Substantial numbers of psychiatric inpatients are not linked successfully to outpatient specialty mental health care after an acute hospitalization. Estimates range from 22% to 90%, depending on the sample and the definitions of linkage
(1–
7). Failure to engage patients in outpatient services greatly increases the probability of relapse and rehospitalization and reduces patients’ quality of life
(8–
10). Moreover, pressure to provide appropriate care in the less restrictive and less costly outpatient sector has been increasing at the same time that managed care companies and consumers are holding hospitals accountable for outcomes after discharge. The widespread gap in continuity of services underscores the importance of inpatient staff’s being able to identify patients at high risk for not completing referrals and the need for effective strategies for linking patients to outpatient care.
In much of the research on the determinants of failed or successful linkage between inpatient and outpatient psychiatric care, findings on patient risk factors have been inconclusive. Data on the role of clinical characteristics in predicting successful linkage are contradictory
(5,
11–
13), and uncertainty about the impact of diagnosis has been compounded by the large number of studies in which neither diagnosis nor severity of illness was measured. The propensity to begin outpatient treatment is probably not captured by diagnosis alone, but more likely by high-risk behaviors
(14,
15), the meaning of psychiatric symptoms, the distress they cause, and how much they disrupt social, family, and work activities
(16). Patients who are not successfully linked to outpatient care may be clinically different from those who are successfully linked, but these differences are not known.
Sociodemographic characteristics have by and large not been systematically associated with linkage to outpatient care
(1,
12,
17,
18). Inconsistency also exists in the relationship between linkage and previous hospitalizations
(6,
11,
12), length of stay
(12,
13,
19), and patients’ attitudes about their illness, hospitalization, and outpatient treatment
(5,
12).
By contrast, a more consistent predictor of successful transition to outpatient treatment after a hospital discharge is the presence of interventions or “bridging strategies”
(20). Such strategies have ranged from more routine contacts (e.g., telephone and letter prompting) to various inpatient programmatic interventions aimed at discharge planning and linkage
(1,
3,
12,
21) to boundary-spanning communication and involvement of the patient and treatment staff
(4,
9,
13,
22). The relative effectiveness of these various strategies has not been examined in the context of patients’ clinical and social risk factors. With noteworthy exceptions, hospital staff often engage in the more easily and quickly accomplished practices than in those that are most effective
(23). The limited base of clinical and research findings on the effectiveness of bridging strategies for different patient groups may contribute in part to the uneven use of these strategies in routine clinical practice.
The study reported here examined the impact of several clinical bridging strategies on successful linkage with outpatient psychiatric care in a sample of inpatients discharged to the community. Patient risk factors for unsuccessful linkage were assessed along with the linkage strategies intended to mitigate these risks.
Method
Procedures
The medical records of a sample of consecutive psychiatric patients discharged over a 4-month period were identified and reviewed by using a clinically detailed, structured form developed and pretested for this study. The medical record abstraction form included six general categories of patient data: 1) sociodemographic characteristics; 2) clinical history; 3) diagnosis, comorbidities, and assessment of dangerousness; 4) length and content of hospital stay (e.g., medication regimens, participation in education groups); 5) inpatient treatment practices preparatory to discharge, referral, and linkage to outpatient services; and 6) outpatient referral sites. Estimates of interrater reliability (intraclass correlation coefficient=0.81–1.0) for record abstraction data were well above acceptable criteria. The abstraction of medical record data was done blind to patient follow-up status. Clinicians and staff at outpatient programs were contacted to determine if patients attended scheduled or rescheduled initial appointments within 4 weeks of discharge. Project staff made telephone calls and site visits to acquire attendance information. All outpatient providers were given copies of patients’ consent forms to encourage cooperation and ensure confidentiality.
Study Participants
Patients with a primary psychiatric diagnosis discharged from the psychiatric units of two large urban, acute-care, general hospitals had to satisfy the following criteria for inclusion in the study: 1) 18 years of age or older, 2) length of stay of 72 hours or more, 3) no principal diagnosis of mental retardation, and 4) a discharge to the community for which inpatient staff had the opportunity to plan outpatient care. Patients transferred to nursing homes, state institutions, corrections facilities, other short-term general hospitals, and inpatient rehabilitation centers were excluded from the study group. A total of 340 patients met the inclusion criteria. Within this group were 45 patients who were not referred to outpatient mental health programs, and 66 referred patients whose attendance or no-show status could not be confirmed despite persistent efforts by the research team in contacting providers. Thus the final study group consisted of 229 patients (78%) for whom inpatient staff had arranged referrals to outpatient programs.
Analyses showed some distinctive characteristics of the two excluded subgroups. The majority of the 45 patients who were not referred by staff left the hospital against medical advice or earlier than expected (62.2%). Another 20.0% preferred to arrange their own outpatient care, 8.9% went to residences with onsite care, and 8.9% refused referrals. Although the nonreferred patients did not differ from the referred patients on several clinical characteristics (e.g., substance abuse problems, first admission, dissatisfaction with prescribed antipsychotics, unstable housing placements at discharge, or involuntary admission, an indicator of possible treatment resistance), they were more likely to be members of a minority group (68.2% versus 45.9%) (χ2=7.55, df=1, p=0.006), to not have a case manager (95.6% versus 80.7%) (χ2=6.03, df=1, p=0.01), to have less family involvement during the inpatient stay (mean score on a scale of family involvement=0.91 versus 1.46) (t=2.85, df=338, p=0.005), and to have a shorter length of stay (mean=14.44 days versus=24.72 days) (t=3.44, df=70, p=0.001).
The majority of the 66 patients who were given a referral but whose attendance or no-show status could not be confirmed were referred either to a private clinician (69.7%) or to a substance abuse program (19.7%), referral sources that were reluctant to provide information on these patients. Compared with patients whose outpatient attendance could be confirmed, those whose attendance could not be confirmed were more likely to be white (64.6% versus 50.9%) (χ2=3.77, df=1, p=0.05), married (24.6% versus 8.1%) (χ2=13.23, df=1, p=0.001), and employed (33.3% versus 21.0%) (χ2=4.33, df=1, p=0.04). Although many of the patients referred to private clinicians were returning to providers who had treated them previously, information about patients’ previous treatment providers was not consistently available. By contrast, the patients in the final study group—those who had referrals and were successfully followed—had more clinically complex cases, including more dangerous behaviors (mean score on a scale of dangerous behaviors=0.98 versus 0.64) (t=2.06, df=293, p=0.05), and more resistance to treatment (mean score on scale of treatment resistance=0.35 versus 0.20) (t=2.00, df=126, p=0.05) than those whose outpatient status remained unknown. Among the final study group of 229 patients, almost one-half (48.0%) had a primary diagnosis of schizophrenia, 13.9% had other psychotic illnesses, 24.0% had a depressive disorder, and the remaining 13.9% had other primary psychiatric diagnoses.
Measures
Measures of substance abuse, dangerousness to self, abusive/violent behaviors, and treatment resistance were compiled to assess patients’ clinical and behavioral risk status. Patients were considered to have a substance abuse problem if the history or records of a toxicology screen or blood alcohol level indicated current use of illegal substances, including sedatives, cocaine, cannabis, stimulants, opioids, hallucinogens, inhalants, or alcohol. Dangerousness to self was considered present if there was evidence of an attempted or threatened suicide before admission or during the hospitalization. Abusive/violent behavior was considered present if the chart noted threats, physical abuse of others, or the use of seclusion or physical restraints. Patients who expressed reluctance or refusal to engage in outpatient care were considered to be resistant to treatment. Whether the patient’s hospital stay was involuntary or voluntary was also recorded.
Several practices related to discharge planning and referral were measured. Patient contact with outpatient services before discharge involved three items whose presence or absence was noted: whether the patient met with outpatient clinicians, visited an outpatient program, or began an outpatient program. Involvement of the patient’s family or support network, including friends and significant others, during hospitalization was indicated by entries in the record noting family meetings and support services held during hospitalization (e.g., counseling and educational or discharge planning sessions provided by the inpatient staff for family members or significant others and at times including the patient), inpatient staff’s discussion of the discharge plan with the family, and family visits with the patient during the inpatient stay. A single item measured whether staff discussed the discharge plan with outpatient clinicians. Inpatient staff’s involvement after discharge was measured with four items: whether the patient was accompanied to the first outpatient visit, whether outpatient transportation was arranged, whether reminders about the first outpatient visit were given, and whether staff confirmed the patient’s attendance at the initial visit. Because of the positive association between the use of long-acting intramuscular neuroleptics and treatment compliance
(24), patients who were prescribed depot neuroleptics at discharge were identified. Patients who had case managers were also identified.
Data Analysis
Chi-square tests for categorical variables and t tests for continuous variables were used to identify patient risk factors associated with failure to keep initial outpatient appointments and to identify treatment practices and interventions associated with patients’ keeping appointments. All statistical tests used two-tailed significance levels.
Multivariate logistic regression models were used to examine the impact of patients’ risk characteristics and inpatient treatment practices on linkage with outpatient services after discharge. In the logistic regression models, the variables for patient contact with outpatient clinicians and family or support network involvement were coded to reflect the intensity of involvement (e.g., a patient’s beginning an outpatient program before discharge meant that the patient visited the program and met with clinicians; “family meetings” meant that inpatient staff discussed the discharge plan with the family and that the family visited the patient in the hospital).
Results
Identifying High-Risk Patients
Almost two-thirds of the discharged patients (65.1%, N=149) failed to keep a referral appointment or a rescheduled appointment.
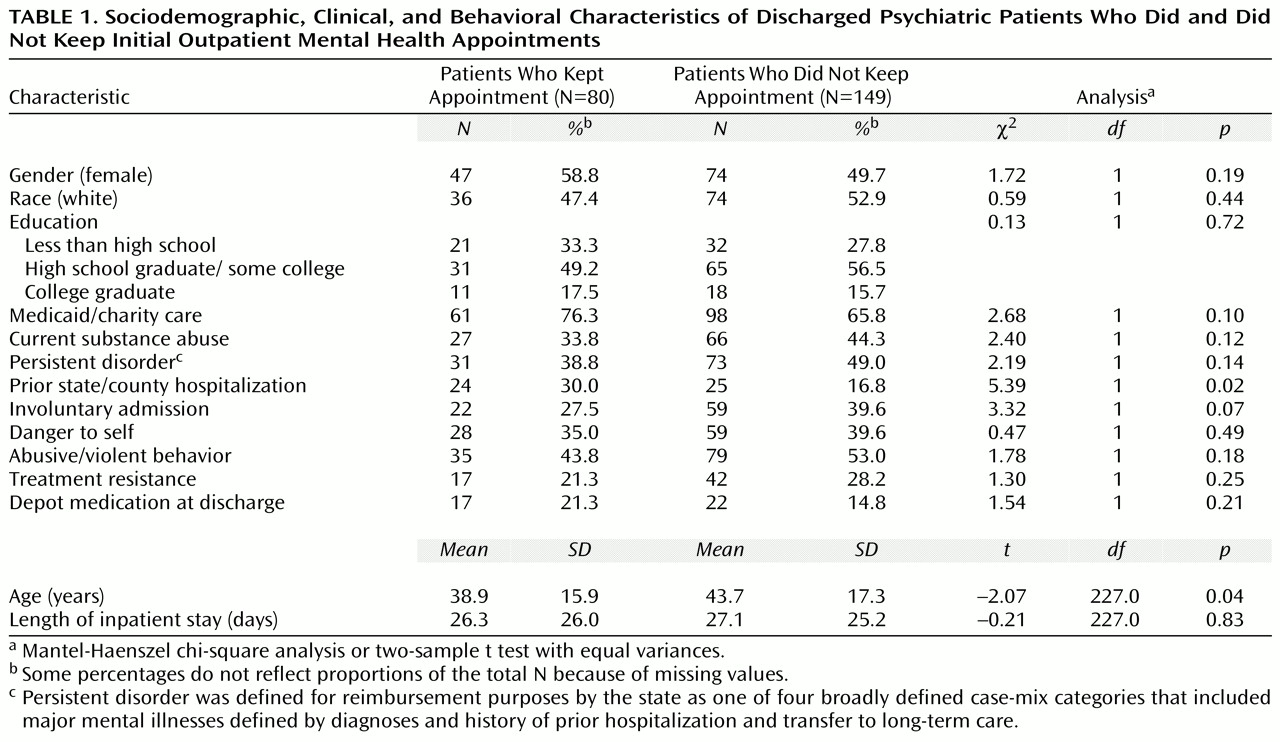
Table 1 shows that the sociodemographic and clinical/behavioral characteristics of patients who kept outpatient appointments were similar to those of patients who did not keep the appointments. Patients who kept the appointments differed significantly from those who did not only in being younger and having a prior public psychiatric hospitalization. Other potential clinical and behavioral risk factors, including dangerousness to self, treatment resistance, and a history of abusive and violent behavior, were not significantly related to keeping an appointment. Approximately 70% of the study group were participating in the Medicaid program.
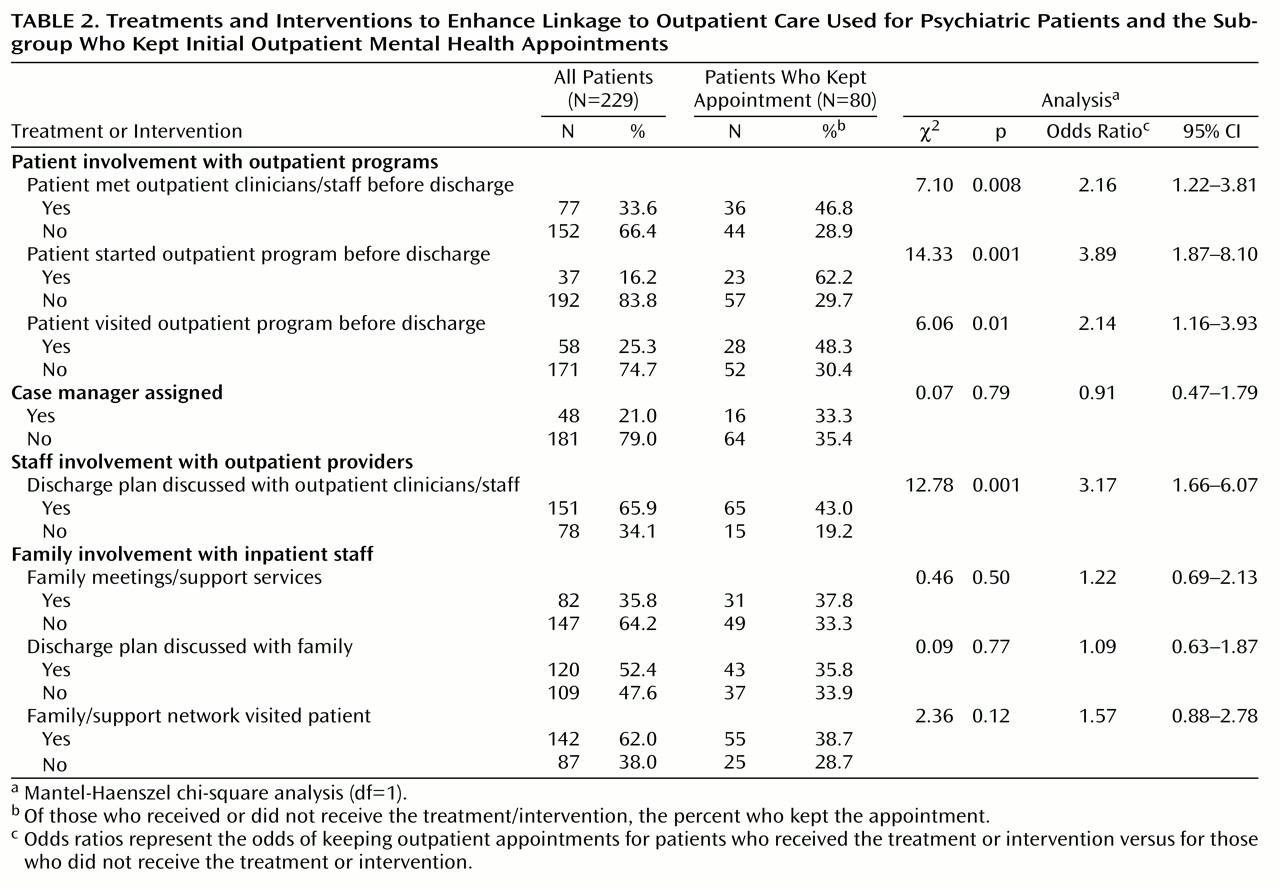
Treatments and Interventions Aimed at Enhancing Linkage
Table 2 shows data on the use of inpatient treatments and interventions aimed at enhancing linkage in the entire study group and among the patients who kept their referral appointments. The most common linkage strategy that was significantly associated with patients’ keeping their initial appointments was a discussion about the discharge plan between inpatient staff and outpatient clinicians. This intervention was used for about two-thirds of the entire study group. Among patients whose discharge plans were discussed by inpatient staff and outpatient clinicians, 43.0% kept their initial outpatient appointment, compared with 19.2% of patients whose plans were not discussed. Patient involvement with outpatient programs while still in the hospital was less common, but had a significant impact on patients’ keeping scheduled appointments for outpatient services. About one-half of the patients who met with outpatient clinicians and staff before discharge (46.8%) kept their appointments, compared to only about one-fourth (28.9%) of the patients who did not meet with outpatient clinicians before discharge. Among the patients who visited an outpatient program before discharge, almost one-half (48.3%) kept their appointments, and for those starting an outpatient program before discharge, almost two-thirds (62.2%) kept their appointments. This predischarge contact underscores the generalizability of Olfson and colleague’s 1998 finding that inpatients who had contact with outpatient clinicians who had not previously treated them were significantly more likely to attend their scheduled appointment after discharge
(22).
Family visits and families’ participation in discharge planning or meetings with the staff were not associated with patients’ keeping an appointment. The most infrequent linkage strategies, used for 5% or less of patients, involved staff efforts that focused on the postdischarge period (e.g., arranging transportation, issuing reminders about appointments) (data not shown).
Effectiveness of Treatments and Interventions
As shown in
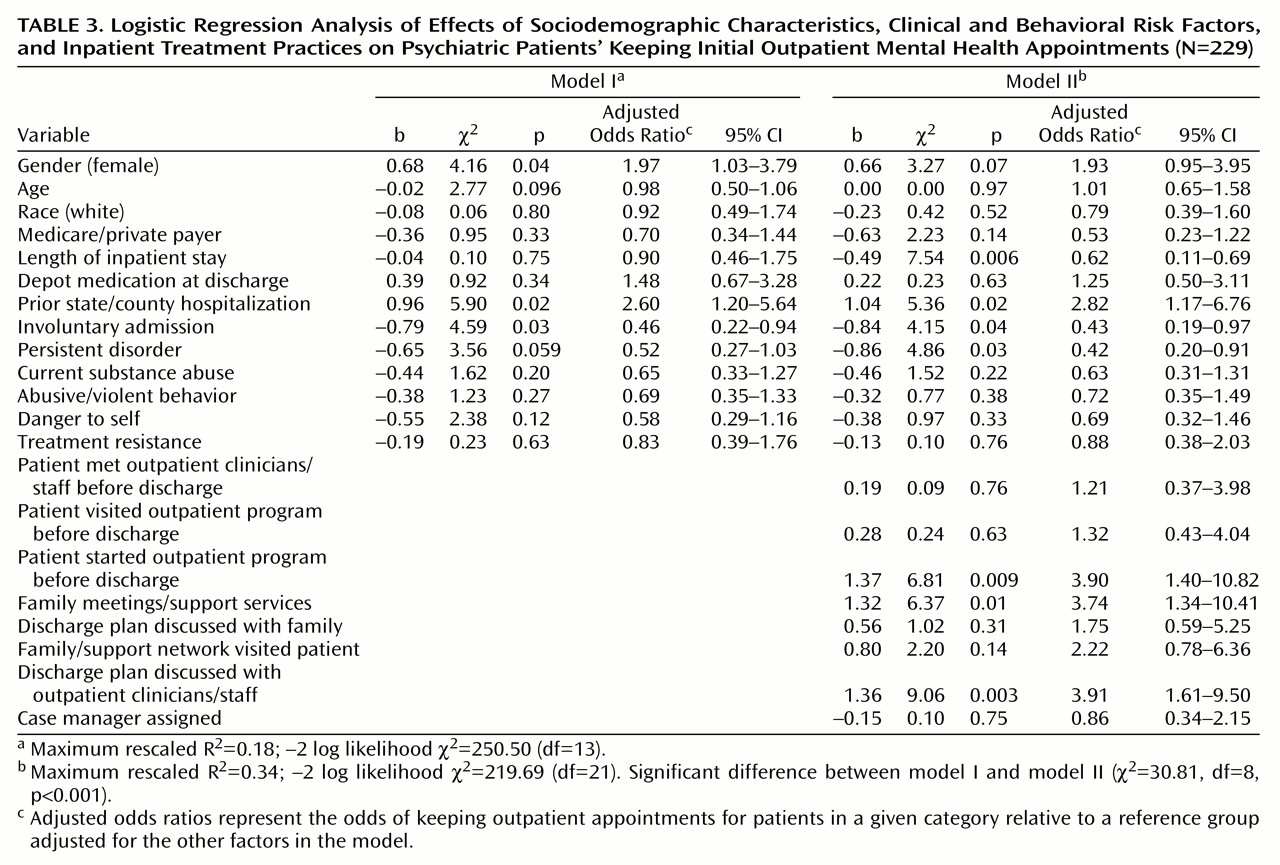
Table 3, multivariate logistic regression model I included sociodemographic and clinical/behavioral risk variables, and model II examined the impact of inpatient practices on linkage, controlling for patient risk factors. Among the sociodemographic factors, female gender increased the probability of linkage to outpatient appointments. Patients admitted voluntarily and those with a prior admission to a public mental health institution also had an increased probability of attending their outpatient appointments.
As shown in model II, three inpatient treatment strategies significantly increased the probability of patients’ attending their first outpatient appointments: patients’ starting an outpatient program before discharge, family meetings and support services for families and significant others, and communication about the discharge plan between inpatient staff and outpatient clinicians. These strategies more than tripled the probability of patients attending their initial appointments (odds ratios=3.74–3.91). Although family involvement was an insignificant factor in the bivariate analyses, with the inclusion of patients’ risk characteristics, family meetings significantly increased the probability of patients’ linkage to outpatient care. The inclusion of these intervention variables in the regression analysis also significantly improved the fit of the second model.
Length of stay also became significant in the final model. Patients with shorter lengths of stay had an increased probability of keeping referral appointments. The odds of keeping an appointment for those with a length of stay of 28 days was 1 in 5 compared to about 1 in 3 for patients discharged at 2 weeks. Linkage strategies were more effective for patients who were discharged earlier, which may signal that inpatient staff give higher priority to these practices when earlier discharge is anticipated. It is also possible that a longer length of stay reflects difficulty in placing patients in outpatient programs. Persistent mental disorder was an additional risk factor in the final model; patients with a persistent disorder had a decreased probability of keeping referral appointments even in the presence of linkage strategies.
Discussion
The failure of patients to engage in specialty mental health care shortly after hospitalization undermines important clinical gains made during inpatient treatment and thwarts the intended trajectory toward further stabilization, maintenance, and community adjustment. Evidence that patients are connected to ongoing care shortly after a hospital stay is also indicative of a clinically integrated system of care. Yet, in this study, only about one-third of the patients attended the outpatient program to which they were referred, a serious problem for usual psychiatric practice. With the investment of considerable resources in inpatient care, much effort needs to be directed to preparing patients adequately for discharge and optimizing their linkage to appropriate community services.
This study improves on existing research by examining competing interventions in a group of patients with diverse and complex needs. Inpatient staff have an opportunity to identify patients who represent a high risk for not complying with referrals, notably patients with persistent mental disorders, those who are admitted involuntarily, those who are likely to have a longer length of stay, and those without a history of long-term care or longer experience in the mental health system.
The most meaningful and successful linkage strategies involved an interpersonal dimension that reduced the inpatient-outpatient dichotomy
(25). These strategies included inpatients’ beginning outpatient programs before discharge, communication about discharge plans between inpatient and outpatient staff, and sessions that made the family a part of the treatment team. Prior work has also shown that inpatient psychiatric units that reported more family interventions during a hospital stay were also oriented to using more linkage strategies
(26).
Although these inpatient strategies appear to connect patients successfully to outpatient programs, many are not routinely used. For more than one-third of the patients, discharge plans were not discussed with outpatient providers. For two-thirds or more, extensive predischarge contacts between patients and outpatient providers did not occur.
As the patient population served through Medicaid managed care has grown to 54% of the total Medicaid population nationally, and 70% or more in 17 states
(27), hospitals may especially want to negotiate provisions for outpatient service contact before discharge for Medicaid patients with clinically complex cases. Managed care organizations also have a financial interest in services that decrease the probability of costly readmissions. Likewise, the practice of beginning an outpatient program before discharge might be incorporated into the procedures of hospitals and managed care organizations as a quality improvement measure.
As Olfson and colleagues have reported
(22), it is conceivable that patients who met with outpatient clinicians during an inpatient stay or visited or began an outpatient program before discharge may have been highly motivated to participate in treatment and adhere to the discharge plan. Although we measured treatment resistance and found that it was not associated with linkage, it is likely that this measure did not completely capture motivation. Without an experimental design, we could not fully examine the differences in patients’ motivation or other unmeasured patient characteristics and treatments that may have contributed to improved probability of completing referrals. Because patients admitted involuntarily were less likely to keep outpatient referral appointments, motivation should be assessed and regarded as a critically important risk factor.
Issues of self-selection and attrition limited our study group. Not included in the study group were patients who left against medical advice, those discharged without outpatient appointments, and those with self-referrals. Given their shorter length of stay and resistance to further inpatient treatment, these patients may be especially vulnerable to relapse. The effectiveness of inpatient staff’s contacting these patients after discharge to help to arrange self-referrals is worthy of future study. In addition, we cannot assess the effects of the bridging strategies on the 66 patients lost to follow-up who were less impaired and higher functioning and who were likely to have been referred to private clinicians. Likewise, the study group was limited to patients from the inpatient units of two large urban hospitals, and the findings may not be generalizable to all persons with a severe mental illness.
The measures of patients’ and staff’s contacts with outpatient clinicians and programs do not detail the nature and content of the interactions. Some contacts might have been informal, and others may have been directed more specifically to treatment issues. Nonetheless, this contact is critical as a necessary first step in developing a strong therapeutic alliance
(28). The reviews of medical records also would have missed strategies that were not recorded. Only initial outpatient visits after discharge were confirmed. Data were not available on successive visits or later dropouts from treatment.
Continued pressures in a managed care environment to reduce the length of an inpatient stay, staffing reductions, and decreased revenues may force actions that can increase, not reduce, discontinuities in care if high priority is not given to effective discharge planning and bridging strategies that avert relapse and rehospitalization. More inpatient clinical work that focuses on the interface with families and outpatient clinicians will need to be accomplished in less time. Involving family members, significant others, and outpatient clinicians in ways that engage patients successfully in ongoing care should be a critical component of the inpatient stay.