There is growing evidence that major depression and even subthreshold depression is associated with higher rates of mortality in patients with medical illness
(1–
11). Although earlier studies questioned whether depression is simply a marker for severity of illness, more recent investigations have found this relationship to be significant, even after controlling for the severity of illness and age
(10). This association has been best established in patients with cardiovascular disease
(2,
3,
5) and stroke
(6) but has been less well-demonstrated in general populations
(12) and for other diagnoses
(10). One study
(11) found that depression raised in-hospital mortality rates but had no effect on mortality rates after discharge. In a study of patients recruited from both medical and surgical wards
(4), the presence of depression continued to be a risk factor for 30 months after the diagnosis.
Despite this relationship between depression and mortality, little attention has been paid to what criteria for a diagnosis of depression best predicts mortality, partly because an accurate diagnosis of depression in the medically ill is difficult
(13). Low levels of depressive symptoms, grief-like symptoms, and demoralization are common in the medically ill
(14). Symptoms of depression are also caused by physical illness, treatments, and the experience of hospitalization
(14,
15). Many solutions to these diagnostic problems have been discussed in the literature
(11,
15,
16). Some
(11) have suggested that diagnostic criteria modified for use in the medically ill are as accurate in making a diagnosis of depression in this population as are criteria that include all symptoms regardless of etiology. To our knowledge, no one has examined which diagnostic scheme best predicts mortality.
DSM-IV criteria for diagnosing depressive disorders are difficult to operationalize in the medically ill. For a major depressive episode, DSM-IV states, “Do not include symptoms that are clearly due to a general medical condition,” but does not specify how this should be accomplished. Because a clear severity rating for each symptom is not mentioned in DSM-IV, less severe symptoms, which are common in the hospitalized medically ill
(14), might erroneously be counted as present by the inexperienced interviewer. To address these problems, one of us (S.V.A.C.) proposed modifications of DSM-IV criteria for use in the medically ill
(13); these are described in the Method section.
There is some suggestion
(3,
5) that a past history of depression may predict medical morbidity and perhaps mortality, independent of current depression. Frasure-Smith et al.
(3) suggested that a past history of depression is an independent predictor variable of post-myocardial-infarct events. However, to our knowledge, no studies have shown that a history of depression is an independent predictor of death in hospitalized medically ill patients. A second related issue is whether primary depression (depression that predates illness) or secondary depression (depression that follows illness) is more likely to predict mortality
(17). To our knowledge, there are no studies that address this issue.
Method
Study Group
All consecutive admissions to the adult medical wards of a university hospital in Florianopolis, Brazil, over a 5-month period were eligible to participate (N=392). The hospital is a 250-bed teaching hospital affiliated with the Federal University of Santa Catarina. The general medical wards have a total of 90 beds (60 for male patients and 30 for female patients). Of the 392 patients considered for interview, 241 (61.5%) were interviewed within the first 3 days after admission and 151 (38.5%) were excluded. Of the exclusions, 46 were unable to complete the interview due to severe physical illness, 62 were unable to complete the interview due to delirium or dementia according to DSM-IV, 28 were discharged before 3 days, 11 were given antidepressants during their hospitalization, and four patients refused to participate in the study.
Procedures
An experienced consultation-liaison psychiatrist (L.M.F.) with training in the use of the Schedule for Affective Disorders and Schizophrenia (SADS)
(18) interviewed all study subjects. Data on demographic and medical variables as well as history of psychiatric disorders were collected from the medical chart and during the psychiatric interview, which included the SADS. Mortality and length of stay during the index hospitalization were recorded for each patient.
The protocol was approved by the Institutional Review Board at the Federal University of Santa Catarina in Florianopolis, and written informed consent was obtained from all patients before they were interviewed.
Depressive Diagnoses
All patients participating in the study were diagnosed according to both the modified and inclusive criteria for depression. The DSM-IV diagnosis of major depressive disorder based on criteria modified for use in the medically ill
(13) was made in the following manner. The qualifying affective symptom was depression, anhedonia, or hopelessness. Although hopelessness was deleted as a qualifying affective symptom in DSM-III-R, it continues to be useful, particularly in the elderly
(13), who may not report depression or anhedonia. For the associated symptoms of depression, several clarifying questions were designed to eliminate depressive symptoms easily explained by physical illness, treatments, and/or the hospital environment. For the associated symptom to be counted, its onset had to coincide or intensify with the onset of the qualifying affective symptom(s). A modified diagnosis of minor depressive disorder was made according to DSM-IV by using these same criteria.
For the inclusive diagnoses of major and minor depressive disorder, the qualifying affective symptom(s) were depression and anhedonia; all associated symptoms of depression were counted when present regardless of etiology.
For both the modified and inclusive diagnoses, the SADS questions, which have been translated into Portuguese and found to be reliable and valid in a Brazilian population
(19), were used to assess symptom severity. The score for SADS items, except depressed mood and suicidality, ranges from 1 to 6 (1=not at all, 2=slight, 3=mild, 4=moderate, 5=severe, 6=extreme). Depressed mood and suicidal ideation are scored from 1 to 7 (1–6 are scored as are the rest of the items, and 7=very extreme). Cutoffs were suggested by the DSM-IV diagnoses for major and minor depressive disorder. For all symptoms except suicidal ideation, weight loss, and insomnia, a cutoff score of 4 or higher was required for the symptom to be counted. A cutoff of 3 or higher was used for insomnia (“often has some significant difficulty sleeping”) and weight loss (“five to ten pounds per month,” which corresponds to DSM-IV “5% of body weight per month”). A cutoff score of 2 or higher was used for suicidal ideation (“Thoughts of death,” “I would be better off dead,” “I wish I were dead”). For both modified and inclusive diagnoses of major and minor depressive episodes, symptoms had to be present for 2 weeks.
The history of past psychiatric illness was made according to part II of the SADS. Questions regarding character pathology were not asked.
Patients who were depressed were asked which came first—the depression or the nonpsychiatric medical illness. A depression that occurred before the medical illness was considered a primary depression, and depression that occurred after the onset of the medical illness was considered a secondary depression
(18).
Physical Morbidity
We used five measures of physical morbidity:
The disease responsible for hospitalization was coded according to ICD-9. This does not take into account the severity of this diagnosis or the number of other concurrent diagnoses.
Severity of illness was measured by using the Charlson combined age-comorbidity index
(20,
21), a weighted index that takes into account the patient’s age (a significant risk factor for death) as well as the number, type, and severity of the patient’s illnesses. This measure was shown to be a valid predictor of risk of death in several longitudinal studies
(1,
20,
21).
Pain/discomfort numerical rating scales
(22,
23) were used to rate the patient’s pain/discomfort for that day. On a scale from 0 to 100, 0 indicated no pain/discomfort and 100 indicated symptoms “so severe that the patient can’t stand it.”
Length of stay was measured for each patient in days from admission to discharge or death.
We also measured the number of weeks since the diagnosis was made of the primary illness that was responsible for the hospitalization.
Statistical Analysis
Data were analyzed by using SPSS for Windows (version 8.0, SPSS, Chicago). All statistical tests were two-tailed; p≤0.05 was considered statistically significant. Categorical variables were compared by using chi-square tests or Fisher’s exact tests as appropriate. Ordinal and continuous variables were assessed by using Mann-Whitney tests.
The primary outcome measure was death during the index hospitalization. Univariate logistic regression was used to evaluate the relationships between the predictor variable and outcome. Variables with skewed distributions were transformed with the natural logarithm before regression analyses were performed. Multivariate logistic regression was performed for all univariate variables that were significant at p≤>0.10 to determine their independent associations with death.
We used receiving operating characteristic curve analysis and area under the curve analysis as aids in choosing the best cutoff for accuracy-of-prediction classification table. The internal consistency reliability of the depressive symptoms used to make modified diagnoses and inclusive diagnoses was assessed by using Cronbach’s alpha.
Results
Twenty (8.3%) of the 241 patients in the study group died.
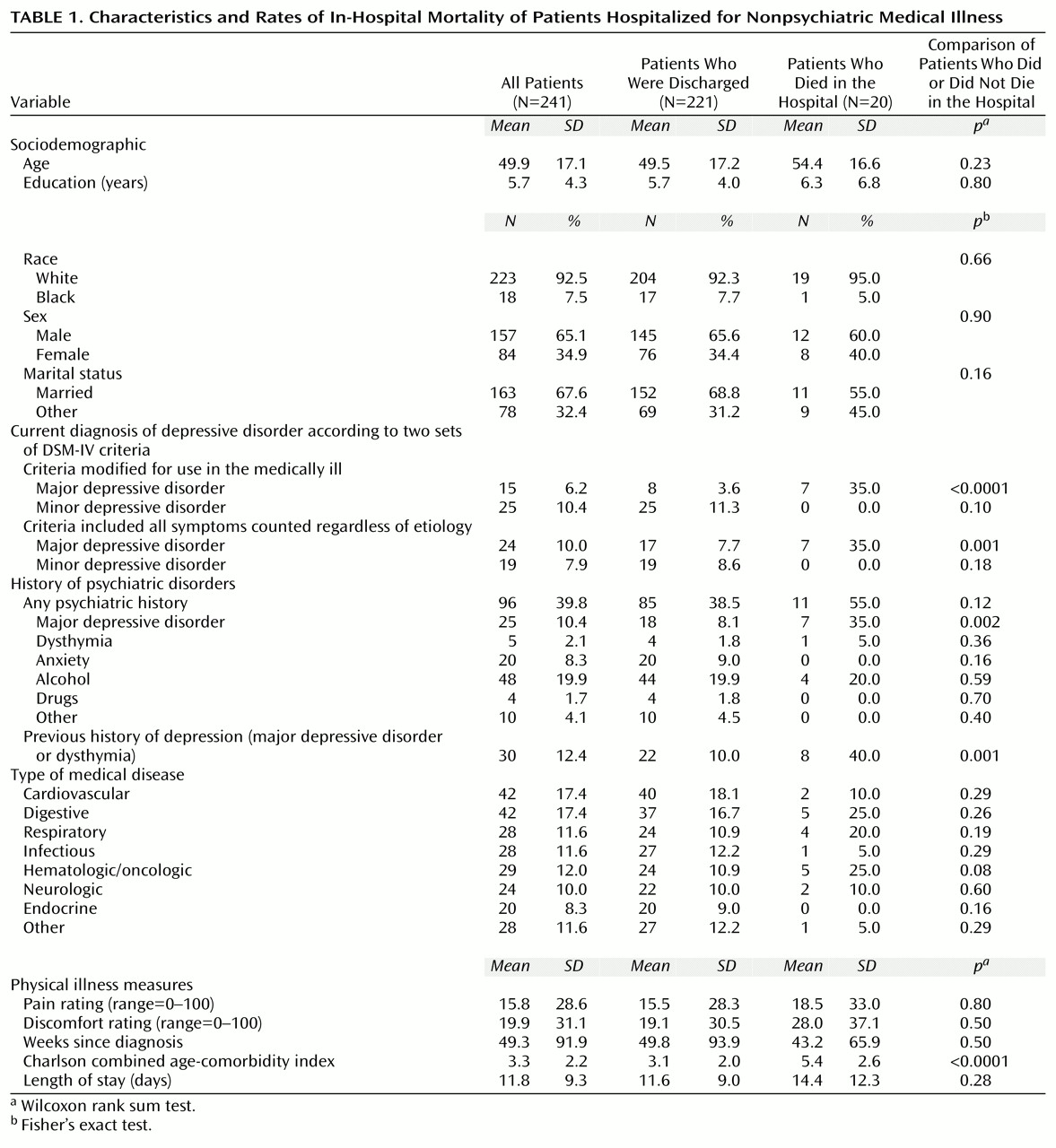
Table 1 provides information on the patients’ characteristics.
When compared with the 241 patients included in the study, the 151 patients who were excluded were older (mean age=65 years, SD=18.4) (z=5.23, p=0.01); were no different in gender (N=47 [31%] female and N=102 [68%] male) (χ2=0.41, df=1, n.s.); had a higher Charlson combined age-comorbidity index (mean=5.6, SD=2.43) (z=5.90, p=0.01); showed no difference in the length of stay (mean=14 days, SD=12) (z=0.43, n.s.); and had a higher mortality rate (N=26 [17%]) (χ2=4.98, df=1, p=0.03).
Modified and Inclusive Diagnoses of Depression
Of the 24 patients with an inclusive diagnosis of major depressive disorder, 13 had a modified diagnosis of major depressive disorder and 11 had a modified diagnosis of minor depression. Of the 19 patients with inclusive diagnoses of minor depression, 13 had a modified diagnosis of minor depression and six had no depressive diagnosis. As would be expected, the modified criteria for major depressive disorder resulted in fewer diagnoses of major depression but more diagnoses of minor depression.
Using Cronbach coefficients, we found that the internal consistency reliability of the depressive symptoms used to make modified diagnoses was 0.86; the reliability of the symptoms for an inclusive diagnoses was 0.82.
Primary Versus Secondary Depression
Eight (53.3%) of the 15 patients with a modified diagnosis of major depressive disorder, 14 (58.3%) of the 24 patients with an inclusive diagnosis of major depressive disorder, 10 (40.0%) of the 25 patients with a modified diagnosis of minor depression, and five (26.3%) of the 19 patients with an inclusive diagnosis of minor depression experienced the depression before their nonpsychiatric medical illness (Fisher’s exact p=0.99 for all). Thus, whether the depression came before or after the illness did not predict mortality in any diagnostic group.
Logistic Regression
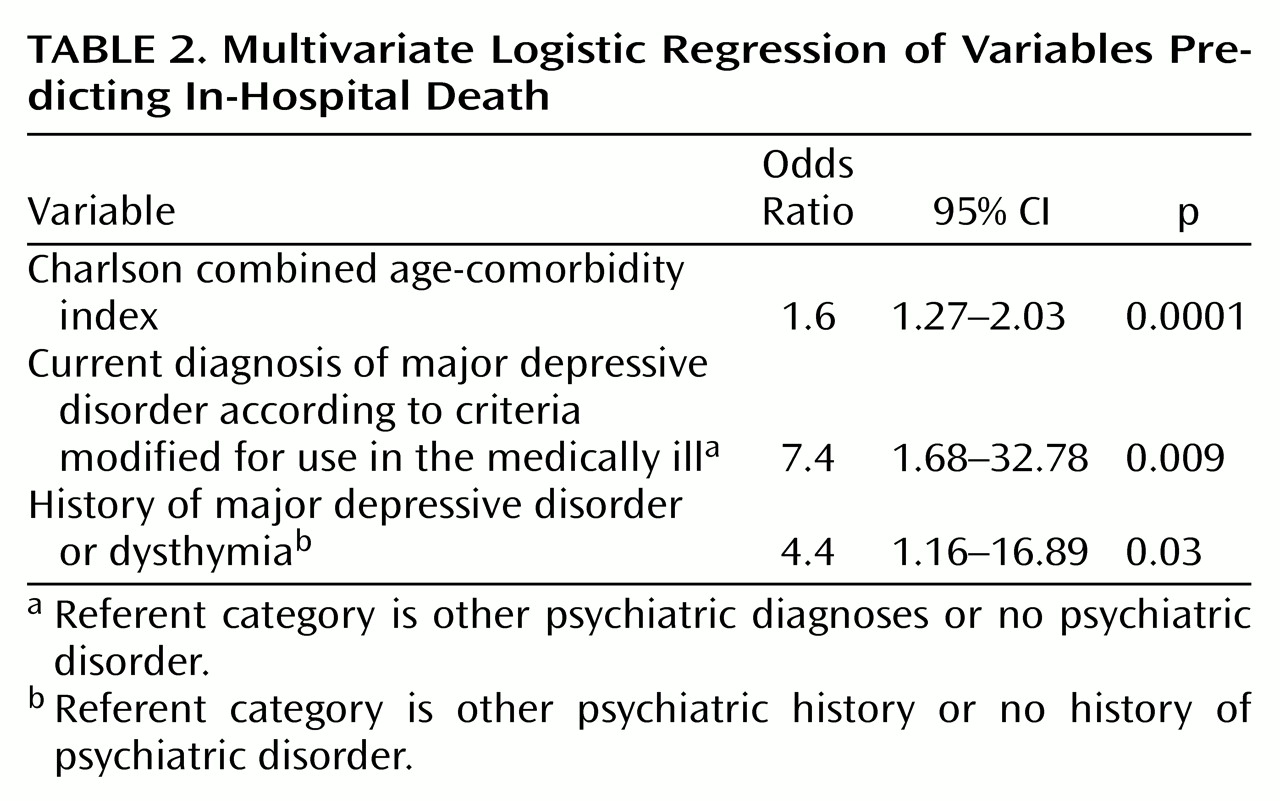
Logistic regression was performed for all univariate predictor variables that were significant at p≤0.10. After adjustment for the Charlson combined age-comorbidity index, the following characteristics of the study group were found to predict mortality: modified diagnosis of major depressive disorder (odds ratio=15.5, 95% confidence interval [CI]=4.02–60.10, p>0.0001); inclusive diagnosis of major depressive disorder (odds ratio=5.8, 95% CI=1.85–18.49, p>0.004); past history of major depressive disorder (odds ratio=9.0, 95% CI=2.66 to 30.90, p>0.0007); and past history of major depressive disorder and dysthymia (odds ratio=8.5, 95% CI=2.69–27.20, p>0.0004). No other demographic variables, diagnostic categories, past history variables, other illness measures, or medical diseases were found to be significant.
Both univariate and multivariate logistic regression showed the modified diagnosis of major depressive disorder to have a higher odds ratio and smaller p value than the inclusive diagnosis of major depressive disorder. As a result, the modified diagnosis of major depressive disorder was included in the final multivariate model.
A history of major depressive disorder and dysthymia, rather than a history of major depressive disorder alone, was chosen for the final model because major depressive disorder and dysthymia had a slightly lower p value in both univariate analysis and after adjustment for Charlson combined age-comorbidity index.
Table 2 shows the final multivariate model.
We also performed the same multivariate logistic regression using a history of major depressive disorder alone rather than a history of major depressive disorder and dysthymia. The results of this regression were similar: for the Charlson combined age-comorbidity index, beta=0.47, beta SE=0.12, odds ratio=1.61, 95% CI=1.27–2.04, p>0.0001; for the modified diagnosis of major depressive disorder, odds ratio=8.02, 95% CI=1.87–34.31, p>0.005; and for a past history of major depressive disorder, odds ratio=4.6, 95%, CI=1.87–34.31, p>0.03.
We used the receiver operating characteristics curve as an aid to finding the best tradeoff between sensitivity and specificity produced by the multivariate model shown in
Table 2. For the prediction classification table, we chose a value of 6% because it produces good sensitivity (75%), specificity (72%), and overall accuracy of prediction (78%). The area under the receiving operating characteristics curve was 0.82.
Discussion
This study supports the growing evidence that depression, independent of severity of illness, predicts death in medically ill patients
(10). Specifically, this study shows that patients who were capable of having a psychiatric interview in the first 3 days following admission for a medical illness and had a major depressive disorder were more likely to die in the hospital independent of the severity of their nonpsychiatric medical illness. This finding may be applicable to other groups of patients whose medical comorbidity is similar to that of the patients in our study group.
The diagnosis of major depressive disorder based on DSM-IV criteria modified for use in the medically ill, as described by one of us (S.V.A.C.)
(13), was more likely to predict death than a diagnosis of major depressive disorder based on DSM-IV criteria that included all symptoms regardless of etiology. Of the patients with a modified diagnosis of major depressive disorder, 46.7% (seven of 15 patients) died, compared with 29.2% (seven of 24 patients) of those with an inclusive diagnosis. After controlling for the severity of illness, we found that the mortality odds ratio for patients with a modified diagnosis of major depressive disorder was 15.5, compared with 5.8 for those with an inclusive diagnosis of major depressive disorder. Of the 24 patients classified as having major depressive disorder by the inclusive criteria, 13 were classified as having major depressive disorder and 11 were classified as having minor depression by the modified criteria. None of those diagnosed as having major depressive disorder according to the inclusive criteria and were reclassified as having minor depression according to the modified criteria died, further confirming the predictive power of the modified criteria for major depressive disorder to predict death.
This study found that minor depression did not predict in-hospital death, either with or without controlling for severity of illness. Although some investigators
(4,
7) have shown no relationship between subsyndromal depression and death, others
(2,
3,
8,
9) have. Studies that have shown this association have had larger study groups
(8,
9), used morbidity as well as mortality as an outcome measure
(2,
3), and/or have had extended follow-up beyond hospital stay
(2,
9). Certain disease categories, such as cardiovascular disease
(2,
3), may be more likely to show this relationship, although we did not find this to be true in our study group.
The base rates of major and minor depressive disorders, regardless of whether an inclusive or modified diagnostic system was used, are similar to the rates reported in other nonpsychiatrically hospitalized patients
(9,
24). It is important to note that the educational level of our study group was low, which might limit generalizability to more educated groups. Of course, we can offer no conclusions about the 108 patients (27.6%) who were gravely ill, demented, or delirious and could not be interviewed, the 28 (7.1%) who were discharged before they could be interviewed, and the 15 (3.8%) who refused to participate in the study or were taking antidepressants.
Because our study group is Brazilian, the forces of managed care, which often determine the number of days a patient can stay in the hospital in the United States, are not relevant. Patients generally entered the hospital when they were ill and either left the hospital improved or died in the hospital. The generalization of these data to U.S. hospitals is uncertain because U.S. hospitals use more technology, may require a higher illness burden for admission, and may require less improvement before discharge.
Particularly intriguing is the finding of a relationship between a history of depression (major depressive disorder or dysthymia) and prediction of death in the hospital, which was independent of a current diagnosis of major depressive disorder and severity of illness. The odds ratio for a past history of major depressive disorder or dysthymia was 7.8 after controlling for severity of illness. Whether the depression preceded or was subsequent to the illness did not predict death. Despite the care that is taken in part II of the SADS in establishing a past psychiatric history, using retrospective recall to determine past history of major depressive disorder, dysthymia, primary depression, and secondary depression is a limitation of this study.
There have been studies that examined the possible mechanisms of depression leading to higher rates of morbidity and death, particularly in cardiovascular disease
(25). Further research needs to examine why patients with a history of depression are more likely to die and why a past history of depression plus a current diagnosis of major depressive disorder further increases a patient’s risk of death.
Our final multivariate logistic regression model showed that the following variables independently predicted death: severity of illness (odds ratio=1.6 for each unit increase in the Charlson combined age-comorbidity index), current modified diagnosis of major depressive disorder (odds ratio=7.4), and a history of depression, major depressive disorder, or dysthymia (odds ratio=4.4).
Few studies have addressed the issue of treatment of depression in the medically ill and outcome. One group
(4) showed that treatment with antidepressants did not alter outcome but that patients who recovered from depression had an intermediate risk of death compared with patients who were never depressed (who had the lowest risk) and those whose depression did not remit (who had the highest risk). A number of investigators are currently studying the type of treatment that best results in remission of depression in different disease categories and how this affects morbidity and mortality. Although the data from this study do not show that treatment of depression in the hospitalized medically ill alters mortality, until more data are available, it seems reasonable for the clinician treating physical illness to recognize and aggressively treat serious depression as well. Particular attention should be paid to depressed patients who have a past history of dysthymia or major depressive disorder.