What’s come to perfection, perishes.
—R. Browning: Old Pictures in Florence, Stanza 17
This concept of perfectionism by Robert Browning may be most apt for those with anorexia nervosa. A unidimensional definition of perfectionism is “the belief that a perfect state exists that one should try to attain”
(1). Over a century ago, Louis-Victor Marcé commented on the obstinate refusal of food of persons with anorexia nervosa
(2). A decade later, in a seminal account of the illness, the French physician Charles Lasegué cautioned, “Woe to the physician who, misunderstanding the peril, treats as a fancy without object or duration, an obstinacy which he hopes to vanquish by medicines”
(3). Lasegué further described in these patients an unrelenting pursuit of unusually rigid standards of propriety: “Ever on the watch for judgements concerning themselves, especially such as are approved by the family.” These references to a seemingly incessant demand for the highest possible standards of behavior and external approval have since found empirical support in psychometric studies showing significantly greater inflexibility, restraint, and perfectionism in the personalities of individuals with anorexia nervosa relative to healthy comparison subjects
(4–
7). Of added note, two other studies
(8,
9) found that scores on a measure of perfectionism
(10) were significantly greater in patients with anorexia nervosa relative to healthy comparison subjects, even after long-term weight recovery. In view of evidence of at least moderate heritability of perfectionism
(11) in studies of human personality, its prominence in anorexia nervosa, both acutely and postmorbidly, and strong evidence of familial transmission of anorexia nervosa
(12), it has been hypothesized that perfectionism is one of several related phenotypic temperamental or personality trait markers expressing a genotypic vulnerability to this illness
(13). However, it remains unknown if perfectionism in anorexia nervosa differs by clinical subtype (e.g., subjects who engage in strict dietary restriction versus purging or binge eating and purging) or is associated with other core behavioral features of the illness. Such questions are of theoretical importance, since personality factors may play a role in mediating phenotypic aspects of illness behavior
(14) among persons with eating disorders.
The present study examines multidimensional aspects of perfectionism in a cohort of affected family members selected for the presence of anorexia nervosa. These affected relative pairs were recruited to participate in a multinational genomic analysis of eating disorders, the goal of which was to map loci influencing susceptibility to anorexia nervosa and bulimia nervosa and to identify behavioral phenotypes associated with genetic heterogeneity in these syndromes. Data from perfectionism measures, along with data on obsessional behavior and pathological eating attitudes and behaviors, were obtained for a total of 322 women with a history of anorexia nervosa. We examined variation in perfectionism across clinical subtypes of anorexia nervosa as well as the covariation of perfectionism with these behavioral measures.
Method
Subjects
Participants with a history of anorexia nervosa were enrolled in an international, multicenter study examining the genetic basis of anorexia nervosa. Specific details of the study background, methods, proposed genome typing analysis, association analyses, and candidate gene studies have been previously reported
(14).
Relative pairs affected with anorexia nervosa were recruited through clinic services and advertising at seven sites in North America and Europe: the University of Pittsburgh, Weill Medical College of Cornell University, the University of California at Los Angeles, the University of Toronto, Maudsley Hospital in London, the University of Munich, and the University of Pennsylvania. Written informed consent was obtained after the study had been fully explained.
During the first contact, the initial respondent was questioned about eating disorders in her first- through fifth-degree relatives. If it appeared that a relative might be affected, permission to contact said person was obtained. It was necessary that the proband met criteria for a diagnosis of anorexia nervosa and that the co-affected relative met DSM-IV criteria for anorexia nervosa, bulimia nervosa, or eating disorder not otherwise specified. Additional proband-specific requirements were onset of anorexia nervosa before age 25 and no history of regular binge eating, obesity, serious medical illnesses, psychotic disorder, bipolar disorder, or known genetic disorder. The co-affected relative also had to have no history of obesity, serious medical illnesses, psychotic disorder, bipolar disorder, or known genetic disorder. If these criteria were met, informed consent was obtained and the proband and relative were enrolled in the study.
All subjects in the current study were female and met modified DSM-IV criteria for anorexia nervosa disorder (amenorrhea was not required). The 322 subjects were classified by anorexia nervosa subtype: restricting (N=146), purging (N=116), or binge eating and purging (N=60). Seventy-five of the subjects had no relative for the current analysis. Of the relative pairs, 79 were first-degree relatives, six were second-degree relatives, 11 were third-degree relatives, and seven were greater than third-degree relatives. There were 11 relative trios among the current data set (i.e., a proband with two other affected members of the same family). Of the trios, seven were first-degree relatives (e.g., three sisters), one contained a proband with a first-degree and a second-degree relative, one contained a proband with two second-degree relatives, and two contained a proband with two third-degree relatives. There were two relative quads—a proband with three other affected members of the same family. One of the quads was a proband with three first-degree relatives, and the other quad was a proband with two first-degree relatives and one second-degree relative. Subjects were a mean age of 28.2 years (SD=10.4, range=14–65).
The primary goals of this genetic study of anorexia nervosa were to use family-based association and linkage studies to identify susceptibility genes for the development of anorexia nervosa. Thus, the focus of the study was to ascertain and assess biological relatives affected with an eating disorder. As a result of this ascertainment strategy, we did not have access to a community comparison group of women that could be directly matched to the women with anorexia recruited for this study. Consequently, for the current study, data from 44 comparison female subjects who had served as a comparison group in a family study by Lilenfeld et al.
(15) were used for some of the analyses. These subjects were recruited by using a commercial mailing list and had no history of any eating disorder or eating disorder behaviors. They were excluded if they had weighed less than 90% or more than 125% of ideal body weight since menarche. The comparison subjects were a mean of 26.1 years of age (SD=6.2, range=17–41).
Measures
Multidimensional Perfectionism Scale
All subjects completed the Multidimensional Perfectionism Scale
(10), a self-report questionnaire that assesses six aspects of perfectionism (concern over mistakes, personal standards, parental expectations, parental criticism, doubts about actions, and organization) and yields an overall perfectionism score. Eating disorder participants were instructed to describe their symptoms when they felt that their eating disorder was most severe. The purpose of this strategy was to eliminate any ambiguity concerning their symptoms. This also allowed us to relate the Multidimensional Perfectionism Scale scores to severity of the eating disorder in the same time period. Data regarding validity of the Multidimensional Perfectionism Scale and its role in psychiatric disorders frequently comorbid with anorexia nervosa can be found elsewhere
(16–
19).
Eating Disorder Inventory-2
Two hundred sixty-two anorexia nervosa subjects (restricting subtype: N=109; purging subtype: N=105; binge eating and purging subtype: N=48) also completed the Eating Disorder Inventory-2
(20) (this information was not collected at the Munich site). Only data from the perfectionism subscale of the Eating Disorder Inventory-2 will be presented here. This second measurement of perfectionism was included because it has been the most frequently used index of perfectionism in subjects with eating disorders and thus allows comparison with other studies. In addition, the relationship between the perfectionism subscale of the Eating Disorder Inventory-2 and the overall measure of perfectionism from the Multidimensional Perfectionism Scale has not been assessed in a large cohort of anorexia nervosa subjects. By administering both questionnaires, we attempted a broader, more definitive empirical assessment of perfectionism in this cohort.
Yale-Brown Obsessive Compulsive Scale
Anorexia nervosa subjects at each site were also administered the Yale-Brown Obsessive Compulsive Scale, which is a reliable and valid semistructured interview
(21,
22). This instrument first generates a symptom checklist for both current and lifetime symptoms, then process-oriented questions are asked about the obsessions and about the compulsions. Both the checklist and the questions were completed only for the time that obsessions and compulsions were the most severe.
Yale-Brown-Cornell Eating Disorder Scale
The Yale-Brown-Cornell Eating Disorder Scale, a reliable and valid semistructured interview
(23,
24) that assesses core preoccupations and rituals that are related to food, eating, exercise, and the subject’s weight and body, was administered to each anorexia nervosa subject. Lifetime and current symptom checklists are generated and process-oriented questions are asked about the preoccupations and about the rituals. For the current analyses, only scores from time of worst symptoms are used.
Statistical Analyses
For each group of anorexia subjects, Pearson product-moment correlations were calculated between total score on the Multidimensional Perfectionism Scale and both scores on the perfectionism subscale of the Eating Disorder Inventory-2 and total score on the Yale-Brown Obsessive Compulsive Scale. Correlations were also computed between total score on the Multidimensional Perfectionism Scale and both lifetime lowest body mass index and total score on the Yale-Brown-Cornell Eating Disorder Scale, as well as with scores on the preoccupation, ritual, and motivation for change subscales of the Yale-Brown-Cornell Eating Disorder Scale. Since multiple correlations were conducted, only p values <0.01 were considered as significant. An intraclass correlation was computed for the Multidimensional Perfectionism Scale total score for sibling pairs by using the SAS version 7.0 VARCOMP procedure
(25).
Analysis of data sets in which some individuals are related is problematic, since the assumption of independent observations is violated because paired or clustered data are collected. Thus, mean differences on dependent measures among women with anorexia nervosa and comparison subjects were examined by using generalized estimating equations
(26–
28). Generalized estimating equations adjust the data to account for a genetic relationship between some of the subjects. Generalized estimating equations are a statistical approach based on regression techniques and are used to investigate correlated data, such as panel studies. It is thus well suited to the data from affected relative groups used in the current study. In the generalized estimating equations method, the correlated data are modeled with the same link function, the same linear predictor setup, and the same variance function as is used with a generalized linear model in the independent case. However, in the generalized estimating equations approach, the covariance structure of the correlated measures is also modeled. Specifically, by using the generalized estimating equations method, the existence of a relationship between observations in a particular cluster is assumed, whereas no relationship is assumed between observations of separate clusters. The relationships among observations within a cluster are then estimated by the generalized estimating equations method and treated as a nuisance variable in analyses. There are several choices for the form of this working correlation matrix, including a fixed correlation matrix, the identity matrix, an exchangeable correlation matrix, and an unstructured correlation matrix.
In the current study, biologically related family members constituted each cluster in the generalized estimating equations analyses. However, because the current study included family members of varying relatedness (i.e., first-, second-, and third-degree relatives as well as unrelated comparison subjects), the generalized estimating equations analyses were done in two steps. First, models were fit to data from the Multidimensional Perfectionism Scale, Eating Disorder Inventory-2, and the Yale-Brown Obsessive Compulsive Scale by means of the generalized estimating equations method; an exchangeable working correlation matrix was used for probands and their siblings only to obtain an estimate of the familial correlation among these first-degree relatives. Second, models were re-fit to the entire data set of relatives and unrelated comparison subjects by using familial correlations estimated from the probands and siblings as the user-defined working correlation matrix. The model parameters and statistics from these models were then used as the final solution. This approach to the analyses can be considered conservative, since the proband/sibling correlations used are likely overestimates of the expected correlations among clusters of unrelated individuals and second- and third-degree relatives. Such overestimation is likely to result in fewer rather than more significant findings.
In the second model, we examined Multidimensional Perfectionism Scale, Eating Disorder Inventory-2, and Yale-Brown Obsessive Compulsive Scale score differences between the three anorexia nervosa subtypes, excluding the comparison subjects, by using the site at which data were collected (“center”) and the interaction between center and diagnosis as covariates in analyses. Center was added as an additional clustering variable in the model, since it was believed that subjects from similar regions of the world might be more correlated for the scores than those from different regions. Results from these two models were then compared to determine if the inclusion of additional covariates influenced the results of the contrasts comparing anorexia subtypes. If they did not, then contrast results from the first model were reported in the tables and text for all groups. If findings did differ, then contrast results from both models were reported for comparison purposes.
An alpha level of p<0.05 was used for analyses of overall effects, while an alpha level of p<0.01 was used for contrasts between groups to control for the relatively large number conducted. All statistical analyses were conducted by using the SAS version 7.0 GENMOD procedure
(25).
Results
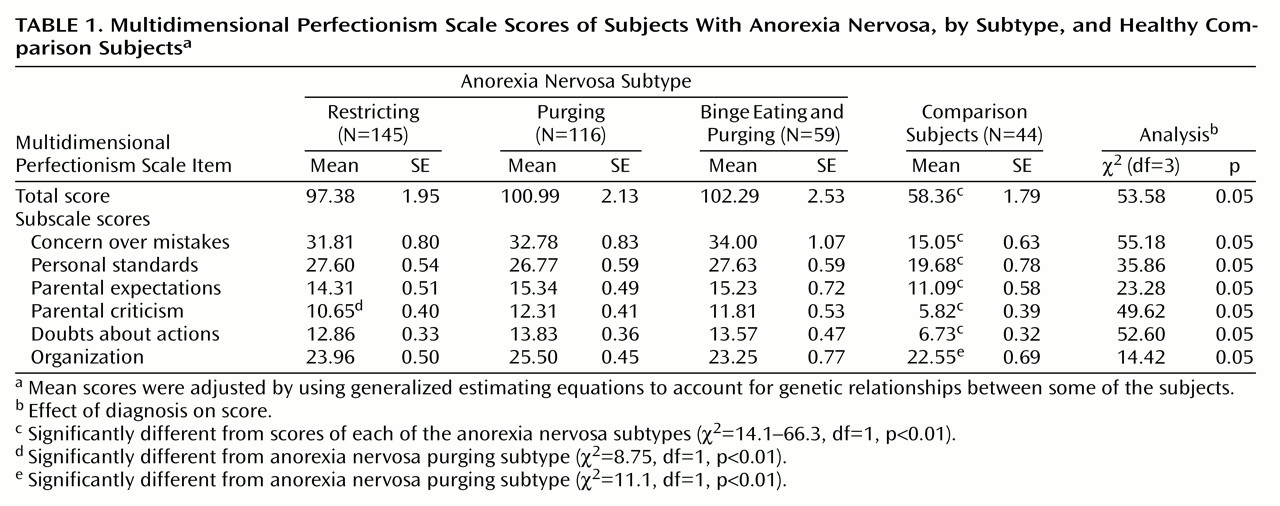
Table 1 presents the adjusted Multidimensional Perfectionism Scale scores across diagnostic groups. We noted that the healthy comparison subjects had slightly lower scores on all subscales of the Multidimensional Perfectionism Scale than previously reported normative data from a female college population
(19). (For reference, those scores were as follows: total score=67.3, concern over mistakes=17.7, personal standards=22.5, parental expectations=13.0, parental criticism=6.4, doubts about actions=7.7, organization=21.0.) The healthy comparison subjects in our study had significantly lower scores than each of the eating disorder groups for all subscales of the Multidimensional Perfectionism Scale except organization, where they differed only from the purging subtype. The only significant difference between any of the three anorexia nervosa subgroups was on parental criticism, where those with the restricting subtype of anorexia nervosa had significantly lower scores than the purging subtype. The intraclass correlation (ICC=0.21) for affected sibling pairs was not significant.
There were no significant differences in scores among the three anorexia nervosa subtypes on the perfectionism subscale of the Eating Disorder Inventory-2 (restricting: mean=9.37, SD=0.46; purging: mean=9.12, SD=0.47; binge eating and purging: mean=9.62, SD=0.62). The scores were not different from the normative data for anorexia nervosa subtypes reported by Garner
(20). Indeed, the mean perfectionism score of the restricting subjects in our study was in approximately the 50th percentile, and the mean score of the binge eating and purging subjects was in approximately the 48th percentile, of the Eating Disorder Inventory-2 norms for these subytpes. All three anorexia nervosa subtypes had mean scores above the nonpatient college female norms reported for the Eating Disorder Inventory-2, with the restricting and purging subtypes in approximately the 82nd percentile and the binge eating and purging subtype in approximately the 84th percentile.
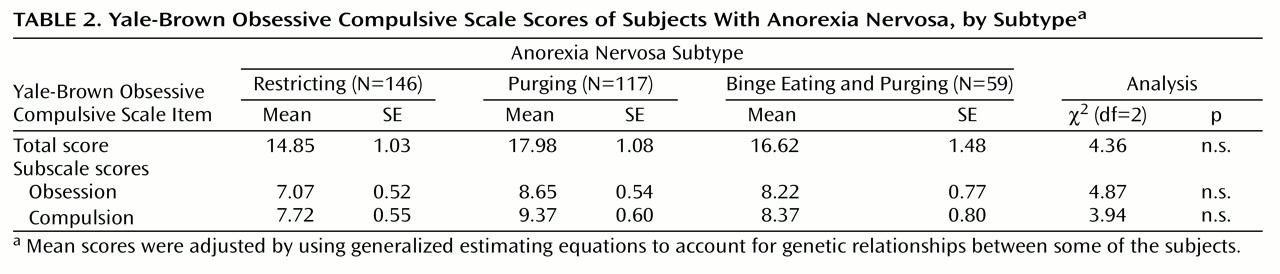
There were no significant differences between the anorexia nervosa subgroups on any of the Yale-Brown Obsessive Compulsive Scale scores (
Table 2.
There were no significant interactions between site and diagnosis for any of the scores. When the analyses were rerun without the interaction, the following scores had significant site effects (df=6 and p<0.01 for all analyses): Multidimensional Perfectionism Scale total score (χ2=23.47), concern over mistakes (χ2=22.14), personal standards (χ2=25.08), doubts about actions (χ2=21.03), organization (χ2=26.25), and obsessions (χ2=16.47) from the Yale-Brown Obsessive Compulsive Scale. For all Multidimensional Perfectionism Scale scores that had a significant effect of site, the Munich site had significantly lower scores than Los Angeles, Toronto, and London. Munich was also significantly below Pittsburgh on four of the Multidimensional Perfectionism Scale scores (total, concern over mistakes, personal standards, and organization), and below New York on personal standards and organization. The effects of diagnosis between subgroups of anorexia nervosa with site entered as a covariate were identical to those without site entered as a covariate. Munich was significantly below Los Angeles and Toronto, and London was significantly lower than Los Angeles, for the Yale-Brown Obsessive Compulsive Scale obsession score. There were no site differences for scores on the perfectionism subscale of the Eating Disorder Inventory-2.
The two measures of overall perfectionism (the Multidimensional Perfectionism Scale total and the Eating Disorder Inventory-2 perfectionism subscale) were significantly correlated (p<0.01) for the restricting (r=0.64, df=108), purging (r=0.71, df=104), and binge eating and purging (r=0.75, df=47) anorexia nervosa subtypes. The Multidimensional Perfectionism Scale total was also significantly correlated with Yale-Brown Obsessive Compulsive Scale total scores for the restricting (r=0.41, df=145), purging (r=0.28, df=116), and binge eating and purging (r=0.34, df=58) anorexia nervosa subtypes. The Yale-Brown Obsessive Compulsive Scale total score was significantly correlated with the Eating Disorder Inventory-2 perfectionism subscale score for the restricting (r=0.41, df=108) and purging (r=0.22, df=104), but not the binge eating and purging (r=0.11, df=47), anorexia nervosa subtypes.
Overall perfectionism (total score on the Multidimensional Perfectionism Scale) was also significantly positively correlated (p<0.01, df=319 for all) with the Yale-Brown-Cornell Eating Disorder Scale total score (r=0.32) and its subscales (preoccupations: r=0.28, rituals: r=0.32, motivation for change: r=0.23) and was negatively correlated with lifetime lowest body mass index (r=–0.20, df=319, p<0.01). Thus, subjects who were more perfectionistic when their eating disorder was at its worst generally had more preoccupations and rituals, were less motivated to change (higher motivation scores reflect increased pathology), and had a lower lifetime lowest weight.
Discussion
The present study is the largest to date to examine the role of perfectionism in anorexia nervosa. The findings from 322 women with anorexia nervosa from seven different sites showed that those with anorexia nervosa scored significantly higher on the Multidimensional Perfectionism Scale than healthy comparison subjects. In addition, they scored higher on the perfectionism subscale of the Eating Disorder Inventory-2 compared to normative data for this instrument. These two measures of overall perfectionism were highly correlated within each of the three anorexia nervosa subtypes, which indicates that they were measuring the same underlying personality construct.
The present results support the notion that perfectionism is a prominent feature of the personality background of individuals affected with anorexia nervosa. The profile of scores on the Multidimensional Perfectionism Scale indicated that subjects with anorexia nervosa were distinguished from healthy comparison subjects by their more strenuous efforts at, and preoccupations with, avoidance of mistakes in daily life and of parental criticism, doubts over the correctness of actions, and more extreme adherence to personal and parental standards of excellence. Only perfectionistic strivings in organization activities failed to separate anorexia nervosa subjects from comparison subjects. On balance, our findings concur with evidence of an association between perfectionism and drive for thinness in nonclinical subjects
(29) and elevated perfectionism in malnourished
(8) and weight-restored patients with anorexia nervosa
(9).
A unique new finding in the present study is the observation that levels of perfectionism were greater in each of the three anorexia nervosa subtypes than in the healthy comparison subjects. Within the clinical sample, anorexia nervosa subjects who engaged in purging behaviors alone (i.e., without binge eating) had higher parental criticism scores than did anorexia nervosa subjects who engaged in restricting behaviors. Previous studies
(30) have shown that the purging subtype of anorexia nervosa is associated with more pathology than that found among anorexic patients who engage in purely restricting behaviors. In a study with results similar to those of the current study, Garner and his colleagues
(30) found no differences in scores among these three groups on the perfectionism subscale of the Eating Disorder Inventory-2. However, they did report that obsessive-compulsive symptoms (as measured by the HSCL-58) were more prominent in subjects with the purging subtype of anorexia nervosa than in those with the restricting subtype. Although in the current study there were no significant anorexia nervosa subtype differences on the Yale-Brown Obsessive Compulsive Scale, the restricting subjects tended to have lower Yale-Brown Obsessive Compulsive Scale scores than the purging subjects, which parallels Garner’s findings. From these patterns, we speculate that increased perfectionism among purging anorexic patients indicates more desperate efforts at attaining a thin ideal and may be mediated by greater extremes of perfectionism and related personality phenotypes.
Differences between anorexia nervosa subtypes were identical when site was entered as a covariate. Thus, it appears that the site at which the data were collected did not significantly influence perfectionism scores in anorexia nervosa. Site differences for perfectionism were found only for Munich, whose subjects scored significantly lower on almost all Multidimensional Perfectionism Scale subscales, except parental criticism and personal standards, than subjects recruited at the North American and London sites. Participants from the Munich site were also rated significantly lower on obsessive scores from the Yale-Brown Obsessive Compulsive Scale than subjects from the North American sites. There are several possibilities that could account for the differential response of Munich subjects to the perfectionism scales. First, in spite of careful translation from English to German and back-translation, there may have been subtleties of perfectionism lost in the process of translation. Second, all of the other sites were in English-speaking countries, or countries in which English is the major language. It is possible that there are subtle differences in the German culture from English-speaking cultures as to how patients respond to questionnaires and express themselves. Third, the comparison group for the Multidimensional Perfectionism Scale was from the United States; there was no corresponding German comparison group. The possibility that perfectionism and obsessionality are less prominent in German individuals with anorexia nervosa cannot be discounted.
Hewitt et al.
(29) speculated that a strong need for perfectionist self-presentation can influence eating behavior by not allowing the person to display imperfections or admit to difficulties. Other facets of perfectionism related to eating disorders are the tendencies of these individuals to view achievements in black-and-white terms, such that anything less than perfection is commensurate with failure. Hewitt et al.
(29) suggested that the striving for perfection is part of a strong drive in anorexia nervosa patients to gain approval of others by demonstrating conformity to expectations. In a study that used their own perfectionism scale, Hewitt et al.
(29) found that self-oriented perfectionism was specifically linked to dieting and to concerns with being thinner. Likewise, Mitzman et al.
(31), using a self-report questionnaire that measured neurotic perfectionism, found that patients with anorexia nervosa had significantly higher ratings than did healthy comparison subjects, while Davis et al.
(32) found that a high level of exercise in anorexia nervosa patients was associated with higher scores on perfectionism.
Anorexia nervosa subjects in the current study were more perfectionistic than comparison subjects when their eating disorder was at its worst. Moreover, increasing perfectionism was associated with lower body weight and greater prominence of eating preoccupations and rituals, as well as diminished motivation to change. Thus, greater severity of eating disorder symptoms was associated with greater perfectionism.
There are certain limitations in the present study. First, we used comparison subjects from only a single site. However, the comparison group had only slightly lower Multidimensional Perfectionism Scale scores than the normative data reported by Frost and his colleagues
(19), and they were matched closely to our anorexia nervosa groups with respect to age. Second, familial cases of anorexia nervosa may not be representative of cases of anorexia nervosa selected at random from the general population, spuriously inflating the overall prominence of perfectionism and other personality traits among affected individuals. As evidence suggests that anorexia nervosa and perfectionism may have heritable components
(33), and if it is the case that two traits share genotypic factors in common, then the perfectionism scores in this group may not generalize to the larger population of individuals with nonfamilial forms of anorexia nervosa. However, as shown by Strober and colleagues
(12), only a small minority of people (6.6%) with anorexia nervosa have affected first-degree relatives. Furthermore, the intraclass correlation of affected sibling pairs was not significant, which indicates that perfectionism was not more characteristic of sibling pairs than for nonsiblings. Thus, we believe it is unlikely that the current findings are seriously confounded by the use of familial cases.
In sum, this international multisite study provides strong support for perfectionism as a robust characteristic of anorexia nervosa. Perfectionism, along with related personality phenotypes, may constitute quantitative behavioral measures associated with genetic susceptibility for anorexia nervosa.