The provision and financing of outpatient psychotherapy has long been a matter of contention and controversy. Pointed disagreements have occurred among health policy analysts, mental health professionals, third-party payers, and patients over who should receive psychotherapy, how much they should receive, and who should pay for it. However, policies governing the provision and financing of outpatient psychotherapy have developed with little access to basic information about current patterns of psychotherapy utilization
(1,
2). One reason that so little is known about patterns of psychotherapy use is that most large community mental health surveys do not distinguish psychotherapy from other outpatient mental health services. For example, neither the Epidemiologic Catchment Area study
(3) nor the National Comorbidity Survey
(4) identified whether psychotherapy was provided during outpatient psychiatric visits, nor did they provide an opportunity to assess changes in psychotherapy use over time.
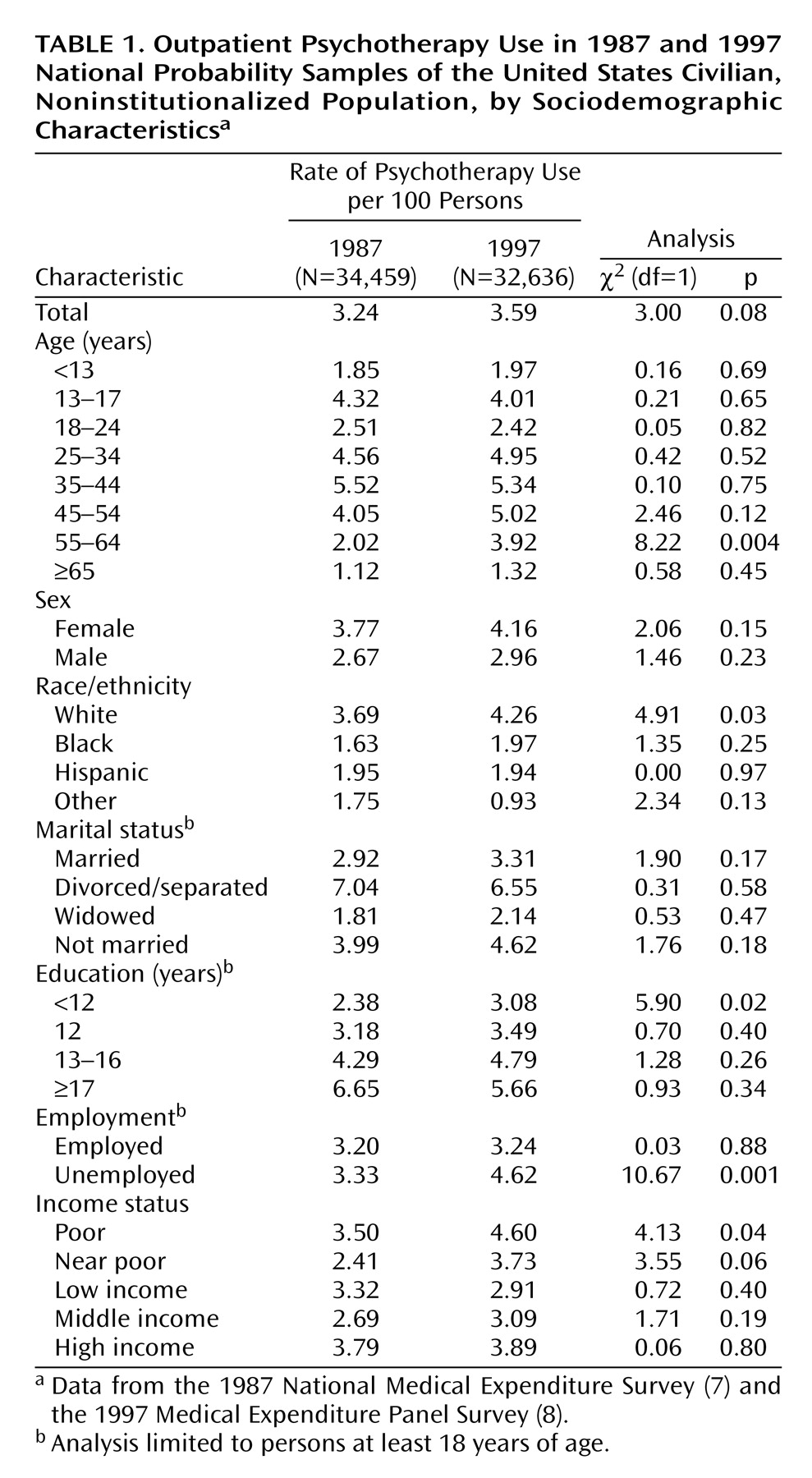
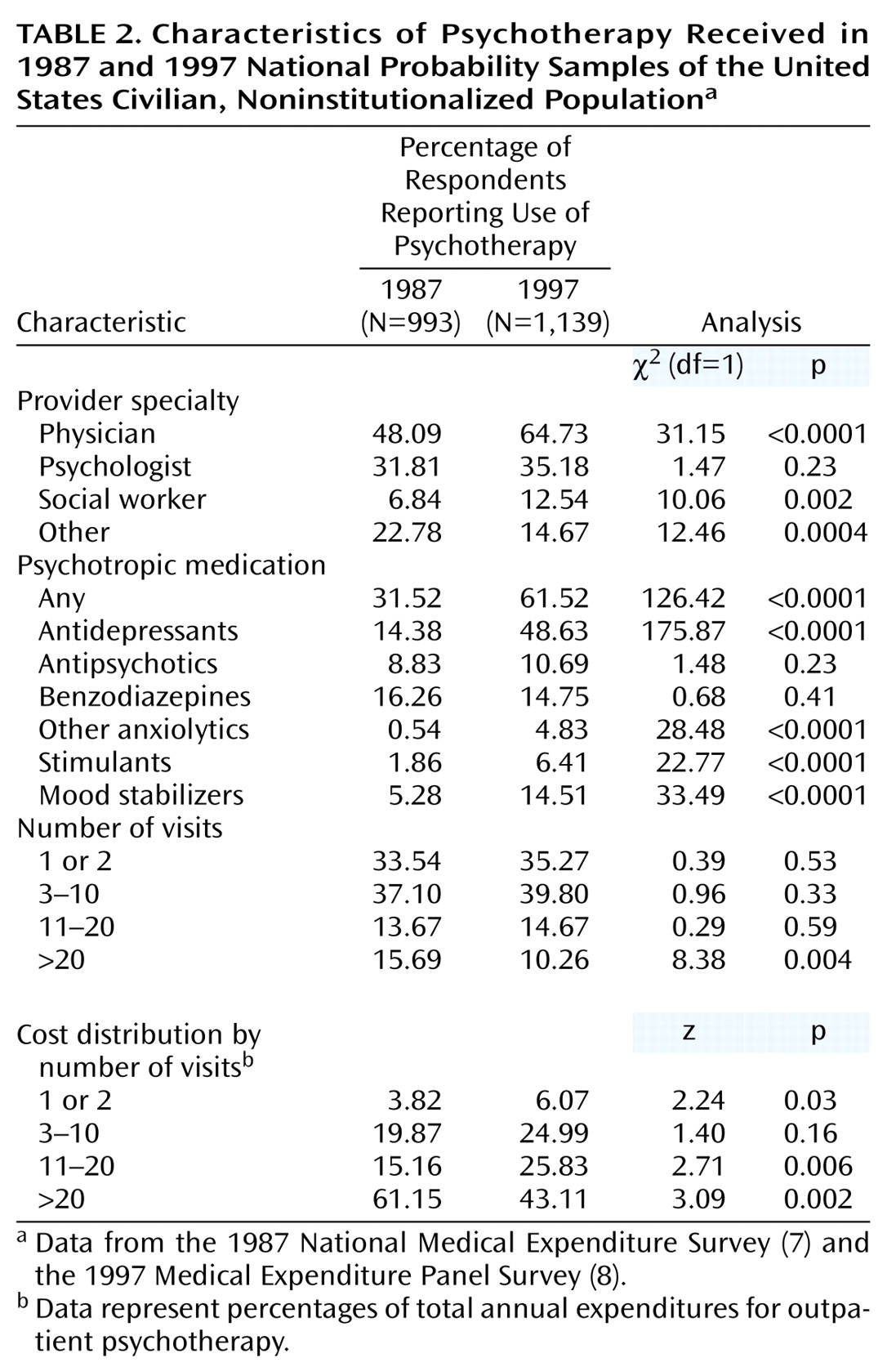
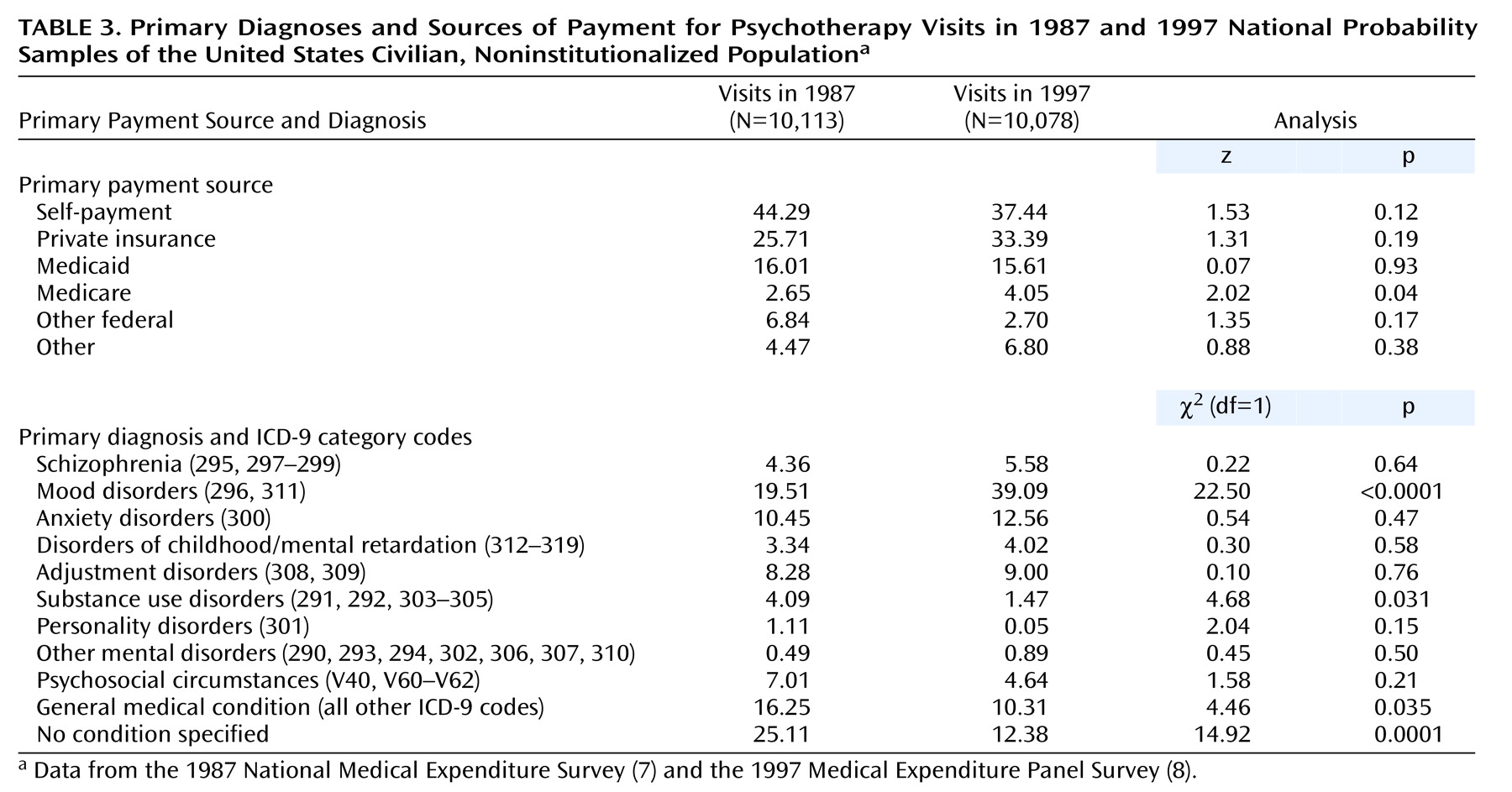
In this report, we examine recent national trends in the utilization and financing of outpatient psychotherapy using two large nationally representative surveys. We consider changes in who provided, received, and paid for outpatient psychotherapy in the United States during the period from 1987 to 1997. We also present national estimates of trends in access to outpatient psychotherapy and examine patterns of costs, reasons for use of psychotherapy, professional specialties of psychotherapists, and concurrent treatment with psychotropic medication for psychotherapy users.
Method
Data were drawn from the household component of the 1987 National Medical Expenditure Survey
(7) and the 1997 Medical Expenditure Panel Survey
(8). Both surveys were sponsored by the Agency for Healthcare Research and Quality to provide national estimates of the use of, expenditures for, and financing of health care services. The National Medical Expenditure Survey and the Medical Expenditure Panel Survey were conducted with national probability samples of the U.S. civilian, noninstitutionalized population and were designed to provide nationally representative estimates to be compared over time.
Study Samples
The 1987 National Medical Expenditure Survey used a sampling design in which 15,590 households were selected from within 165 geographic regions across the United States. A sample of 34,459 individuals was included in the study, representing a response rate of 80.1%. Respondents for the 1997 Medical Expenditure Panel Survey household component were drawn from a nationally representative subsample of the 1995 National Health Interview Survey sample, which was selected by using a sampling design similar to that of the 1987 National Medical Expenditure Survey. A total of 32,636 participants from 14,147 households were interviewed, representing a 74.1% response rate. For both surveys, a designated informant was queried about all related persons who lived in the household.
The Agency for Healthcare Research and Quality devised weights to adjust for the complex survey design and yield unbiased national estimates. The sampling weights also adjusted for nonresponse and poststratification to population totals based on U.S. census data. More complete discussions of the design, sampling, and adjustment methods are presented elsewhere
(9,
10).
Survey Structure
Households selected for the National Medical Expenditure Survey were interviewed four times to obtain health care utilization information for the 1987 calendar year. The Medical Expenditure Panel Survey included a series of three in-person interviews for 1997. In both surveys, respondents were asked to record medical events as they occurred in a calendar/diary that was reviewed during each in-person interview. Selected survey participants provided written permission to contact medical providers mentioned during the interview to verify service use, charges, and sources and amounts of payment.
Psychotherapy
The National Medical Expenditure Survey and the Medical Expenditure Panel Survey used a flash card with various response categories to ask respondents the type of care provided during each outpatient visit. Visits that included psychotherapy or mental health counseling were considered “psychotherapy” visits.
Psychotropic Medications
The National Medical Expenditure Survey and Medical Expenditure Panel Survey asked for a description of each prescribed medicine bought or otherwise obtained by survey participants during the survey year. We focused on prescribed psychotropic medications used by persons who had one or more psychotherapy visits during the survey year. Psychotropic medications were grouped by using the following American Hospital Formulary System therapeutic classes: antidepressants, antipsychotics, benzodiazepines, other anxiolytics, stimulants, and mood stabilizers
(11).
Providers
The Medical Expenditure Panel Survey and National Medical Expenditure Survey solicited information on the type of health care professionals who provided treatment at each visit. We classified providers of psychotherapy into the following groups: physicians of all specialties (a breakdown by physician specialty was not available for 1997), social workers, psychologists, and a residual group of other providers that included nurses, nurse practitioners, physician assistants, chiropractors, and other health care providers. A psychotherapy user was considered to have been treated by a provider group if the user reported making one or more visits to that group during the survey year. Some respondents used psychotherapy from more than one provider group.
Diagnosis
The surveys collected information from the respondents on the primary reason for each ambulatory care visit. This information was grouped to permit classification according to ICD-9 categories by professional coders. The interviewers each underwent 80 hours of training, and coders all had degrees in nursing or medical record administration. A total of 5% of records were rechecked for errors; error rates in these rechecks were less than 2.5%. A staff psychiatric nurse determined mental disorder diagnoses in cases of diagnostic ambiguity or uncertainty.
The ICD-9 diagnoses associated with the psychotherapy visits were grouped into ten categories: schizophrenia and related disorders (ICD-9 codes 295, 297–299), mood disorders (296, 311), anxiety disorders (300), childhood disorders/mental retardation (312–319), adjustment disorders (308, 309), substance use disorders (291, 292, 303–305), personality disorders (301), other mental disorders (290, 293, 294, 302, 306, 307, 310), psychosocial circumstances (V40, V60–V62), and general medical conditions (all other codes). A separate category was constructed for visits in which the diagnosis was not specified. Patients who received one or more psychotherapy visits for the treatment of schizophrenia, affective psychoses, paranoid states, or other nonorganic psychoses (ICD-9 codes 295–299) were considered to have received treatment for a severe mental disorder
(12).
Source of Payment
The survey interviewers asked respondents their sources of payment for each outpatient psychotherapy visit. From these data, summary variables of the following six potentially overlapping groups were constructed: self-payment, private insurance, Medicaid, Medicare, other Federal programs, and a residual group of other sources.
Analysis Plan
Rates of psychotherapy use per 100 persons for each survey year were computed overall and stratified by key sociodemographic characteristics. Psychotherapy use was compared over time by provider specialty, concomitant psychotropic medication use, number of annual visits, and costs. In addition, trends in payment source and primary diagnosis for the psychotherapy visit were examined.
To adjust for changes in patient characteristics over time, we used a logistic regression model to evaluate the strength of the association between survey year and use of psychotherapy while controlling for the effects of background sociodemographic characteristics.
All statistical analyses were performed with the SUDAAN software package
(13) to accommodate the complex sample design and the weighting of observations. Z tests were used to evaluate the statistical significance of changes in proportional cost distributions. The Wald chi-square test was used for all other comparisons. All tests were two-tailed, and alpha was set conservatively at 0.01 to compensate for multiple comparisons.
Discussion
During the decade between 1987 and 1997, the nature of psychotherapy in the United States underwent several important changes. There was an increase in use of psychotherapy by socioeconomically disadvantaged individuals, a rise in psychotherapy for mood disorders, a decline in psychotherapy for nonspecific conditions, greater use of psychotropic medications and involvement of physicians, and a decline in longer-term psychotherapy. We briefly consider each of these trends.
A significant increase was evident in the rate of psychotherapy for unemployed adults, and there were nonsignificant gains among the poor and those with little formal education. These groups are at especially high risk for untreated mental health problems. Poor and less well-educated people have higher rates of mental disorders than their more affluent counterparts
(14,
15) and are also less likely to seek mental health treatment
(16). Increasing access to outpatient psychotherapy for these vulnerable populations is a welcomed development.
The use of psychotherapy for the treatment of mood disorders increased. Advances in clinical assessment and psychopharmacological treatment may have contributed to this trend. During the decade, a new generation of rapid screening and diagnostic instruments became available for clinical use
(17–
19). In addition, the availability of selective serotonin reuptake inhibitors and other newer antidepressants may have increased the demand for treatment of depression and secondarily increased the use of psychotherapy for patients receiving these medications
(20). Increased public awareness of depression and its relative destigmatization may have further increased help seeking for mood disorders
(21). Once patients were in treatment, incomplete or unsatisfactory response to pharmacological treatments, preferences of patients or clinicians, or treatment history considerations may have led to initiation of psychotherapy.
The use of mood stabilizers among psychotherapy patients also increased. In recent years, several anticonvulsants have been discovered to have mood-stabilizing properties
(22,
23). Mood stabilizers have become accepted pharmacological options for a widening array of bipolar spectrum disorders
(24), schizoaffective disorder
(25), posttraumatic stress disorder
(26), and borderline personality disorder
(27). Growth in the number of mood stabilizers and their emerging clinical applications may have contributed to their increased use by psychotherapy patients.
Stimulants have also become more commonly used by psychotherapy patients. Recent growth in the use of stimulants has been reported from analyses of bulk methylphenidate production
(28), pharmacy-based audits
(29), surveys of physicians
(30,
31), school-based surveys
(32,
33), and Medicaid claims
(34,
35). The development of grassroots advocacy groups for attention deficit hyperactivity disorder (ADHD), including Children With Attention Deficit Disorder and the Attention Deficit Disorder Association, as well as federal reform affecting eligibility for special education services, is believed to have promoted recognition of ADHD and use of stimulants
(36).
Psychotherapy for unspecified conditions has become less frequent. The dramatic expansion of managed behavioral health care during the decade may have played a role in the decline of psychotherapy for poorly defined conditions. Under managed behavioral health care, approval of psychotherapy is often linked to “medical necessity” or other precertification utilization review criteria
(37). Such cost containment measures may encourage greater clinical efforts to focus psychotherapy on well-defined psychiatric conditions.
It is widely believed that managed care has shifted the provision of psychotherapy from psychologists, psychiatrists, and other physicians to other lower cost professionals
(38,
39). The current findings belie this belief. We found that physicians were increasingly involved in the provision of psychotherapy. Unfortunately, it is not possible to distinguish psychotherapy visits in the 1997 survey that were provided by psychiatrists from those provided by other physicians. According to the 1987 survey, however, psychiatrists provided more than five times as many psychotherapy visits as nonpsychiatrist physicians
(5).
The surveys also do not permit an assessment of whether patients treated with psychotherapy and psychotropic medications received integrated care (i.e., both pharmacotherapy and psychotherapy provided by a psychiatrist or other physician) or split treatment (i.e., pharmacotherapy provided by a physician and psychotherapy provided by another health professional). Some evidence suggests a recent growth in split treatment, although the effectiveness of such treatment and the cost implications of this development remain unclear
(40,
41).
Long-term psychotherapy became less common during the survey period. This change in the nature of psychotherapy may be related to growth in the number of private health plans that limit outpatient mental visits
(42,
43). It may also be a consequence of the resurgence of interest in cognitive behavior treatments
(44,
45) and of other evidence supporting time-limited psychotherapies
(46).
Approximately one-third of psychotherapy patients received only one or two sessions. Across a variety of patient populations and types of psychotherapy, there tends to be a dose-response relationship between the number of psychotherapy sessions and the amount of patient benefit
(47,
48). These findings suggest that much of the psychotherapy in the United States is shallow and of limited benefit. At the same time, it should be acknowledged that a group of experimental studies has supported the efficacy of single-session cognitive behavior therapies for a variety of specific phobias
(49–
52).
The surveys had several limitations. The National Medical Expenditure Survey and the Medical Expenditure Panel Survey collected data from household informants who may not have been fully aware of all of the services utilized by household members. Recall errors, stigma, and problems distinguishing psychotherapy from other health counseling pose threats to the survey data. A broad definition of psychotherapy also makes it impossible to distinguish simple nonspecific support and generic counseling from established formal psychotherapies. It would be useful if future national surveys characterized psychotherapies in a manner that differentiates various well-defined clinical techniques. Without an independent measure of symptoms, assessment of the validity of the reported diagnostic codes associated with the psychotherapy visits is not possible. Finally, while the National Medical Expenditure Survey and the Medical Expenditure Panel Survey collected information on services provided by the full range of health care professionals, several of these groups typically receive little or no formal training in the provision of psychotherapy.
In summary, the pattern of psychotherapy utilization in the United States underwent several important changes during the decade under study. The use of long-term psychotherapy declined overall, and the use of psychotropic medications increased. At the same time, some socioeconomically disadvantaged groups increased their use of psychotherapy, and individuals with severe mental disorders accounted for an increasing share of long-term patients. These changes occurred in the context of advances in psychopharmacological treatments, development of tools for rapid diagnosis, changing public attitudes toward mental health care treatment, and major revisions in the organization and financing of mental health services.
There is broad consumer satisfaction with psychotherapy
(53), even very brief forms of psychotherapy
(54). However, the effects of commonly available psychotherapies on patient outcomes remain poorly studied. Key challenges ahead include defining technical dimensions of psychotherapy in community practice and determining the clinical effectiveness of psychotherapy for the large number of individuals who receive this intervention.