Brain Volume Measures
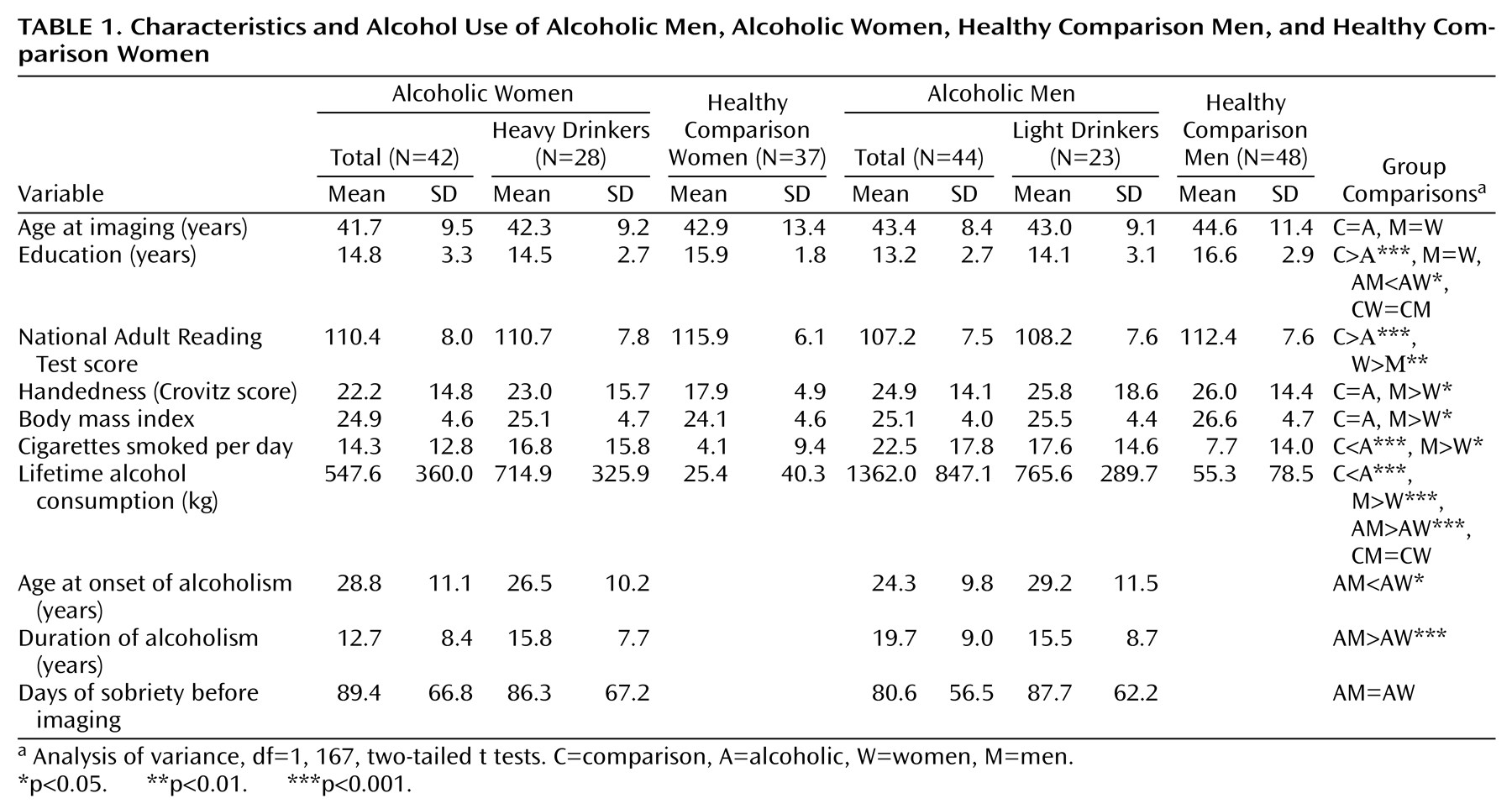
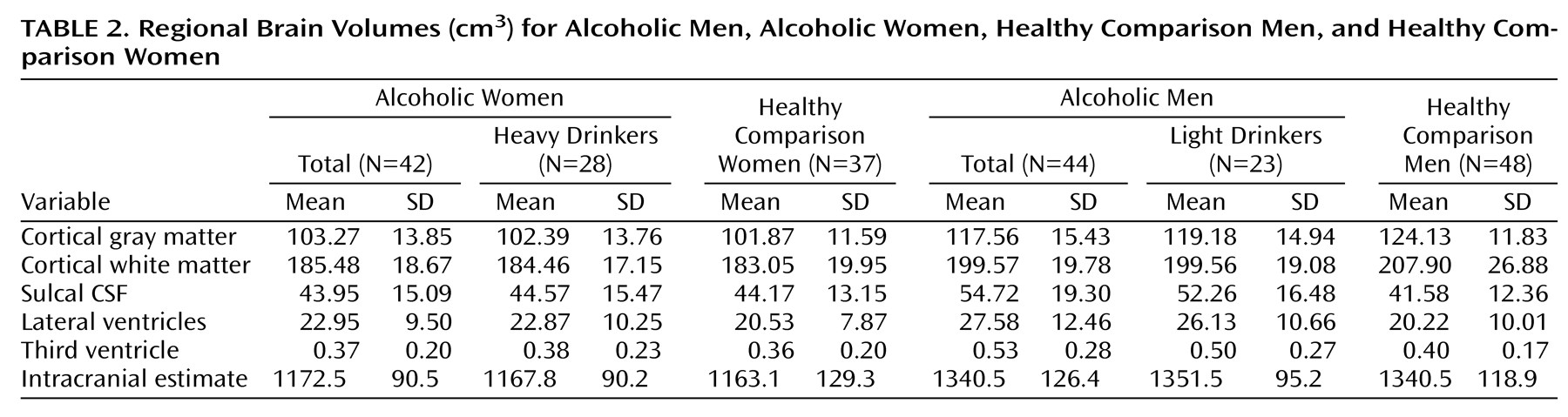
Mean regional brain volumes for each group, expressed in cubic centimeters, are presented in
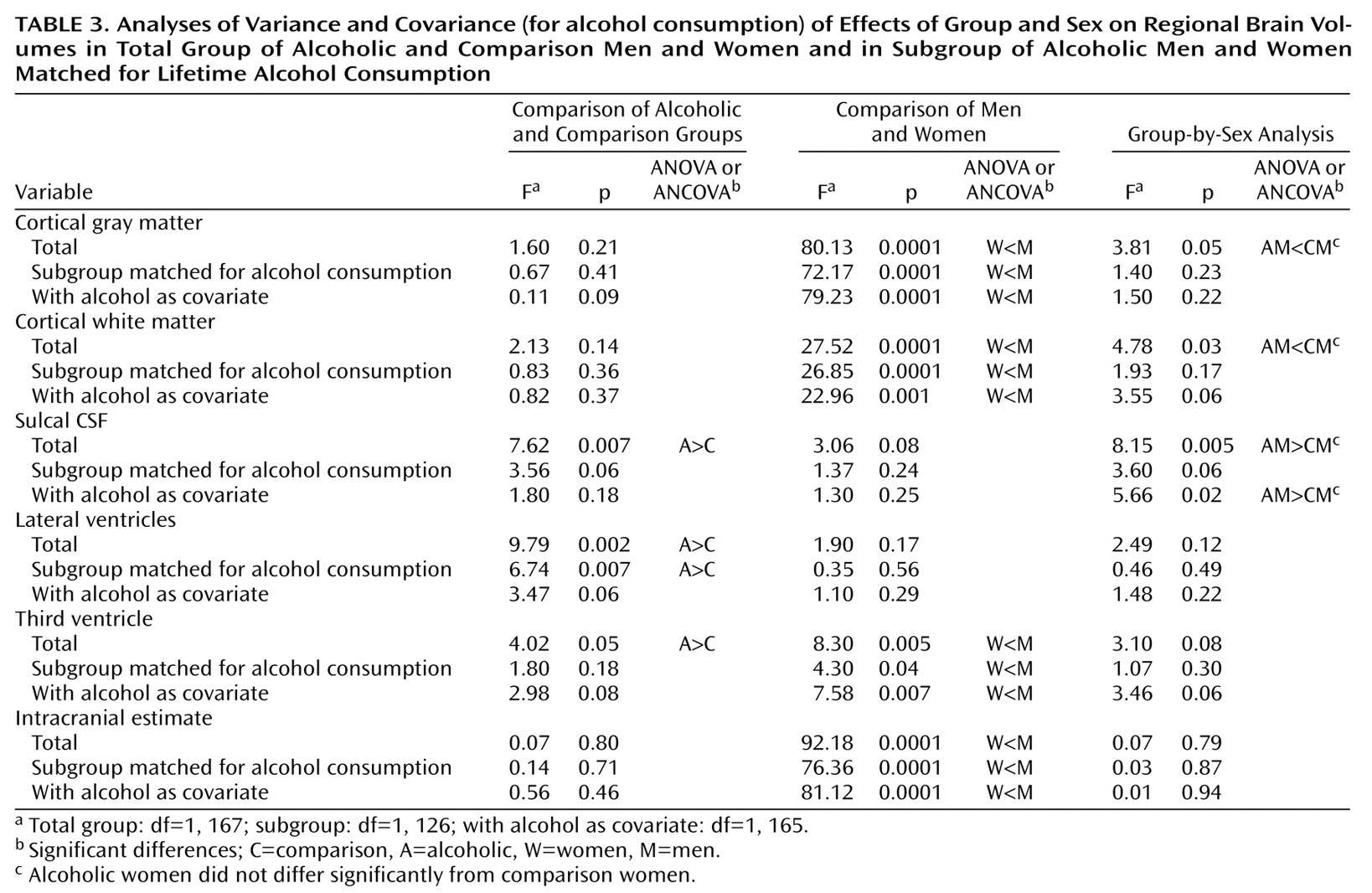
Table 2. ANOVAs for the total groups and subgroups and ANCOVAs, covarying for alcohol consumption, for the total groups are presented in
Table 3.
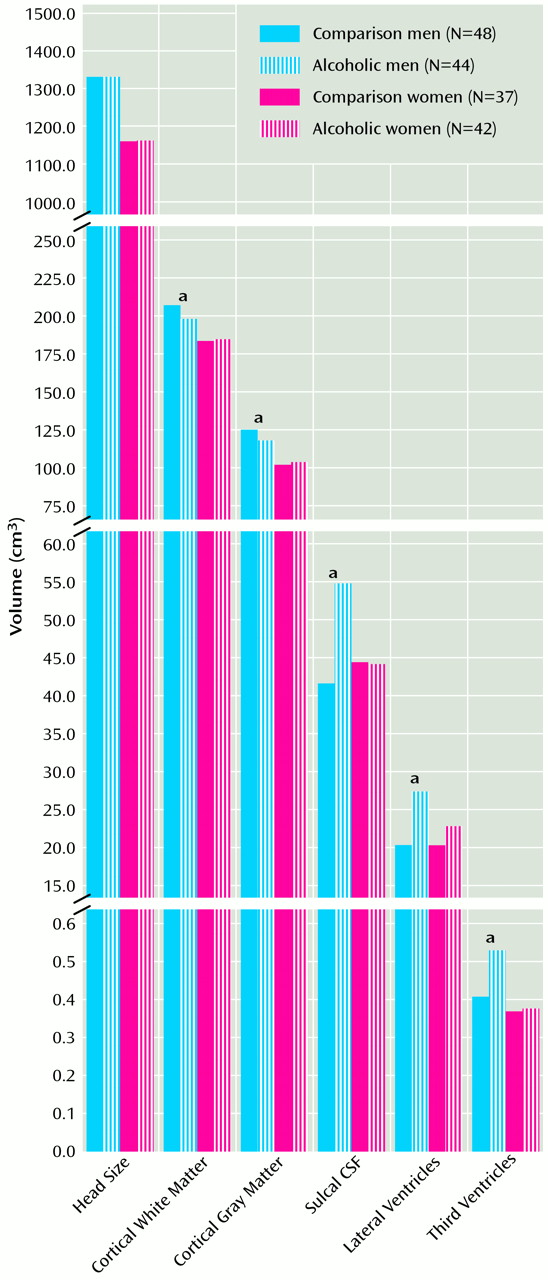
Figure 1 plots values for each group’s regional brain volume measures. As expected, intracranial volume was larger in men than in women. This sex effect was also seen in cortical gray and white matter and in third ventricular volume but did not reach significance for cortical sulcal and lateral ventricular volumes.
The alcoholics had larger volumes of cortical sulci and lateral and third ventricles than the healthy comparison subjects. These differences remained significant for the lateral ventricles, even after covarying for alcohol consumption or within the alcohol-matched restricted groups with lower mean alcohol consumption. The group effects at the cortical sulci and third ventricles were nonsignificant when we compared the smaller alcohol-matched groups or covaried for alcohol consumption.
ANOVA interactions were significant for cortical white matter, gray matter, and cortical sulci. Follow-up two-tailed t tests revealed that alcoholic men showed deficits relative to healthy comparison men, but alcoholic women were not significantly different from healthy comparison women. After statistically covarying for alcohol consumption, the interactions for the sulci remained significant, while those for white matter and the third ventricle volumes approached significance. In the alcohol-matched restricted groups, only the cortical sulci interactions approached significance.
Regression analysis across data for all men, irrespective of diagnosis, found age to be a significant predictor of cortical gray matter (r=0.42, p<0.0001), cortical sulcal (r=0.45, p<0.0001), lateral ventricular (r=0.44, p<0.0001), and third ventricular (r=0.52, p<0.0001) volumes but not cortical white matter volumes (r=0.05, p=0.66). Age was also a significant predictor of cortical gray matter (r=0.46, p<0.0001), sulcal (r=0.47, p<0.0001), lateral ventricular (r=0.33, p<0.003), and third ventricular (r=0.55, p<0.0001) volumes but not cortical white matter volumes (r=0.07, p=0.53) across all women, irrespective of diagnosis.
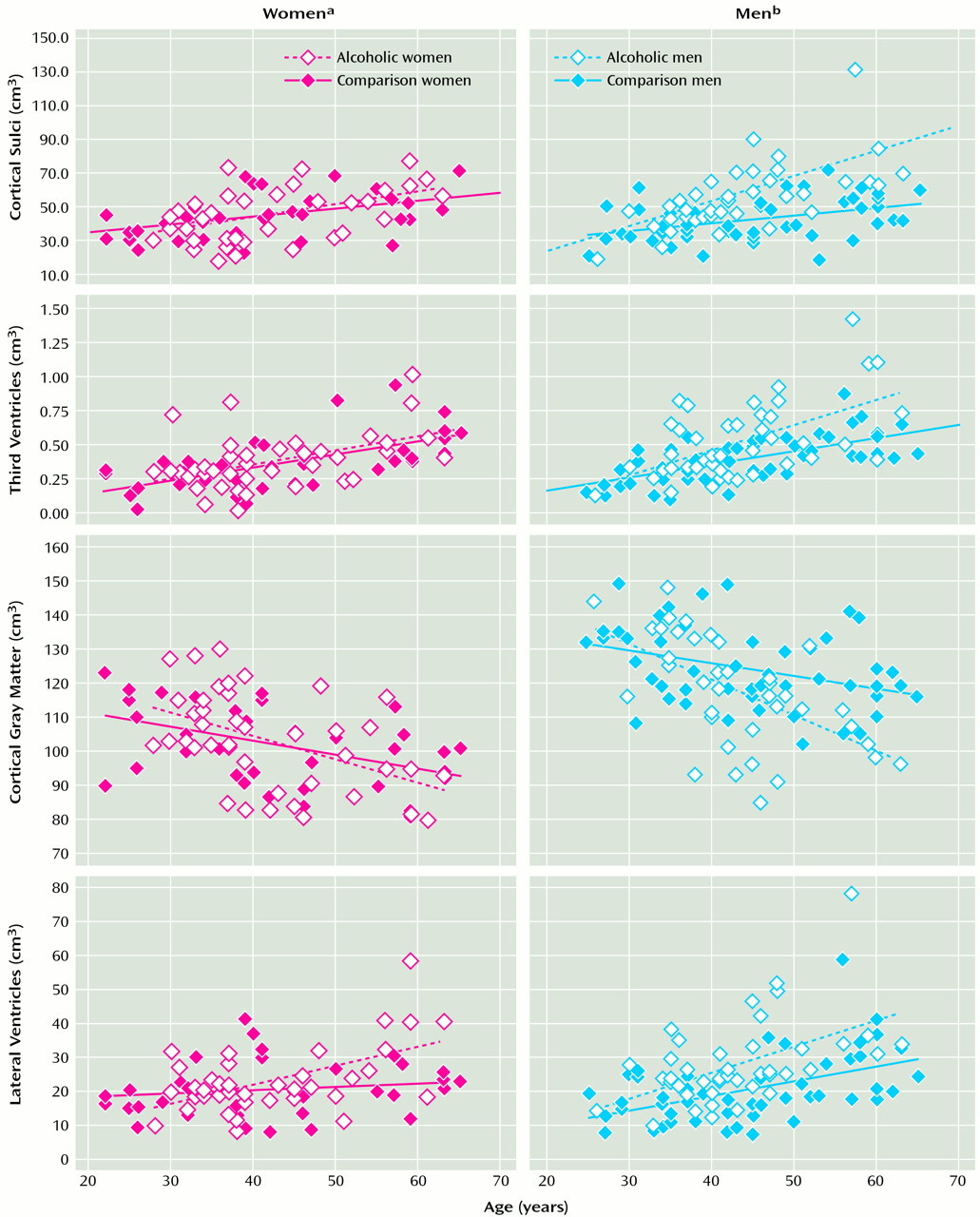
Figure 2 plots values for regional brain volume measures against age, separately for men and women and within each sex group for alcoholic and healthy comparison subjects. The slopes relating regional brain volume measures to age were significantly steeper in alcoholic than healthy comparison men for cortical gray matter, sulcal, and third ventricular volumes but not lateral ventricular volumes. In women, the slopes relating regional brain measures to age were significantly steeper in alcoholic than healthy comparison women for lateral ventricular volumes.
For the alcoholic men, lifetime alcohol consumption added to age in a multiple regression provided no additional predictive value to any of the brain variables measured, nor did length of sobriety before the imaging. The same pattern of results was found for the alcoholic women, with one exception: longer recent sobriety predicted greater cortical white matter volumes (partial F=8.62, df=2, 39, p<0.006) after we controlled for age.
A prior analysis of cortical gray matter volumes in men with alcoholism
(8) found that alcoholics age 45 and older have a selectively more severe deficit in prefrontal gray matter than younger alcoholics. Repeated measures ANOVAs for the six cortical gray matter regions of interest were performed separately for men and women. For men, diagnosis (F=5.87, df=1, 90, p=0.02) and the repeated measure for region of interest (F=1927.66, df=5, 450, p<0.0001) were both significant, as was the interaction of the two (F=4.25, df=5, 450, p<0.001). For women, the repeated measure for region of interest was significant (F=1284.82, df=5, 385, p<0.0001), but neither diagnosis (F=0.26, df=1, 77, p=0.61) nor the interaction of the two (F=0.41, df=5, 385, p<0.84) was significant. When this analysis was repeated only for women over the age of 45, the pattern of results was the same.
One limitation of this study was that the alcoholic and healthy comparison subjects were not well matched on education or tobacco use. Correction for educational differences is complex because, in addition to significant differences in levels of education between diagnostic groups, there was a diagnosis-by-sex interaction in which the alcoholic men had significantly less education than the healthy male comparison subjects (t=5.84, df=90, p<0.0001), whereas the alcoholic women were not significantly different from the healthy comparison women (t=1.75, df=77, p=0.09) regarding education. Furthermore, education-by-brain volume interaction slopes differed by diagnosis for cortical gray and white matter volumes, precluding valid ANCOVA correction over the total groups. Therefore, to determine if educational difference could account for the deficits, ANCOVAs were applied only to the men for whom brain volume deficits were found. This analysis showed that diagnosis remained a significant predictor of sulcal CSF (F=19.57, df=1, 89, p=0.0001), gray matter (F=3.56, df=1, 89, p=0.06), lateral ventricular (F=21.07, df=1, 89, p=0.0001), and third ventricular (F=12.37, df=1, 89, p=0.0007) volumes after control for educational differences. Cortical white matter volume was excluded from this ANCOVA, as it was related differently to education in alcoholic (r=0.18, df=1, 43, p=0.24) and healthy comparison (r=0.55, df=1, 47, p<0.001) men.