Unipolar major depression is estimated to be the fourth most important illness leading to functional disability worldwide, and its impact in this respect is expected to grow
(1). In terms of physical, social, and role functioning, patients with depressive syndromes suffer comparable or worse disability than those with chronic major medical conditions
(2). The annual cost of depression in the United States has been estimated to be about $43 billion
(3), making it one of the 10 most costly illnesses. Indirect costs of depression accounted for almost three-fourths of this amount, and absenteeism and lost productivity at work accounted for more than half
(3). In Finland, the rise in the annual number of disability pensions granted for major depression has been of increasing concern
(4). However, the major public health and economic impact of disability caused by major depression has not received sufficient attention in research and education.
A meta-analysis by Mintz et al.
(5) confirmed that treatments producing symptomatic recovery in depressed patients can also be effective in restoring the patients’ functional ability. Therefore, an investigation of treatment received by subjects granted a disability pension because of depression is warranted to evaluate appropriate measures for preventing disability. We report here findings from a random nationwide sample of subjects in Finland who were granted a disability pension for DSM-III-R major depression during a 12-month period in 1993–1994.
Method
In Finland, employees aged 65 years or younger are eligible for a disability pension after 1 year of continuous disability; they are also eligible for a daily allowance from sickness insurance for 300 work days. The health status of a pension claimant is described in the form of a standard medical statement, which is always prepared by a physician and is divided into three parts. The first part contains the person’s demographic data and medical history, medical status, and functional capacity. The second part details the treatment(s) received, and the third details the claimant’s job and the physician’s assessment of his or her impairment(s).
The basic population of the present study were all subjects living in Finland who were granted a new disability pension on the grounds of a primary diagnosis of DSM-III-R major depression during the 12-month period from October 1, 1993, to September 30, 1994. This time period was chosen because until September 30, 1994, all files on subjects who had claimed a pension were kept at the premises of the Social Insurance Institution in Helsinki. At present the register is no longer fully epidemiologically representative because it does not include all pensions. DSM-III-R criteria (with a few minor modifications) were the basis for the official classification of mental disorders in the Finnish version of the ICD-9 in 1987–1995.
The subjects for the systematic random sample were drawn from the Social Insurance Institution’s Disability Pension Register, in which the main diagnoses appear in the form of a three-digit code. We initially included all subjects who had been granted a new disability pension during the study period with a main diagnostic code of 296 (major depression) (N=2,567). Altogether, 349 randomly chosen subjects with the code 296 were drawn. Seventy-two (21%) were then excluded on the grounds of a diagnosis of depressive disorder not otherwise specified, bipolar I disorder, bipolar disorder not otherwise specified, dysthymia, or an unspecified type of depression or because medical statements were missing (N=3). Thus the final study group comprised 277 subjects with a main diagnosis of DSM-III-R major depression as the primary cause of their disability pension (79% of the 349 drawn). According to Finnish legislation, personal written informed consent was not needed because the study was record-based and approved by the Finnish Ministry of Social Affairs and Health.
The vast majority of the medical statements were written either by a psychiatrist (N=214 [77%]) or a psychiatric resident (N=40 [14%]) under the supervision of a psychiatrist. For 261 subjects (94%), the physician who prepared the statement was also responsible for the treatment received. The dose ranges given as the usual adult doses in the American Psychiatric Association Practice Guideline for Major Depressive Disorder in Adults
(6) were used to classify the antidepressant treatment into usual (adequate) or insufficient doses; adequate dose ranges for the antidepressants not available in the United States in 1993 were taken from other sources.
Results
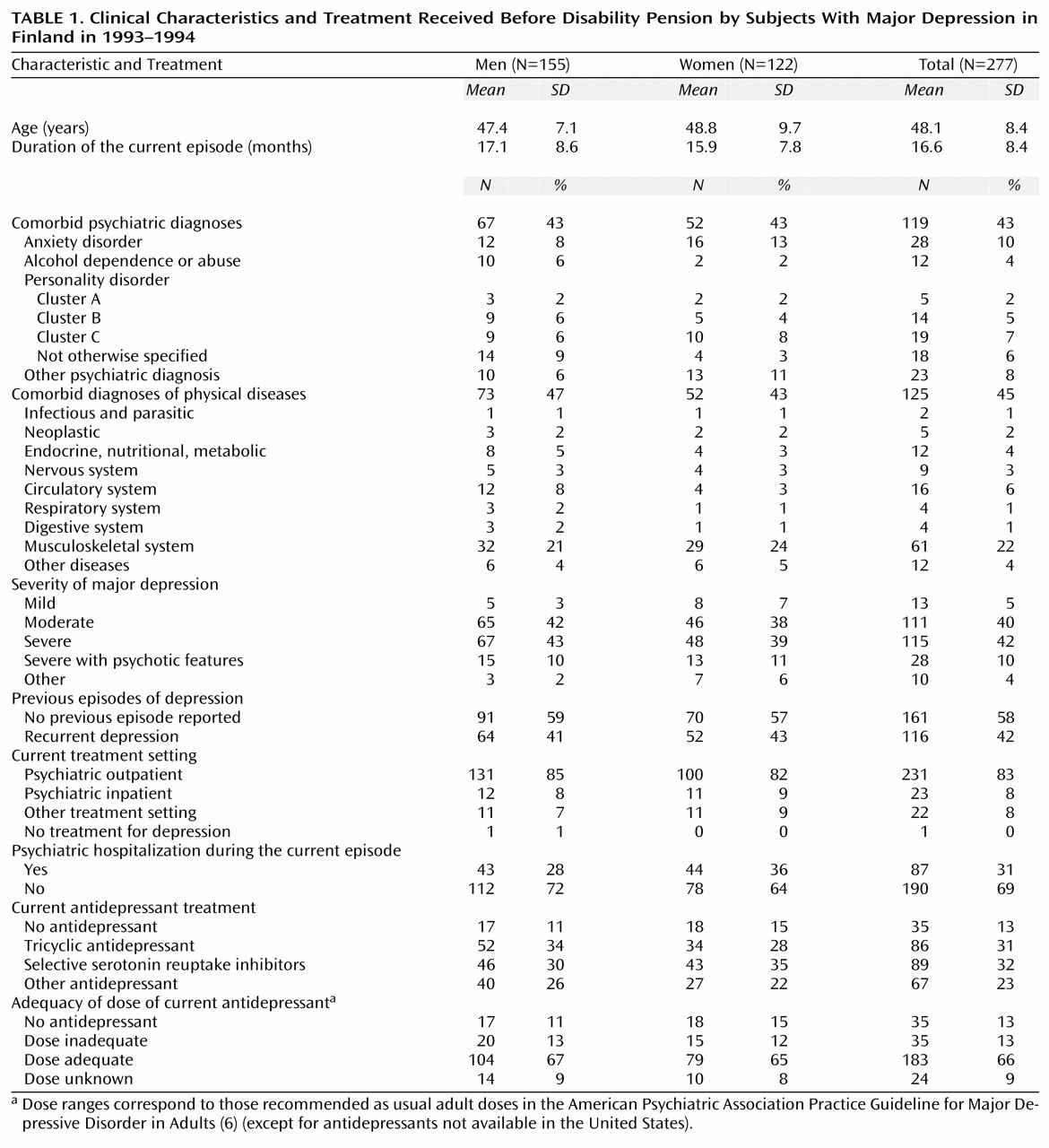
The sample comprised 155 male and 122 female subjects between age 17 and 63 years. The majority were married (N=161 [58%]). Almost half were blue-collar workers (N=120 [43%]), and the remainder mainly lower-level (N=49 [18%]) or higher-level (N=58 [21%]) employees. Two-thirds of the male and female subjects had a comorbid psychiatric or medical diagnosis contributing to the disability (
Table 1). Subjects with a comorbid musculoskeletal disease represented the largest subgroup of subjects with a comorbid disorder (N=61 [22%]).
Most subjects had received some treatment for depression before they applied for a disability pension; only 14 (5%) of the statements mentioned no pertinent treatment for the depressive episode. Patients treated in psychiatric settings were more likely to have received antidepressants than those treated elsewhere (230 [91%] of 254 versus 12 [52%] of 23) (χ2=24.8, df=1, p<0.001, with Yates’s correction). Inadequate antidepressant dosing was far more common with tricyclic antidepressants (29 [37%] of 78) than for SSRIs (one [1%] of 78) and other antidepressants (five [8%] of 62) (χ2=41.4, df=2, p<0.001). Only 24 (9%) of the subjects had received weekly psychotherapy, 11 (4%) ECT, and three (1%) lithium. Less than half of the subjects (N=109 [39%]) reportedly received a course of another antidepressant before the current one.
More of the subjects with a negative attitude toward psychiatric care (16 [37%] of 43) than those without a negative attitude (19 [8%] of 234) according to the medical statements were not receiving antidepressants (χ2=25.3, df=1, p<0.001, with Yates’s correction). Only five (2%) of the subjects had made an earlier, unsuccessful application for a disability pension on the basis of a psychiatric disorder. Twenty-two (8%) had made an unsuccessful application on the basis of a somatic disease; in two-thirds of these the application was made on the basis of a musculoskeletal disease.
Discussion
To our knowledge, this is the first nationwide investigation of the characteristics and treatment received by subjects before they were granted a disability pension for major depression. We found that most subjects receiving a disability pension for major depression had comorbid mental or physical disorders contributing to their disability. Most were prescribed antidepressant treatment, but it appears that less than half received sequential antidepressant trials, and few received pharmacological augmentation or effective nonpharmacological treatments.
Although this study’s major strength is that the subjects were representative of all new disability pensions in one country during 1 year, there were methodological limitations. First, we had no nationwide comparison group of patients with depression in Finland; therefore, we could not investigate risk factors for disability. Second, the study was completely record-based. The reliability and validity of, for example, the clinical diagnoses of DSM-III-R major depression are unknown. On the other hand, the attending psychiatrist reported that the patient had major depression, and it is therefore pertinent to investigate how it was treated. Furthermore, a survey of a large sample of Finnish psychiatrists in 1995
(7) found that their knowledge of the DSM-III-R criteria for major depression was quite good. The third limitation to the study is that the medical statements are not research instruments but standardized forms designed to yield relevant information to enable insurance company experts to decide on eligibility for disability pensions. This information is generally highly relevant, and the quality of reporting is good, but the amount of treatment actually given may have been underreported.
A disability pension for major depression is usually granted only if there is evidence that treatment efforts have failed to restore the patient’s functional capacity. This does not necessarily mean that the treatment received was optimal, but the vast majority of the subjects in our study group (N=263 [95%]) had received some relevant treatment. At least two-thirds had received antidepressants in doses that have been found effective in clinical trials
(6). Therefore, to prevent disability, the questions that need to be addressed are more problems of refractory depression
(8). Sequential trials of antidepressants were reported in only 108 (39%) of the subjects; whether the earlier antidepressant was switched because of lack of response, side effects, or other reasons is not known.
It appears that many of the patients (up to 169 [61%]) may have actually received only a single trial of an antidepressant before being granted a pension. Moreover, the other biological treatment methods pertinent to refractory depression, e.g., lithium augmentation, were remarkably rare. That only 11 (4%) of the subjects reportedly received ECT during the current episode is noteworthy in view of the facts that 86 (31%) were hospitalized during this time and 144 (52%) had been assigned a clinical diagnosis of severe depression with or without psychotic features. The percentage of subjects receiving weekly psychotherapy was also strikingly low. In addition, it may be that a small minority of patients become disabled because of their refusal to accept antidepressants or psychotherapy.