A wide range of psychiatric disorders frequently co-occur with bipolar disorder
(1–
5). Persons with bipolar disorder who have co-occurring psychiatric disorders tend to experience greater impairment and poorer outcomes than those without psychiatric comorbidity
(3,
6). However, few longitudinal studies have investigated whether individuals with bipolar disorder are at risk for future psychiatric disorders or whether individuals with other psychiatric disorders are at risk for bipolar disorder. A few prospective studies have investigated the course of bipolar disorder and co-occurring disorders in clinical samples
(4,
7), but strong inferences regarding the nature of these associations have not yet been possible. Further longitudinal research may facilitate early identification and intervention for individuals who are at risk for onset of bipolar disorder and co-occurring disorders.
Early manifestations of bipolar disorder are of particular interest because manic symptoms bear more resemblance to the externalizing symptoms associated with childhood disruptive disorders than to the internalizing symptoms associated with anxiety and depressive disorders
(5). However, epidemiological research with retrospective data has suggested that anxiety disorders may uniquely predict onset of bipolar disorder
(1), and we have recently reported longitudinal findings indicating that anxiety disorders during adolescence may increase risk for unipolar depression during early adulthood
(8). Yet, we are aware of no previous community-based longitudinal study that has investigated whether adolescents with bipolar disorder are at risk for other psychiatric disorders during early adulthood, or whether adolescents with specific psychiatric disorders are at risk for bipolar disorder during early adulthood. We report cross-sectional and prospective associations between bipolar disorder and anxiety, depressive, disruptive, personality, and substance use disorders during adolescence and early adulthood.
Method
Participants were a random sample of 717 youths (N=366 female, 51.0%) and their mothers from upstate New York who were interviewed in their homes in 1975, when the youths were a mean age of 5 years old (SD=3), and reinterviewed in 1983 (mean age of youths=14 years, SD=3), 1986 (mean=16 years old, SD=3), and 1992 (mean=22 years old, SD=3)
(9). At each assessment, written informed consent was obtained from participants after study procedures were fully explained. Families were demographically representative of the sampled population
(9). Severe anxiety, disruptive, mood, and substance use disorders were assessed in 1983, 1986, and 1992 by parent and youth interviews with the Diagnostic Interview Schedule for Children
(10). Youths and their mothers were interviewed separately by extensively trained and supervised lay interviewers. Within each youth-mother pair, the interviewer of the youth and the interviewer of the mother were blind to the responses of the other informant. Previous research has indicated that the reliability and validity of the Diagnostic Interview Schedule for Children as employed in the present study are comparable to those of other structured diagnostic interviews
(11).
Manic symptoms were considered present only if there was a distinct period of abnormally and persistently elevated, expansive, or irritable mood lasting at least 1 week, and if family or friends recognized that there was something wrong with the youth when manic characteristics were present. Subthreshold bipolar disorder was diagnosed when bipolar disorder diagnostic criteria were met, except that the number of manic symptoms was one symptom below the threshold required for bipolar disorder. Bipolar disorder was considered present during adolescence if the disorder was diagnosed in either 1983 or 1986.
Fourteen adolescents had full bipolar disorder (mean age=15 years, range=10–20), and 10 had subthreshold bipolar disorder (mean age=15 years, range=10–20). Ten adults had full bipolar disorder, and 14 had subthreshold bipolar disorder. Twenty-two adolescents and 22 adults with full or subthreshold bipolar disorder had elevated or expansive mood; 16 adolescents and 11 adults had irritable mood. Three individuals met criteria for full or subthreshold bipolar disorder during both adolescence and early adulthood. The presence of manic symptoms in adolescence was significantly correlated with the presence of manic symptoms in early adulthood (r=0.27, df=716, p<0.001). Data on cycling between manic and depressed mood were not collected. Personality disorders were assessed with items selected for that purpose and adapted for adolescents
(12). Additional information about the study methods is available from previous reports
(9,
13).
Results
Adolescents with full bipolar disorder (N=14) were more likely than those without full bipolar disorder (N=703) to have an anxiety disorder (57.1% [N=8] versus 6.0% [N=42]) (odds ratio=19.96, 95% confidence interval [CI]=6.64–60.09), a depressive disorder (28.6% [N=4] versus 7.0% [N=49]) (odds ratio=5.34, 95% CI=1.62–17.64), a disruptive disorder (42.9% [N=6] versus 11.0% [N=77]) (odds ratio=6.28, 95% CI=2.12–18.59), or a personality disorder (64.3% [N=9] versus 21.1% [N=148]) (odds ratio=6.81, 95% CI=2.24–20.62). Disruptive disorders (20.0% [N=2] versus 3.0% [N=21]) (odds ratio=7.43, 95% CI=1.49–36.98) and substance use disorders (30.0% [N=3] versus 5.0% [N=35]) (odds ratio=8.75, 95% CI=2.17–35.39) were more prevalent among adults with full bipolar disorder (N=10) than among adults without full bipolar disorder (N=707).
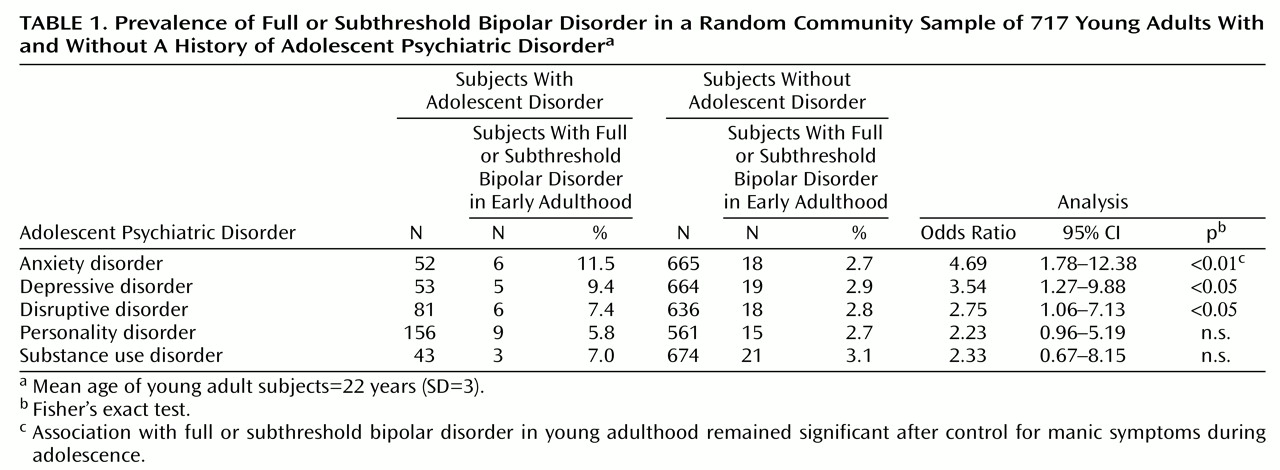
As
Table 1 indicates, adolescents with an anxiety, depressive, or disruptive disorder had elevated risk for full or subthreshold bipolar disorder during early adulthood. After adolescent manic symptoms were controlled statistically, only adolescent anxiety disorders remained significantly associated with full or subthreshold bipolar disorder in early adulthood. Full or subthreshold bipolar disorder in adolescence was associated with increased risk for early adulthood disruptive disorders before adolescent disruptive disorders were controlled statistically (odds ratio=4.36, 95% CI=1.21–15.70). However, there were no significant associations between full or subthreshold bipolar disorder in adolescence and anxiety, depressive, disruptive, or substance abuse disorders in early adulthood after corresponding disorders during adolescence were controlled statistically. Supplemental analyses indicated that adolescent anxiety disorders were associated with increased risk for early adulthood bipolar disorder even when cases of subthreshold bipolar disorder were not included (odds ratio=5.76, 95% CI=1.44–22.95) and that the findings were not attributable to overall patterns of psychiatric comorbidity or to the prevalences of anxiety, depressive, disruptive, substance use, or personality disorders.
Adolescent manic symptoms were associated with increased risk for early adulthood anxiety disorders (adjusted odds ratio=1.38, 95% CI=1.15–1.66) and depressive disorders (adjusted odds ratio=1.27, 95% CI=1.02–1.59) after corresponding adolescent diagnoses were controlled statistically. Specifically, adolescent manic symptoms were associated with new-onset or persistent generalized anxiety disorder, obsessive-compulsive disorder, and dysthymic disorder during early adulthood.
Discussion
The findings confirm that a wide range of psychiatric disorders co-occur with bipolar disorder among adolescents and young adults
(1–
6). More important, the present findings suggest that adolescents with anxiety disorders may be more likely than adolescents without anxiety disorders to develop clinically significant bipolar disorder symptoms by early adulthood. These findings are consistent with research suggesting that anxiety disorders may predict first onset of bipolar disorder
(1) and that adolescent anxiety disorders may increase risk for unipolar depression during early adulthood
(8).
In contrast with previous findings
(7), adolescents with attention deficit hyperactivity disorder were not at risk for clinically significant bipolar disorder symptoms during early adulthood after manic symptoms during adolescence were controlled statistically. It is important to note that because the Diagnostic Interview Schedule for Children does not assess hypomanic, mixed, or rapidly cycling episodes, it was not possible to investigate associations between these kinds of episodes and other psychiatric disorders. In addition, because there were few cases of bipolar disorder in this sample, statistical power concerns prevented us from reporting findings regarding psychiatric comorbidity associated with bipolar disorder. Nonetheless, including cases of subthreshold bipolar disorder in our analyses and investigating associations between psychiatric disorders and manic symptoms has permitted us to report findings that are directly relevant to the association between bipolar disorder and other psychiatric disorders.
Additional research is needed to investigate whether the presence of anxiety disorders may contribute to the onset of bipolar disorder or whether manic symptoms can contribute to the onset of anxiety disorders. The present findings suggest that individuals with anxiety disorders during adolescence should be monitored for signs of bipolar disorder during early adulthood and that anxiety and depressive disorders should be assessed among adolescents who have clinically significant manic symptoms. Previous research has suggested that identifying and treating co-occurring psychiatric disorders among individuals with bipolar disorder may help to alleviate the impairment and prolonged course that individuals with bipolar disorder and additional psychiatric disorders often experience
(3–
6).