Reduction of inpatient length of stay has been a major goal in health care administration in general and in the Veterans Health Administration (VHA) health care system in particular. Prior studies by researchers
(1,
2) and the General Accounting Office
(3) have found that hospital stays within the VHA are significantly longer than at community hospitals and that improved efficiency is possible without lowering quality of care. Efforts instituted by the VHA to encourage reduction in hospital length of stay have included a capitated reimbursement structure and publishing of an annual hospital “score card” that identifies hospitals with unusually long average lengths of stay. Overall length of stay as well as psychiatric length of stay fell in these hospitals during the 1990s, from a mean of 30.6 days in 1994 to 18.8 days in 1998
(4–
7). Further reductions while maintaining the quality of care continue to be a goal. To meet this goal, it is important that the sources of variance in length of stay be well understood
(2).
Prior efforts to identify factors associated with length of stay have had limited success
(8). Multivariate approaches have focused on three general categories of factors: patient factors, treatment factors, and system factors such as reimbursement strategies
(9). These variables have been found to account for only 10%–27% of the total variance in psychiatric length of stay, with R values ranging from 0.31 to 0.52, leaving some researchers pessimistic about the possibility of predicting length of stay from empirical data. Choca and colleagues concluded in 1988
(8) that the predictive efficacy of these models was discouraging and that other major sources of variance in length of stay were unlikely to be identified.
An ecological approach to understanding the sources of variance in length of stay highlights variables in the larger context or environment of hospitalization as among the most likely to be overlooked. The environment in which hospitals operate has an impact on clinical practice and needs to be included in working models of length of stay. Clinicians are often reluctant to discharge psychiatric patients, particularly those who are homeless, during inclement weather; patients are also reluctant to leave warm hospitals. The study reported here focused on one aspect of the physical environment—climate—to determine if it is related to psychiatric length of stay.
To study contextual variables such as climate, it is important to have multiple sites to provide the needed range in the target variables. Many prior studies have looked exclusively at single hospitals or small groups of hospitals
(10,
11). The VHA health care system has a national network of more than 150 hospitals in all 50 states. Relative homogeneity between VHA hospitals in terms of basic mission, policy, and funding procedures allows for easier examination of contextual variables such as climate. At the same time, the mission and population served by the VHA are somewhat different from those of the average psychiatric hospital; VHA hospitals are likely to serve a greater percentage of male patients, patients with dual diagnoses, patients with limited financial resources, disabled adults, and homeless adults. For the study reported here, we hypothesized that climate is significantly related to length of stay and that warmer, drier climates are associated with shorter lengths of stay.
Method
The two variables selected for the study were climate and psychiatric length of stay. Climate is a multifaceted variable and includes factors such as air temperature and precipitation. Eight common climate statistics collected by the National Weather Service at a large number of locations across the country were used for this study. They were mean air temperature during January, mean air temperature during July, number of days per year with temperatures below 32˚F, number of days per year with temperatures below 0˚F, number of days per year with temperatures above 90˚F, annual precipitation, annual snowfall, and number of days with 1 inch or more of snow cover.
Climate statistics represent data collected at national weather stations for the period of 1955–1990. Data for VHA sites were selected from a national listing of climate data collected by the National Weather Service for more than 1,000 sites in the U.S.
(12). Complete climate data were available from the specific town or city in which the hospital was located for 112 of the 152 VHA hospitals. Twenty-two of the remaining 40 hospitals had climate data available from a location within 20 miles of the hospital, and so were included in the analysis. The 18 hospitals for which no climate data were available for a site within 20 miles were excluded. To ensure that excluding those hospitals would not significantly impact the results of this study, mean psychiatric length of stay was compared for hospitals with and without climate data. No significant difference was found.
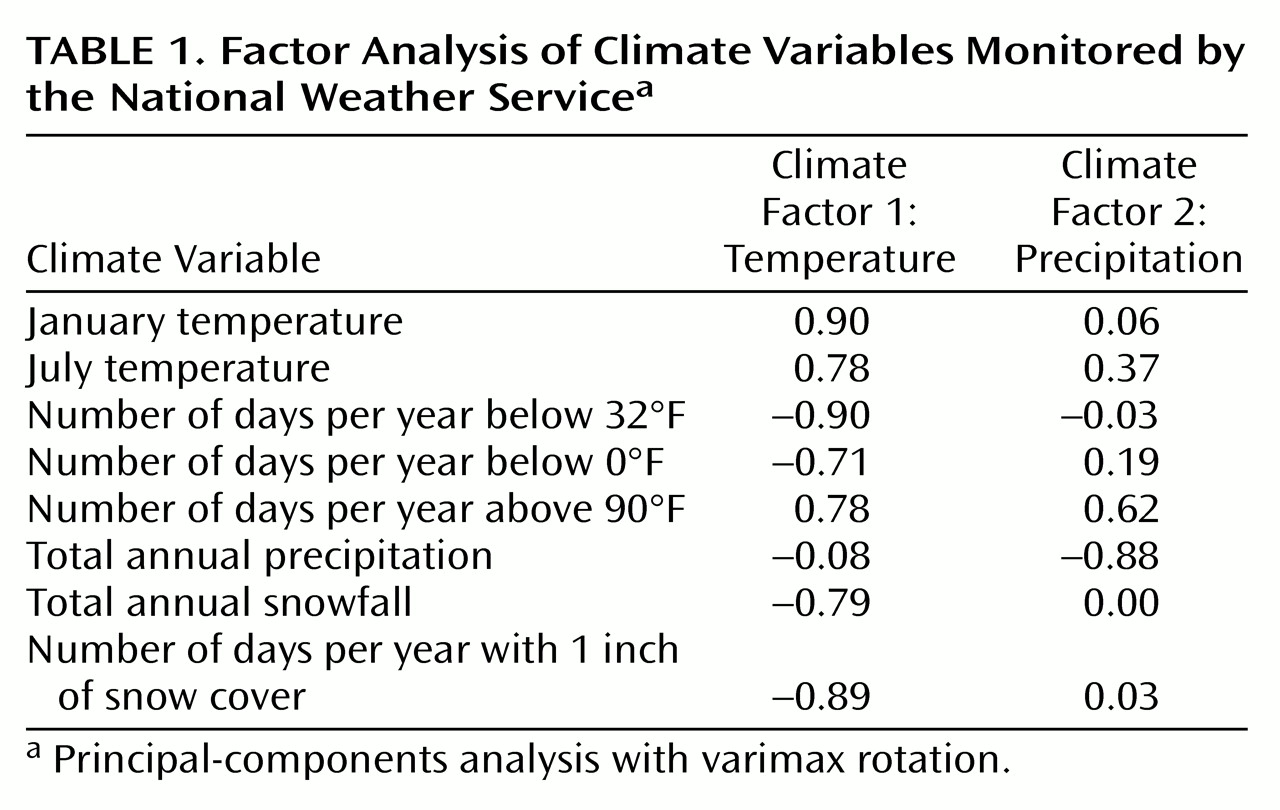
Climate variables correlate highly, so factor analysis was performed to reduce their number. A principal-components analysis with varimax rotation resulted in two factors (
Table 1). Factor 1 loadings represented an overall temperature factor. Factor 2 loaded most heavily on annual precipitation and days per year with a temperature over 90˚ F, and so appeared to represent precipitation in a climate continuum from hot and dry to cool and moist. The Pearson product-moment correlation between the two climate factors was small (r=0.07). Psychiatric length of stay was defined as the number of days of hospitalization per admission to an acute psychiatric ward. Inpatient substance abuse and psychiatric rehabilitation services were not included in this analysis, as these services tend to have specified program lengths. Service utilization data, including length of stay for psychiatric hospitalization in VHA hospitals, are published annually by the VA Northeast Program Evaluation Center. Data for 1994–1998 were used in the study
(4–
7). Of the 134 hospitals for which climate variables were available, 18 had no acute psychiatric program during at least one or more of the years from 1994–1998. Data on psychiatric length of stay were not available for 17 additional hospitals, resulting in a pool of 99 hospitals with complete climate and length-of-stay data.
VHA hospitals are organized into 22 regional groups or Veterans Integrated Service Networks, each of which includes four to 10 hospitals. The hospitals included in this study were distributed evenly throughout the 22 Veterans Integrated Service Networks, with the exception of Veterans Integrated network 19, representing the Northern Rocky Mountain states, for which complete data were available for only three of seven hospitals. Hospitals in Alaska and Hawaii were among those excluded for the reasons noted above. Length of stay was calculated at the service network level by weighting the contribution of each hospital by the number of psychiatric admissions in the target year. Climate data were calculated for each service network in the same way.
Two climate factor scores were calculated for each of the 99 VHA hospitals included in the study and for each of the 22 service networks. Correlations were calculated between climate factors and psychiatric length of stay at the hospital level and at the service network level for the years for which these data were available, 1994–1998.
Results
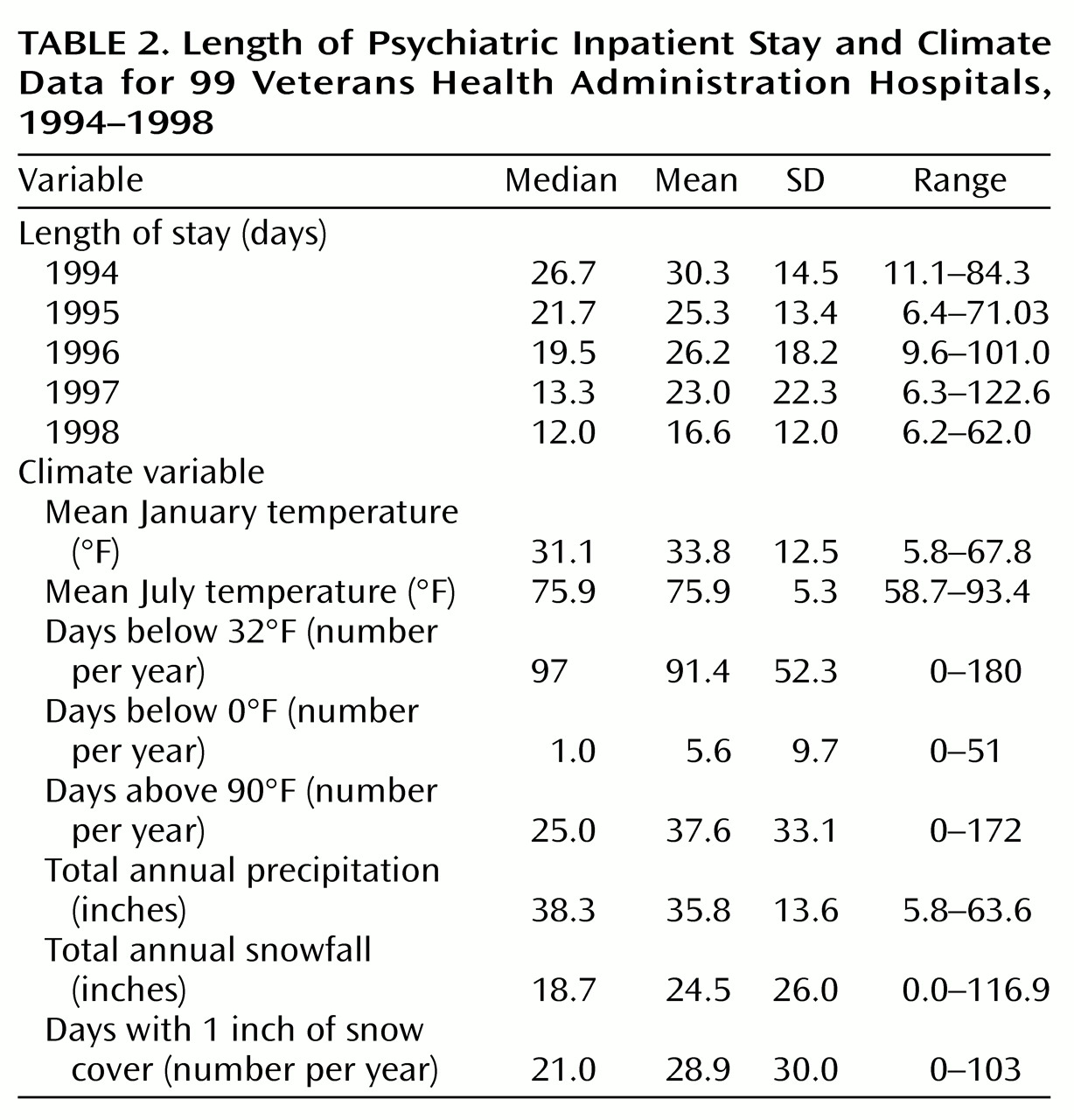
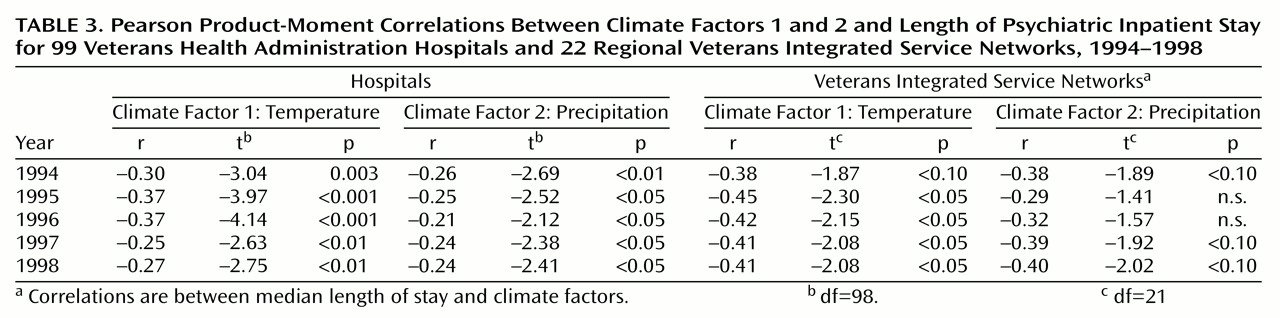
Table 2 summarizes length-of-stay data for 1994–1998 as well as the climate data used to create the climate factors. As expected, the mean length of stay at the hospital level decreased 45% from 30.3 days (SD=14.5) in 1994 to a mean of 16.6 (SD=12.0) in 1998. Pearson product-moment correlations between length of stay for each year and climate factor 1 ranged from –0.25 to –0.37, with the percentage of variance accounted for ranging from 6% to 14%, with colder climate associated with longer lengths of stay.
Table 3 summarizes the correlations between length of stay and climate factors at both the hospital level and the level of the Veterans Integrated Service Networks. Correlations between length of stay and factor 2 at the hospital level are slightly smaller in magnitude, ranging from –0.21 to –0.26, with the percentage of variance accounted for ranging from 4% to 7%. These correlations were also all statistically significant, with wetter climates associated with longer length of stay. At the service network level, correlations with mean length of stay and climate factor 1 ranged from –0.47 to –0.75, with the percentage of variance accounted for ranging from 22% to 56%. As the distributions of length of stay at the service network level were skewed, median length of stay and climate factors were correlated at this level (
Table 3). Correlations using the median were somewhat smaller, ranging from –0.38 to –0.45 and accounting for 14% to 20% of the variance. January temperature had a correlation of –0.68 with length of stay at the service network level, accounting for 46% of the variance. Correlations between median or mean length of stay and factor 2 were smaller in magnitude and were not statistically significant.
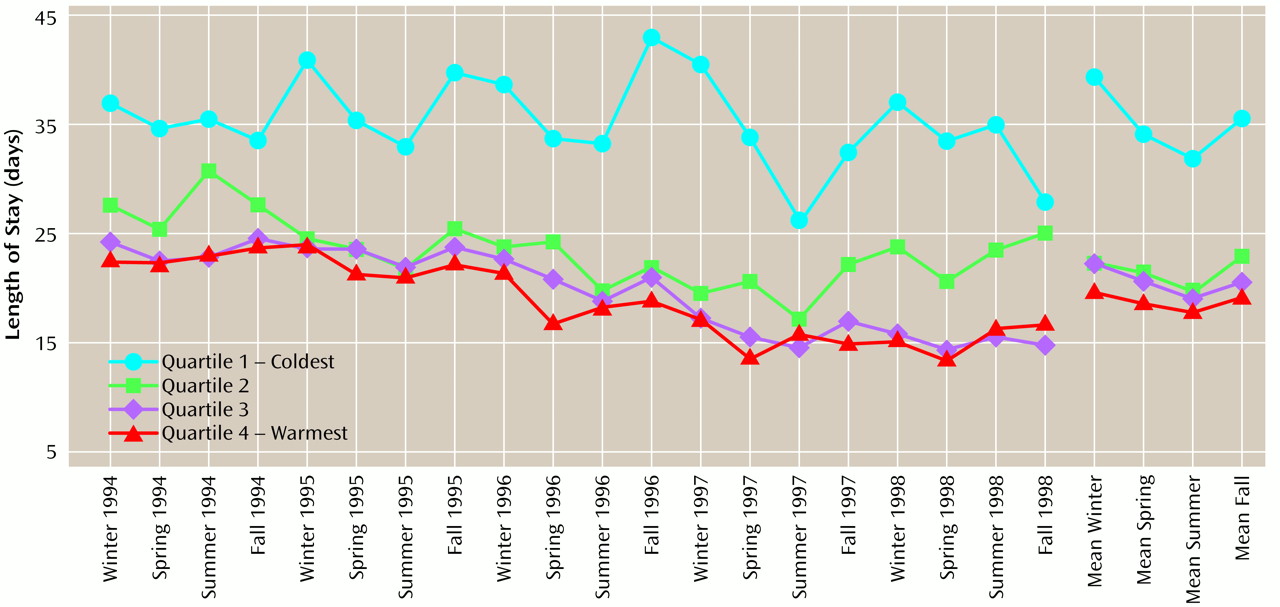
Figure 1 represents the fluctuations in length of stay by season across the 5-year span at the hospital level, with hospitals divided into quartiles by climate factor 1. The coldest quartile was substantially higher in overall length of stay than the remaining hospitals. Within the coldest quartile of hospitals, a seasonal variation in length of stay, most evident in 1995–1997, was found. Aggregated across years, the pattern indicates that for each of the four quartiles, the longest length of stay occurred in the winter and fall, although analysis of variance (ANOVA) failed to find a significant effect for season across all hospitals (F=0.36, df=3, 380, p>0.50) or for the coldest quartile of hospitals alone (F=0.16, df=3, 93, p>0.50). Given the skewed distribution of length of stay, a log transformation was performed and the ANOVA was repeated on the transformed variable. Again, a significant effect for season was not found either across all hospitals (F=0.87, df=3, 380, p>0.40) or for the coldest quartile hospitals alone (F=0.14, df=3, 93, p>0.50).
To examine the potential moderating role of homelessness, the percentage of psychiatric admissions who were homeless at the time of admission was correlated with both the climate factors and length of stay for 1996, the year of the largest correlation between climate factors and length of stay. The percentage of admissions from homelessness was positively but not significantly correlated with length of stay (r=0.04, t=0.34, df=94, p>0.50) and with climate factor 2 (r=0.05, t=0.35, df=94, p>0.50) and was positively and significantly correlated with climate factor 1 (r=0.21, t=2.04, df=94, p<0.05), suggesting that the percentage of admissions from homelessness were higher in hospitals in warmer areas.
Discussion
The results indicate that a modest but statistically significant relationship between psychiatric length of stay and climate does exist, with temperature being the climate factor most strongly related to length of stay. This finding supports our hypothesis that environmental variables such as climate influence hospital utilization. To our knowledge, climate has not been examined with respect to psychiatric length of stay, nor have clinicians or researchers linked climate to length of stay theoretically
(13). Surprisingly, although the magnitude of the relationship between climate and length of stay is quite modest, it is similar to that of many other clinical variables previously studied
(9). For example, these data suggest that climate factor 1 alone accounts for up to 14% of the variance in length of stay, and a recent study found that diagnoses together with history of previous admissions account for less than 17% of the variance
(9). These findings suggest that there may be other contextual variables besides climate that contribute to variance in length of stay and underscore the importance of examining the impact of other such variables on service utilization.
An alternative interpretation of the current findings is that a nonclimate factor such as regional variations in patient, treatment, or hospital variables may correlate with climate and may be more salient in determining length of stay. If climate has a direct impact on length of stay, it would be reasonable to expect seasonal variations in length of stay that correspond to the natural variations in climate variables.
Figure 1 provides limited evidence of seasonal variations for the hospitals in the coldest areas of the country.
One explanation for the relationship between climate and length of stay is that colder and wetter climates may be associated with a threat or perceived threat to patient health or well being. This association may be a perception of the patient, the treating staff, or both, and it may be particularly strong for homeless patients. However, this explanation is not supported by the findings that the percentage of homeless veterans admitted to psychiatric units was actually higher in hospitals located in warmer climates and was not significantly correlated with length of stay.
It has not been established whether the correlation between climate and length of stay is common across all hospitals or is limited to VHA hospitals. In the past, VHA hospitals have been criticized for relatively long lengths of psychiatric stay
(2). For some hospitals, the relationship between length of stay and climate is likely to have contributed to the lengths of stay that have been criticized. However, the current data are not sufficient to document that this climate factor accounts for longer lengths of stay for the VHA as a whole.
The relationship between climate and length of stay over this 5-year period, during which there was a significant shortening of length of stay overall, suggests that despite the VHA’s effort to manage inpatient treatment, the relationship with climate has not significantly changed in magnitude. Some reduction in the correlation between length of stay and climate factor 1 occurred in 1997 and 1998, but the correlation with climate factor 2 at the service network level increased slightly during those years. It is possible that climate is not related to patient or treatment concerns and therefore is a source of variance that could be eliminated without impacting quality of care. It is also possible, however, that the influence of climate represents a real patient need and so reflects clinical judgment. In that case, hospitals in colder and wetter climates will by necessity have longer lengths of stay and are at a disadvantage in a capitated reimbursement system that does not correct for climate. Climate and associated costs differentials are not included currently in VHA reimbursement models. They are also not included in performance monitoring systems that focus on hospital utilization.
Limitations of this study include the lack of data on patient outcomes and the number of hospitals eliminated due to missing data. Lack of outcome data is an important shortcoming in this study, as it has been in many other studies examining length of stay. Without data about the relationship of climate to treatment outcome, it is unclear whether the impact of climate needs to be eliminated through managed care or whether it is related to appropriate clinical needs. The number of hospitals eliminated due to unavailable data on climate or length of stay represented 25% of the VHA hospitals providing inpatient psychiatric services across the 5 years studied. Although this proportion is considerable, post hoc statistical comparisons suggested that the eliminated hospitals were not significantly different from the included hospitals with respect to climate and available data on length of stay. (Results of post hoc analyses available from the first author.)
Additional research is needed to identify the ways in which climate influences length of stay by specifically looking at practitioner variables and patient needs as a function of climate. Treatment outcomes also need to be examined as a function of climate. Finally, the study results suggest that future studies should continue to look at the impact of other contextual variables on health care and specifically on hospital length of stay.