loss but did not include patients with nonmusical, auditory verbal hallucinations. These previous findings also appear to be concordant with the muscarinic hypothesis of schizophrenia, whereby decreased cholinergic activity in the central nervous system of patients with schizophrenia is thought to contribute to perceptual disturbances. Postmortem studies of individuals with schizophrenia have shown a decrease of muscarinic receptor density, particularly M1 receptor density, in various brain regions, including the frontal cortex, basal ganglia, and hippocampus. Some studies of patients with schizophrenia have indicated that augmenting an antipsychotic with a cholinesterase inhibitor may help improve cognitive function, positive symptoms, and tardive dyskinesia (
9). Further research is warranted to investigate the utility of alternative interventions to antipsychotics in treating patients with atypical presentations of auditory hallucinations.
Key Points/Clinical Pearls
Acknowledgments
The authors thank Lisa Bosco, M.D., for clinical guidance in this case and John Querques, M.D., and Cristina Montalvo, M.D., for editing help.