Electroencephalography was introduced by Hans Berger of Jena, Germany, in 1929, primarily to study brain dysfunction in mental illnesses
(1). The initial hope that it would either lead to specific knowledge of cerebral pathophysiology or support differential diagnosis in idiopathic major mental illnesses has long been abandoned. Nevertheless, it continues to have value in the diagnosis of epilepsy, brain damage, delirium, and dementia and in differentiating brain disease from primary psychiatric disorders
(2,
3). Electroencephalographic (EEG) abnormalities occur in patients with various idiopathic psychiatric disorders. In studies antedating widespread use of modern atypical antipsychotic agents, about 30% of hospitalized psychotic patients had EEG abnormalities over the temporal lobes
(4), with epileptiform EEG abnormalities in about 2.6% of cases
(5). EEG abnormalities also have been found in manic patients
(6).
Relative contributions of primary brain dysfunction and effects of medicinal treatments to these EEG findings largely remain uncertain. Many psychotropic drugs can alter EEG activity
(1–
8). Older neuroleptics commonly produce excessive diffuse, slow-wave EEG activity or increased alpha rhythm without obvious clinical manifestations
(9,
10). Low-potency neuroleptics can also induce clusters of slow dysrhythmic waves, sharp waves, or spike and slow-wave responses that may anticipate overt epileptic seizures
(11). EEG abnormalities associated with recently introduced antipsychotic-antimanic drugs have been minimally studied. Clozapine has an unusually high impact on EEG activity and has induced a variety of types of epileptic seizures
(12), dose dependently, in about 10% of patients exposed to a range of clozapine doses (25–900 mg/day) for up to 3.8 years
(13). Rates of EEG abnormalities during treatment with newer atypical antipsychotics have been much less well evaluated
(7).
Given the limited knowledge of EEG abnormalities among patients treated with modern antipsychotics, we undertook an extensive retrospective analysis of EEG recordings of 293 psychiatric inpatients treated with various antipsychotic agents as well as those of 30 whose treatment did not include these agents. We also considered associations of EEG findings with selected clinical and treatment factors. We hypothesized that EEG abnormalities would be associated mainly with atypical antipsychotics of low potency and would increase with drug dose.
Method
Subjects
Medical records of 2,812 psychiatric patients admitted to McLean Hospital between January 1992 and February 1999 who underwent electroencephalography as inpatients were reviewed. Criteria leading to exclusion of 2,489 (88.5%) of the patients screened were age <14 years, epilepsy, cerebral tumor, stroke, traumatic brain injury without full recovery, clinical or brain scan evidence of focal brain lesions, current delirium, Down’s syndrome, current migraine headaches, history of multiple sclerosis, positive HIV test, any instance of loss of consciousness that exceeded 5 minutes, prior drug overdose leading to coma, WAIS IQ <70, prior EEG abnormalities, alcohol and drug abuse or withdrawal within 10 days of the EEG recording, current anticonvulsant treatment (including use of anticonvulsants as mood stabilizers), or receiving ECT within the previous 4 months.
Of the remaining subjects entered into the study, 293 were receiving antipsychotic treatment. Their mean age was 35.6 years (SD=15.7, range=13–82); 50.5% (N=148) were male. The other 30 patients, who passed the exclusion criteria but who were not recently or currently being treated with an antipsychotic, were selected as control subjects. The mean age of this group was 33.3 years (SD=18.0, range=15–69); 43.3% (N=13) were male. They were required to have had no oral antipsychotic treatment for at least 5 days and no long-acting injected neuroleptic for at least 2 weeks (if given fluphenazine) or 4 weeks (if given haloperidol) before their EEG recording. Psychiatric diagnoses (according to DSM-IV) among subjects treated and not treated with antipsychotics included schizophrenia/schizoaffective disorder (41.3% [N=121] and 23.3% [N=7], respectively), bipolar disorder (26.6% [N=78] and 23.3% [N=7]), and major depression (17.7% [N=52] and 13.3% [N=4]) along with a miscellaneous category of “other” diagnoses (14.7% [N=43] and 40.0% [N=12]).
Data collected from medical records included sex, age, and handedness; discharge psychiatric and substance abuse diagnoses (updated to meet DSM-IV criteria by consensus); comorbid medical and neurological diagnoses; antipsychotic type, current dose, and duration of use before EEG recording; type and dose of other drugs used at the time of the EEG recording; length of hospitalization; and treatment response as recorded in discharge summaries. Antipsychotic drug doses (mg/day) were converted to chlorpromazine equivalents and corrected (mg/kg) for body weight
(8,
14).
Antipsychotic Treatment
Treatment was categorized by agents used at the time of the EEG recording. Subjects exposed to more than one antipsychotic (N=24) were assigned to a combination treatment category. Typical neuroleptics were categorized as high potency (e.g., fluphenazine, haloperidol, loxapine, perphenazine, pimozide, thiothixene, trifluoperazine) or low potency (e.g., chlorpromazine, mesoridazine, molindone, thioridazine) on the basis of daily dose (i.e., ones or tens of mg/day versus hundreds). Similarly, atypical agents also were divided into drugs of high potency (risperidone) and low or moderate potency (clozapine, olanzapine, and quetiapine).
Seventeen treatment groups were formed comprising 15 individual antipsychotic agents, a combination category, and the untreated control group. Drug type subgroups were also formed to compare typical versus atypical and high- versus low-potency agents.
Outcome Measures
Principal outcome measures were a binary categorization (EEG abnormality present versus absent) and EEG abnormality severity scores within the defined treatment groups. Clinical outcome was also considered in relation to EEG abnormality status on the basis of condition at discharge rated by consensus assessment of information in the medical record and clinical discharge summary. Hospital length of stay was also employed as a surrogate index of treatment responsiveness.
EEG Assessment
EEG recordings (one per subject) were performed according to recommendations of the American Electroencephalographic Society, with a standard 10/20 placement of 21 electrode leads; bipolar and referential montages were used
(15). EEG recordings during the awake state were obtained from all antipsychotic-treated patients and control subjects; 62.1% (N=182) of the antipsychotic-treated patients and 63.3% (N=19) of the control subjects were also recorded during sleep; drowsiness was noted in the EEG recordings of 48.1% (N=141) of the antipsychotic-treated patients and 3.3% (N=1) of the control subjects. Recording during hyperventilation was obtained from 68.9% (N=202) of the antipsychotic-treated patients and 90.0% (N=27) of the control subjects. Photic stimulation was performed in 93.9% (N=275) of the antipsychotic-treated patients and 96.7% (N=29) of the control subjects. The original EEG interpretations and reports were generated by two experienced, board-certified neurologists. A senior behavioral neurologist (B.H.P.), blind to patients’ names, diagnoses, medications, and clinical outcome, reinterpreted and scored all EEG recordings to assure rating consistency. Reliability of EEG scoring was tested by blind repeated scoring of 30 randomly selected tracings assessed with the kappa statistic and intraclass correlations for blind reproducibility of actual EEG scores.
EEG activity was scored as follows: 0=no abnormality; 1=mild abnormality (generalized or frontal symmetrical theta slowing); 2=moderate abnormality (theta and delta slowing, asymmetrical focal theta or delta, generalized intermixed theta and delta activity, sharp waves or phase reversal); 3=severe abnormality (spike discharges or spike-and-wave activity, either alone or with the characteristics of moderate abnormality). Since only a minority of EEG recording occurred during drowsiness, when EEG patterns can be highly variable
(16,
17), abnormalities recorded only during drowsiness were excluded.
Explanatory Factors
Descriptive factors examined for bivariate correlation with EEG abnormality included age, sex, and handedness. Clinical factors similarly examined included primary psychiatric diagnosis, medical diagnoses, psychosis active at the time of EEG testing, comorbid substance use disorder, length of hospitalization adjusted for year of admission, and overall quality of treatment response. Treatment variables considered included use of any antipsychotic agent and the specific drug given; cotreatment with an antidepressant, benzodiazepine (either standing or as-needed doses), or lithium; mean chlorpromazine-equivalent dose (total mg/day and mg/kg body weight); and duration of treatment exposure.
Statistical Methods
Factors were organized by natural categories or those created by use of median-split continuous data to permit use of contingency tables (chi-square) to test for associations with the presence of EEG abnormalities. Continuous variables were log-transformed when necessary to improve distribution normality. Factors with suggestive associations (p≤0.05) with either presence or absence of EEG abnormalities in the preliminary analyses were then evaluated by multivariate logistic regression to identify a set of risk factors related to EEG abnormality (with partial-residual plots used to check for model fit) and to obtain odds ratios (and 95% confidence intervals [CIs]) for specific comparisons. Regression modeling with EEG score as the dependent variable was carried out by using ordinal logistic regression modeling methods. Robust methods were used to obtain standard error estimates. Interactions between factors retained in multivariate models were checked for significance. Goodness-of-fit chi-square tests were used to check for model fit. Averages are reported as means and standard deviations or with 95% CIs unless stated otherwise. Results with two-tailed p≥0.05 were considered statistically nonsignificant. Analyses employed Statview (SAS Corp., Cary, N.C.) and Stata (Stata Corp., College Station, Tex.) microcomputer programs.
Results
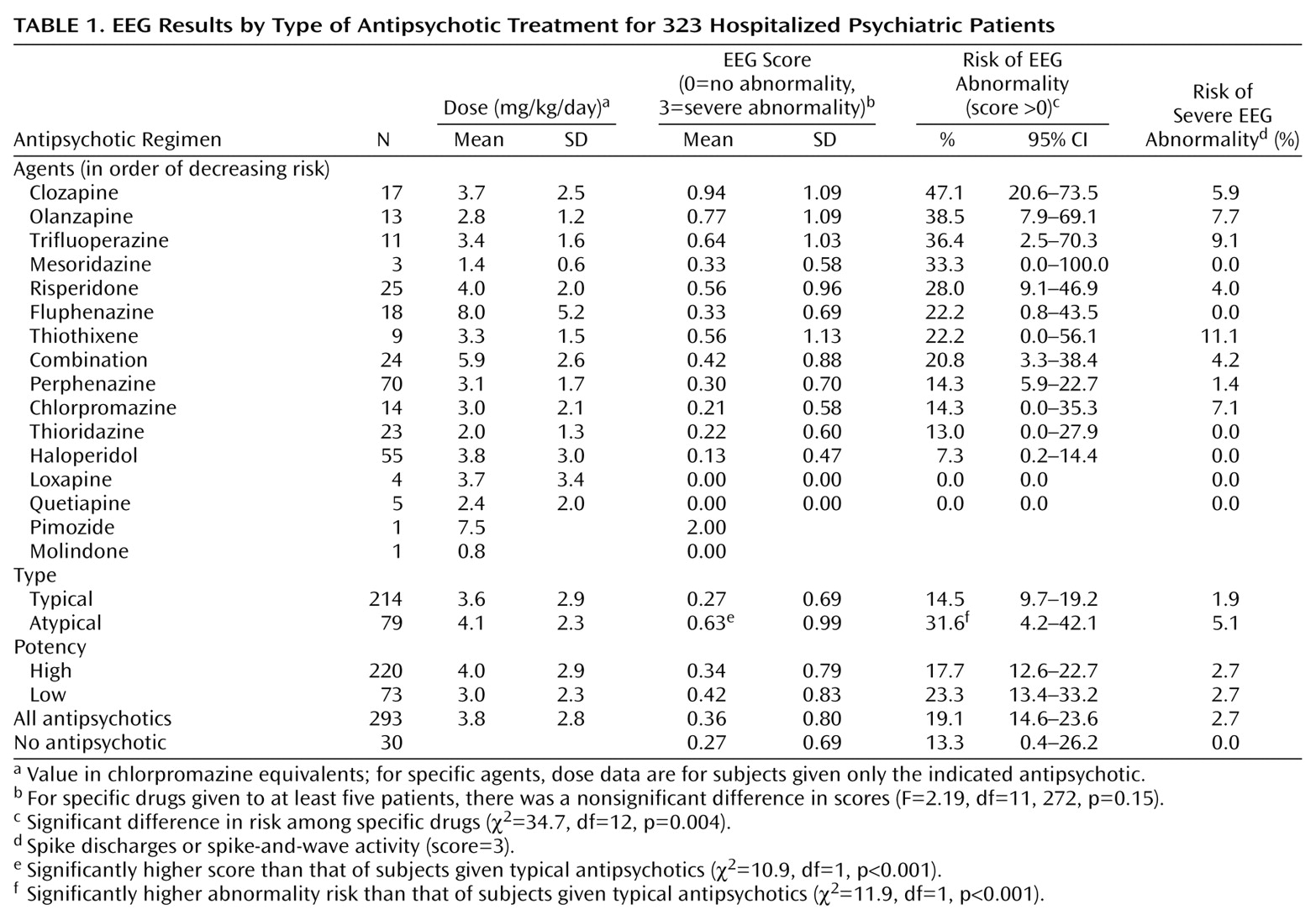
The EEG results by antipsychotic treatment type for the 323 subjects are presented in
Table 1. Four atypical agents were encountered, given alone to 60 patients and in combination with an additional antipsychotic in another 19 (N=79 total, or 27.0%; nine of the combination cases involved clozapine). Eleven different typical neuroleptics were used, given alone to 209 patients and in combination with an additional typical antipsychotic in another five. In all, 24 cases involved antipsychotic combinations: an atypical plus typical agent in 15 cases, two typical neuroleptics in five, and two atypical agents in four. Daily chlorpromazine-equivalent doses averaged 3.80 mg/kg (SD=3.02) (or 279 mg/day, SD=222), with a median of 3.10 mg/kg (or 200 mg/day), ranging from 1.40 mg/kg (mesoridazine) to 8.00 mg/kg (fluphenazine).
For the 30 tracings randomly selected for reliability measurements, ratings of normal/abnormal yielded a kappa of 0.87 (z=4.79, df=30, p<0.0001), and the EEG scores had high reproducibility (intraclass correlation coefficient [ICC]=0.94, 95% CI=0.90–0.98; F=31.9, df=1, 29, p<0.0001). EEG abnormalities (rating score >0) were found in 19.1% (N=56) of the antipsychotic-treated patients but also in 13.3% (N=4) of the hospitalized patients not treated with an antipsychotic (
Table 1). This minor overall difference in risk was not statistically significant (χ
2=0.60, df=1, p=0.44) nor was the difference in average EEG score (z=0.74, p=0.46), reflecting a wide range of outcomes among individual subjects and drugs. Mild EEG abnormalities (score=1) were found in 8.2% (N=24) of the antipsychotic-treated patients and in 10.0% (N=3) of the control subjects; moderate ratings (score=2) were found in 8.2% (N=24) and 3.3% (N=1) of those treated and not treated with antipsychotics, respectively. Severe EEG abnormalities (score=3, indicating spike discharges or spike-and-wave activity) were found in 2.7% (N=8) of the antipsychotic-treated subjects. In order of risk, severe abnormalities were associated with thiothixene, trifluoperazine, olanzapine, chlorpromazine, clozapine, combination antipsychotic therapy, risperidone, and perphenazine (
Table 1). No patient treated with quetiapine or any other agent alone received a score of 3, nor did any untreated patient (
Table 1).
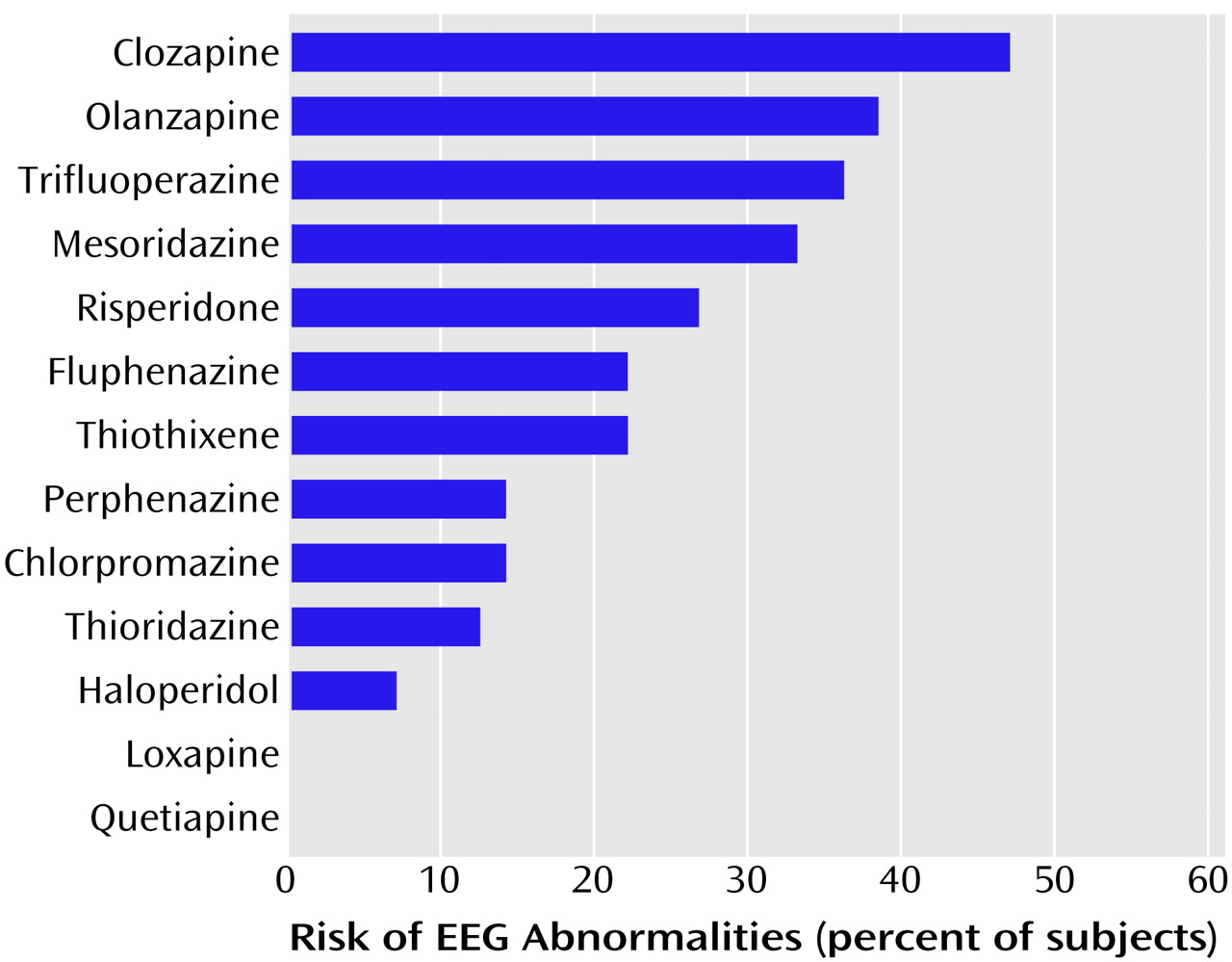
Average EEG abnormality ratings varied greatly among specific antipsychotics (
Table 1). Mean scores ranged from lows of 0.27 (SD=0.69) in the 30 antipsychotic-free subjects (and nil in small groups of five quetiapine-treated subjects, four loxapine-treated patients, and one given molindone), to a maximum of 0.94 (SD=1.09) in 17 patients given clozapine monotherapy. Rates of EEG abnormalities of any type or severity associated with specific treatments ranged from 13.3% in the untreated comparison subjects (or 0% among the few subjects given quetiapine, loxapine, or molindone) to a high of 47.1% of subjects given clozapine alone (
Figure 1). Even in combination with other antipsychotics, clozapine was associated with a high risk of EEG abnormalities (39.1% of all patients exposed to clozapine). Across all individual treatment groups, as expected, risk of EEG abnormality was strongly correlated with mean EEG scores (r=0.98, df=16, p<0.0001).
Owing mainly to the strong impact of clozapine and olanzapine, atypical antipsychotics generally, but inconsistently, carried significantly greater EEG abnormality risk than typical neuroleptics (31.6% versus 14.5%). By ordinal logistic regression modeling, atypical antipsychotics as a group were found to have significantly higher frequencies of EEG abnormalities than typical neuroleptics at each step of the four-level EEG abnormality rating scores; EEG scores for atypical versus typical antipsychotics averaged 0.63 (SD=0.99) versus 0.27 (SD=0.69), respectively (z=3.35, p<0.001). The typical neuroleptics yielded results similar to those seen in the antipsychotic-free subjects for mean EEG scores (0.27 and 0.27) and risks of EEG abnormalities (14.5% and 13.3%, respectively) (
Table 1). Among antipsychotics considered atypical, differences in EEG abnormality risk among clozapine (47.1%), olanzapine (38.5%), and risperidone (28.0%) were not statistically significant (data not shown), and quetiapine (0% risk) was used in only five cases (
Table 1). Evidence of severe EEG abnormality (spikes or spike-and-wave activity) was found in eight of 293 patients (2.7%) at a nonsignificantly higher rate among those given an atypical antipsychotic (5.1% [N=4 of 79] versus 1.9% [N=4 of 214] of those given a typical antipsychotic) (p=0.22, Fisher’s exact test). Antipsychotic drugs of low versus high potency did not differ significantly in risk of EEG abnormalities (23.3% versus 17.7%, respectively; χ
2=2.43, df=1, p=0.12) nor in EEG score (0.42 versus 0.34; z=–0.30, p=0.76).
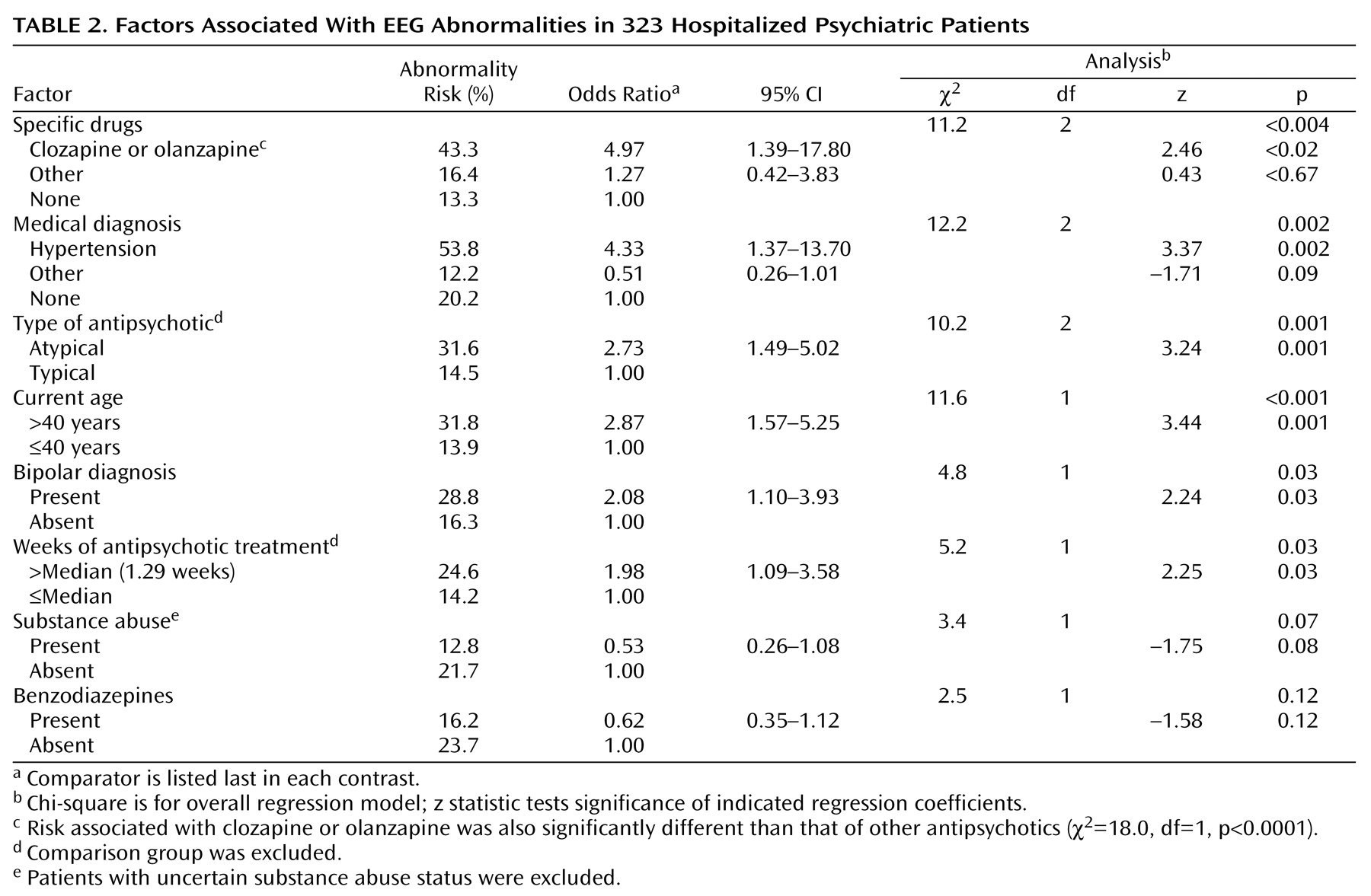
Few demographic, diagnostic, and treatment factors were significantly associated with EEG abnormalities in preliminary categorical comparisons based on binary EEG status (normal versus abnormal). In descending order of significance, the following were associated with EEG abnormalities: 1) use of clozapine or olanzapine versus all other antipsychotics, 2) presence of hypertension (diastolic pressure >90 mm Hg) versus no medical comorbidity, 3) atypical versus typical antipsychotics overall, 4) current age >40 years (median age) versus younger, 5) diagnosis of bipolar disorder versus all others, 6) longer exposure to antipsychotic drug (i.e., >1.29 weeks), and 7) paradoxically, the absence versus presence of a comorbid DSM-IV substance use disorder (
Table 2). In addition, use of a benzodiazepine tended toward an expected
lower risk of EEG abnormality (
Table 2). There was no relationship between daily dose and EEG abnormalities (e.g., for all antipsychotic-treated patients, mean daily doses for those with abnormal and normal EEG recordings were 3.51 mg/kg [SD=2.27] and 3.82 mg/kg [SD=2.92], respectively; F=0.57, df=1, 292, p=0.55).
We found no correlation between the presence or severity of EEG abnormalities and clinical outcome by the time of hospital discharge. First, there was little difference in likelihood of treatment response being rated (blind to EEG status) as favorable between patients with (86.7%) and without (80.3%) EEG abnormalities (χ2=1.31, df=1, p=0.25). Length of hospital stay (adjusted for admission year) also did not differ between patients with normal versus abnormal EEG recordings (mean=27.6 days [SD=21.8] and 23.8 days [SD=17.7], respectively; F=0.81, df=1, 315, p=0.37).
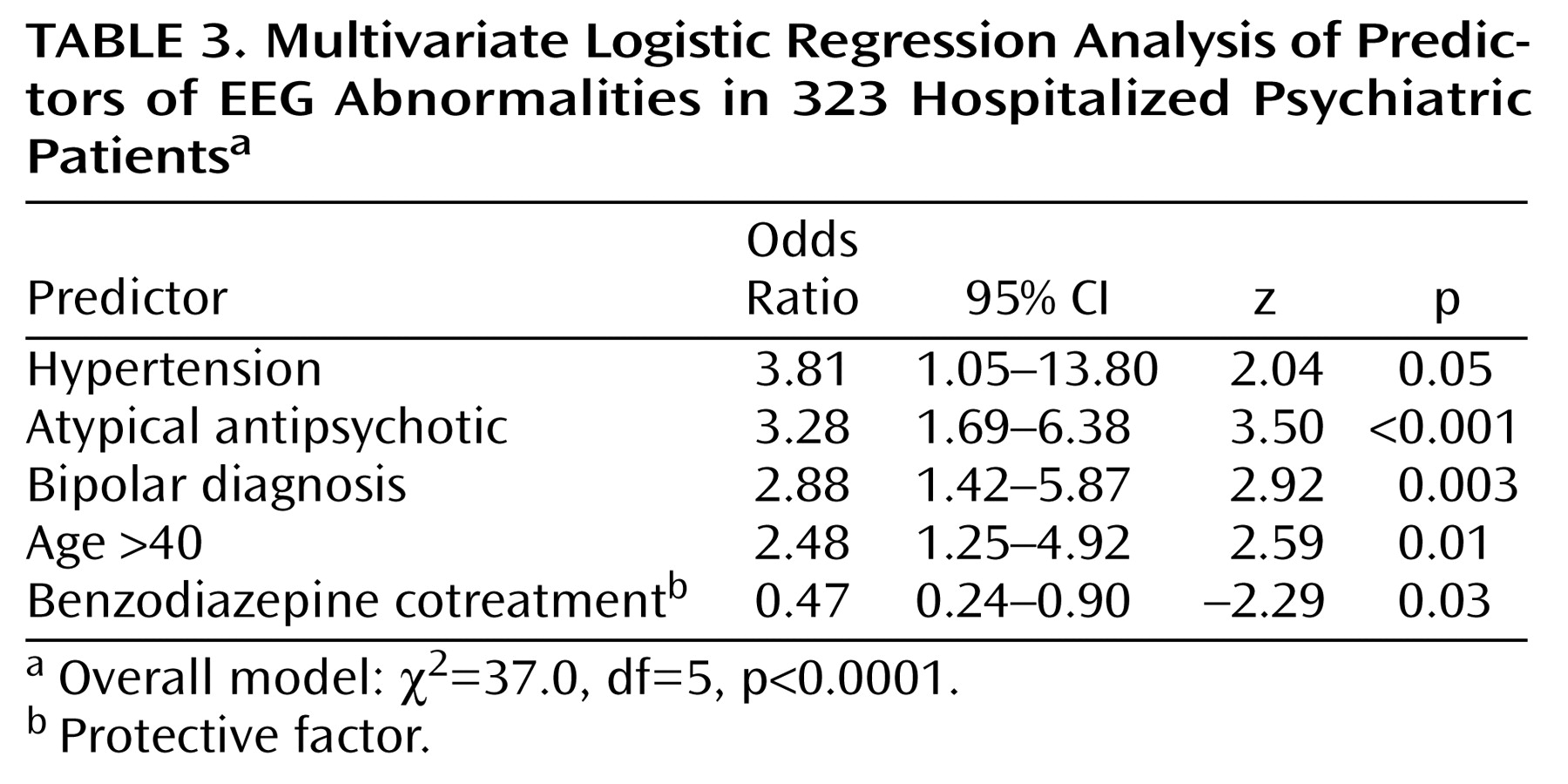
Factors associated with EEG abnormalities in bivariate comparisons (
Table 2) were examined further by multivariate logistic regression modeling, which found that five factors remained significantly associated with EEG abnormalities. In rank order of their odds ratios, these were 1) presence of hypertension, 2) use of an atypical antipsychotic agent, 3) diagnosis of bipolar disorder, 4) age over 40, and 5) absence of cotreatment with a benzodiazepine (
Table 3). The overall multivariate regression model based on these factors was strong (χ
2=35.0, df=5, p<0.0001). The risk factors, with the EEG-protective effects of benzodiazepine cotreatment excluded, also showed cumulative effects leading to increasing probability of EEG abnormality: 2.9% (95% CI=0.0–6.2) with no risk factor present, 24.5% (95% CI=17.2–31.7) with one factor, 34.2% (95% CI=16.6–48.3) with two, and 50.0% (95% CI=20.0–79.9) with three considered. No subject had more than three of the five factors, and there were no significant interactions among the factors.
Discussion
EEG abnormality rates and severity scores were evaluated in 323 hospitalized psychiatric patients. Ratings were blind to treatment with a variety of antipsychotic agents as well as a no-antipsychotic treatment condition. Specific antipsychotics varied widely in their association with EEG abnormalities. Among modern atypical agents, EEG abnormality risk was highest with clozapine, followed by olanzapine and risperidone, with the few quetiapine-treated patients having no abnormalities. Abnormality rates among older neuroleptics ranged from 36.4% with trifluoperazine to 7.3% with haloperidol, with intermediate rates in other neuroleptics of high or low potency (13%–14% with chlorpromazine, perphenazine, or thioridazine) and in untreated subjects. As there is no reason to suspect that pretreatment EEG status differed systematically by drug, the marked differences encountered may be largely drug specific. Contrary to expectation, chlorpromazine-equivalent dose (either in mg/day or mg/kg) did not correlate with EEG abnormalities.
Clozapine has been especially strongly associated with higher seizure risk, and EEG abnormalities are found in at least one-third
(12,
13,
18–
25) or more
(12,
19,
20,
23) of clozapine-treated patients and in 47.1% in the present study. Seizure risk with clozapine probably increases with drug dose and serum concentration
(19,
24,
26). With newer drugs, such studies are uncommon. Risperidone has rarely been associated with severe EEG abnormalities or overt epileptic seizures
(27,
28). With olanzapine, risk of EEG abnormalities (38.5%) was higher than expected from its reported seizure risk (as low as 0.88% [
29,
30]). We found no EEG abnormalities in the five patients treated with quetiapine, which has a low reported seizure risk (0.75%) and only minor EEG effects
(31).
Clinical factors significantly associated with EEG abnormalities included hypertension and older age. EEG abnormalities are uncommon in hypertension associated with advancing age and without evidence of cerebrovascular insufficiency or neurological damage
(2). However, advancing age can increase EEG variability, with some focal temporal slowing or slowing of average alpha EEG frequencies
(2,
17).
The observed protective association between benzodiazepine cotreatment and EEG abnormalities presumably reflects the anticonvulsant effect of these agents and their tendency to suppress epileptiform activity and induce EEG slowing
(2,
3,
7). Slowing is also associated with phenothiazines and butyrophenones as well as tricyclic antidepressants, monoamine oxidase inhibitors, lithium, analgesics, and some hallucinogens
(2,
3,
32,
33). Low-potency phenothiazines can induce generalized paroxysmal bursts in the EEG recording and, occasionally, epileptic seizures
(32). EEG abnormalities are found in nearly two-thirds of patients treated with lithium, including background slowing with high-voltage anterior delta activity and a 17% risk of spike discharges
(3,
33). Recent use of lithium may contribute to the association found between EEG abnormalities and bipolar disorder.
A provocative hypothesis, based on limited data, is that EEG abnormalities may be associated with clinical improvement in psychotic patients, either during treatment
(34–
36) or as a predictive factor before use of clozapine in particular
(37). However, we found no evidence of association of EEG status and clinical improvement.
Limitations of this study include its retrospective design, with medical records and clinical EEG assessments as the primary sources of data. There was no control over when or why EEG recordings were obtained, knowledge of pretreatment EEG status, nor control of treatments given, and the numbers of subjects given some drugs were quite small. The present clinical cohort also may be enriched with patients with EEG abnormalities, although there is no reason for such risk to be differentially associated with specific treatments. Ratings of EEG abnormalities were crude but were carried out blind to treatment and with high test-retest reliability. The present study was unable to specify the clinical significance of EEG abnormalities encountered. However, even ratings of 1 (mild) can be clinically relevant: delirium can be associated with EEG slowing and other “mild” changes (score of 1). “Moderate” (score of 2) changes may suggest focal and structural lesions; “severe” changes (score of 3) may indicate seizure disorder
(3,
5,
15–
17). Nevertheless, prospective studies are required to define the clinical significance of specific types and levels of EEG abnormalities.
In conclusion, this preliminary study yielded several interesting findings. 1) Some atypical antipsychotics carry a higher average risk of EEG abnormalities than many typical neuroleptics. 2) This risk was greatest with clozapine and unexpectedly high with olanzapine. 3) Risperidone was similar to standard high-potency neuroleptics. 4) Quetiapine had a very low rate of EEG abnormality risk among the very few subjects who received this agent. 5) Neither drug potency nor daily or weight-corrected chlorpromazine-equivalent dose was associated with EEG abnormalities. 6) Other risk factors significantly and independently associated with EEG abnormalities included hypertension, older age, and diagnosis of bipolar disorder, whereas cotreatment with a benzodiazepine was a protective factor. The present findings support the view that misattribution of an EEG abnormality to an underlying brain disorder rather than to a medication effect can confuse diagnosis and complicate treatment. Finally, they encourage prospective EEG analyses before and during treatment with specific drugs and objective ratings of clinical changes.