There is consistent evidence that many, but not all, persons affected by schizophrenia and schizophrenia-like psychosis manifest poor social adjustment and subtle deviations from cognitive norms much before the illness is formally diagnosed. However, despite the many studies on this topic
(1–
4), the prevalence, course, characteristics, and correlates of the premorbid and prodromal impairments are far from clear. By studying the events preceding the first episode of psychosis and the multiple domains of psychosocial and educational functioning, it may be possible to detect protective or vulnerability factors and perhaps to devise interventions aimed at secondary prevention such as supplementary educational and vocational programs and other supportive measures. The goal of this study was to describe the patterns of premorbid functioning of a large cohort interviewed during their first episode of psychotic illness and to examine the relationship of premorbid functioning with symptom severity and cognitive functioning.
Method
The data presented here were derived from a retrospective premorbid assessment and the baseline assessment of subjects enrolled in a multicenter double-blind, randomized, controlled trial comparing a typical and a novel antipsychotic drug in the treatment of first-episode psychosis.
Subjects
The trial is being conducted in 11 countries and has enrolled psychotic patients between the ages of 16 and 45 years who have had a DSM-IV diagnosis, based on the Structured Clinical Interview for DSM-IV
(5), of schizophrenia, schizophreniform disorder, or schizoaffective disorder for less than 12 months and have had a maximum of two lifetime psychiatric hospitalizations for psychosis. The cumulative exposure to neuroleptics could not have exceeded 12 weeks. The study was conducted according to Good Clinical Practice guidelines and was approved by local institutional review boards. All subjects gave written informed consent before participating in the study.
The final study group included 535 persons (155 female subjects, median age=25.0 years; 380 male subjects, median age=23.8 years). Two persons left the trial before treatment but after random assignment, and 21 patients were excluded because the center where they were treated was removed from the trial owing to inconsistent data reporting. Patients were assigned the following DSM-IV diagnoses: schizophrenia (N=264), schizophreniform disorder (N=231), and schizoaffective disorder (N=40). Three-quarters of the study group were white (N=400), 12% (N=64) were black, 3% (N=17) were Hispanic, 2% (N=11) were Oriental, and 8% (N=43) were from assorted other groups. Fourteen percent (N=76) of the study group had no high school education, 27% (N=141) had some high school education, 21% (N=114) completed high school, 30% (N=159) completed some post–high school education, and 8% (N=41) completed college. (Data on education were missing for four subjects.) Female subjects were significantly older than male subjects at the time they first experienced psychotic symptoms (median=23.9 versus 22.6 years, Mann-Whitney U=24154, z=2.89, p=0.004). Eighty-eight percent of the patients (N=471) were 18 or older at the time of onset of first psychotic symptoms.
Assessments
The current analysis included data from a cognitive assessment and administration of the Premorbid Adjustment Scale
(6), the Positive and Negative Syndrome Scale
(7), and the Clinical Global Impression (CGI) severity scale
(8). All measures were applied at baseline before administration of the trial drug.
The Premorbid Adjustment Scale is a 28-item rating scale that assesses sociability and withdrawal, peer relationships, adaptation to school, and scholastic performance for four life stages (childhood, 11 years and younger; early adolescence, 12–15 years; late adolescence, 16–18 years; and adulthood, older than 18 years), as well as social-sexual aspects of life after age 15. The Premorbid Adjustment Scale also includes a section of nine general items relating to educational and job achievement, work and school performance immediately preceding onset of psychosis, highest level of independence from family, highest level of social personal adjustment, degree of interest in life, and energy level. The Premorbid Adjustment Scale was completed on the basis of all available data, including data from interviews with the patient and with collateral informants, if they were available.
The cognitive assessment, which is described in greater detail elsewhere
(9), included the 1) Wechsler Memory Scale—Revised visual reproduction subtest I and II
(10), a test of learning memory for nonverbal stimuli; 2) Rey Auditory Verbal Learning Test
(11), a test of verbal learning and memory; 3) Continuous Performance Test, Identical Pairs Version
(12), a test of vigilance; 4) verbal fluency examinations, including tests of category and phonological fluency
(13), a test of verbal productivity and intactness of the lexical system; 5) Wechsler Adult Intelligence Scale—Revised, digit symbol subtest
(14), a test of psychomotor speed and attention; and 6) Wisconsin Card Sorting Test
(15), a measure of executive functioning (e.g., cognitive flexibility, maintenance of a cognitive set, working memory). The tests, which were carefully chosen to be adaptable across cultures
(9), were translated from standard English versions into French, Finnish, German, Hebrew, and Afrikaans and administered to patients in their spoken language. A central monitoring facility evaluated case record forms, and all forms with errors were returned for correction. If the problems were the results of errors in administration, the cognitive testing data on those patients were not included in the study database.
All investigators were college educated, had previous research experience, and were fluent in English. Training in administering the assessment instruments was given in small group sessions at the local sites, as well as at regional meetings. At the meetings, videotapes of patient interviews were shown and the investigators filled out a scoring sheet. Individual investigators’ scores were then compared against a “master” scoring sheet developed by the trainers/developers of the videos. The pass/fail criterion for the rating examination was based on successfully meeting or exceeding an 80% concordance with the total and subscale scores designated on the master rating.
The Premorbid Adjustment Scale was completed for 531 of the 535 subjects, the Positive and Negative Syndrome Scale for 533, and the cognitive assessment for 508. Complete data on all measures were available for 503 subjects. For the Premorbid Adjustment Scale, the main study measure, data on some items were missing, as follows: one patient had missing data on one childhood item; two to six patients had missing data on any given early adolescence item; two to 12 patients had missing data on any given late adolescence item, with the most data missing on items relating to social aspects of sexual life during and immediately after adolescence; and nine patients had missing data on two adulthood items, which were filled out only for persons age 19 or older. On four of the six general items, the maximum number of patients with missing data per item was two. For the item measuring change in school or work performance before onset, data were missing for 20 patients. For a similar item measuring job change and school attendance, data were missing for 18 patients.
Analytic Plan
Data for each of the five Premorbid Adjustment Scale dimensions across the four life stages were analyzed with a repeated measures analysis of variance (ANOVA), controlling for gender and diagnosis. A separate general linear model multivariate analysis of variance (GLM MANOVA) was done for each dimension because all dimensions were not measured at every life stage (e.g., social-sexual aspects of life were not measured for childhood, and adaptation to school was not measured for adults). By using the scoring method developed by Cannon-Spoor et al.
(6), average scores for each life stage were computed by summing the scores received for each item in a section and dividing them by the possible score. The sum of the maximum possible score for all items completed indicates the highest score obtainable. Thus, for example, if a subject received ratings of 2, 3, 3, and 2 for the four items in the childhood section, the total score for that section would be 10. The total possible score was 24 (6+6+6+6), and the total score divided by the possible score was 0.42. When no information was available for a particular item, the item was not scored. The score for each section was expressed as total score divided by the possible score for the items rated.
For a normative comparison, we used the normative data provided by Cannon-Spoor et al.
(6). The mean score of the normal subjects was used to create a variable of normal functioning (versus below-normal functioning) in each of the four life stages. Premorbid functioning was described by using the classification method of Haas and Sweeney
(16), which included the following categories: stable–good, stable–poor, and deteriorating premorbid functioning. Deteriorating premorbid functioning, in terms of the Premorbid Adjustment Scale, was defined as “a pattern of worsening scores from childhood over the remaining premorbid periods and the equivalent of a 2-point change over four premorbid stages (childhood, early adolescence, late adolescence, and adulthood) or a proportional decline for cases in which illness onset was before late adolescence or adulthood.” The remaining patients were regarded as stable, and the median value (0.36) of the Premorbid Adjustment Scale total score was used as a cutoff point to assign these patients to stable–good or stable–poor groups. Data for patients were aggregated on this scale of premorbid functioning, and the three groups were compared on symptom and cognitive measures by using GLM MANOVA with diagnosis, sex, and exposure to antipsychotics as factors. Bonferroni-corrected significance levels for between-group differences are reported. The Bonferroni correction consisted of multiplying each p value by 3, since three comparisons were made (e.g., p=0.05 with Bonferroni correction is presented as p=0.15).
Results
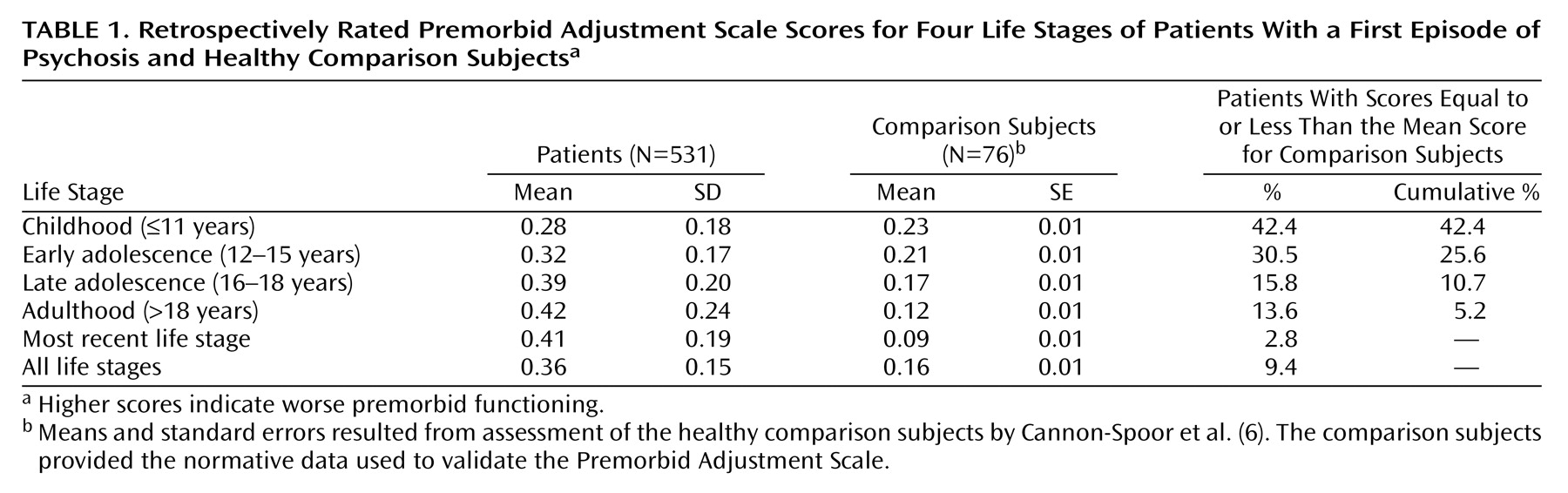
Table 1 presents the subjects’ mean scores on the Premorbid Adjustment Scale for each life stage. The normative data on healthy comparison subjects from the work of Cannon-Spoor et al.
(6) are also shown in
Table 1. The mean score for childhood for the patients in this study was 0.28, which was somewhat higher (reflecting worse functioning) than that for the healthy comparison subjects, who had a mean score of 0.23. Of the patients in this study, 42.4% had scores for the childhood period that were no worse than the mean score for the healthy comparison subjects. The mean score differences between the patients and the comparison subjects increased with each successive time period, and concomitantly the percentage of patients with normal functioning decreased during subsequent periods. The last column of
Table 1 shows the cumulative percentage of patients who functioned within the normal range for each life stage and the preceding stages.
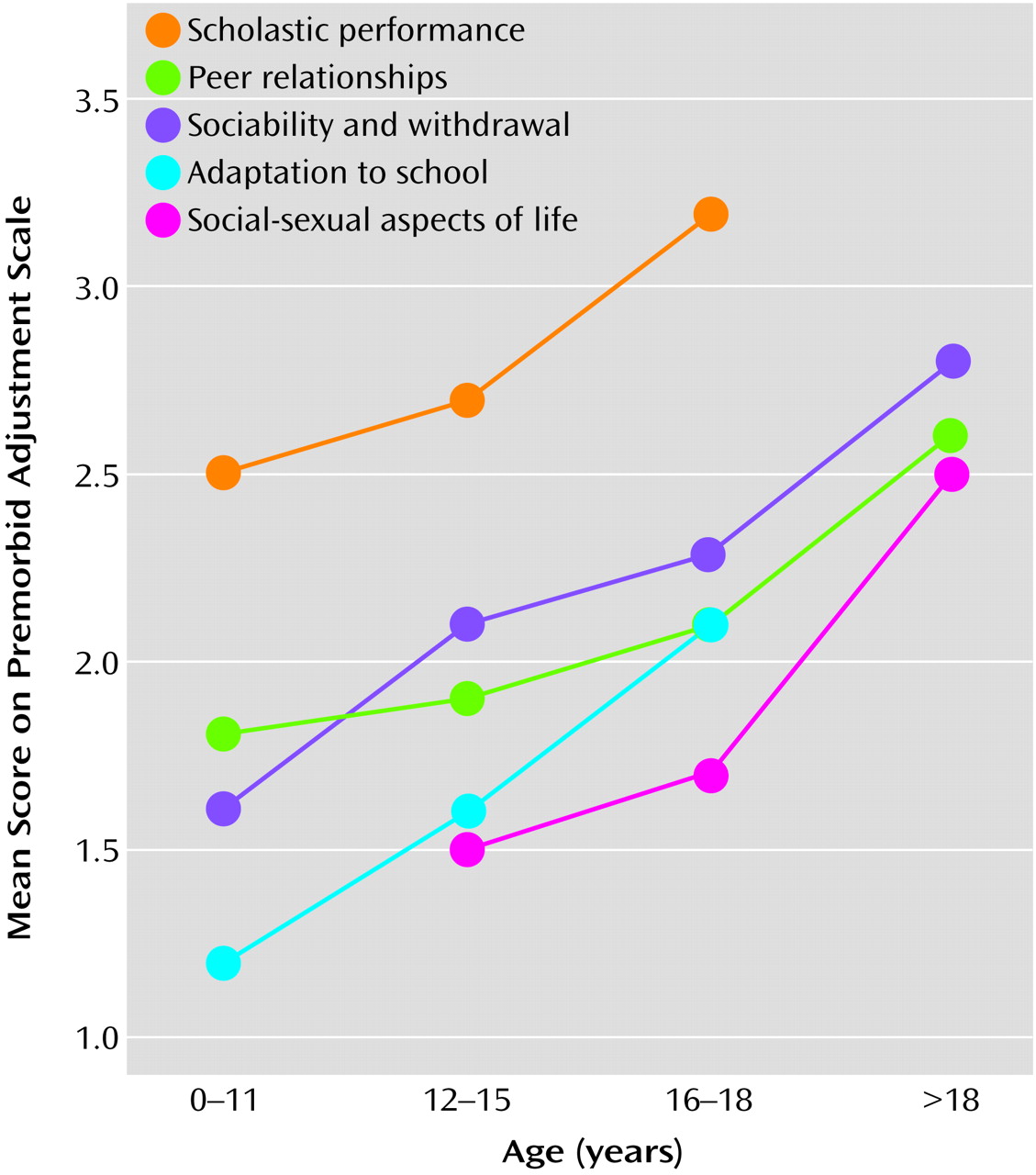
Figure 1 presents the patients’ mean scores on the Premorbid Adjustment Scale across the four life stages assessed. A repeated measures ANOVA comparing these scores across the life stages found an overall significant difference and a significant linear trend (decline) on all five dimensions measured (sociability and withdrawal: F=32.1, df=3, 1383, p<0.0001 and F=53.2, df=1, 461, p<0.0001; peer relationships: F=29.6, df=3, 1383, p<0.0001 and F=47.6, df=1, 461, p<0.0001; scholastic performance: F=35.7, df=2, 988, p<0.0001 and F=48.8, df=1, 494, p<0.0001; adaptation to school: F=51.5, df=2, 978, p<0.0001 and F=74.6, df=1, 489, p<0.0001; and social-sexual aspects: F=32.7, df=2, 878, p<0.0001 and F=47.5, df=1, 439, p<0.0001).
Using the method of Haas and Sweeney
(16), 47.5% of the subjects (N=252) were categorized as having stable–good premorbid functioning; 37.3% (N=198) as having stable–poor functioning; and 15.3% (N=81) as having deteriorating premorbid functioning. Although the Haas scale is based on a different method of computation (described in detail in the section on data analysis) than the method used to compare the overall group of patients to the comparison subjects, the stable–good group had mean scores that were similar to those of the comparison subjects (reported in
Table 1) for childhood and early adolescence (childhood: 0.19 and 0.23, respectively; early adolescence: 0.21 and 0.21, respectively) and different from those of the comparison subjects for late adolescence and adulthood scores (late adolescence: 0.24 versus 0.17; adulthood: 0.24 versus 0.12).
Female subjects had significantly better premorbid functioning (stable–good: 57%, N=88; stable–poor: 34%, N=53; deteriorating: 9%, N=14) than male subjects (stable–good: 44%, N=164; stable–poor: 18%, N=67; deteriorating 39%, N=145) (χ2=10.1, df=2, p=0.006). Patients with a diagnosis of schizophreniform disorder had better premorbid functioning (stable–good: 62%, N=143; stable–poor: 27%, N=61; deteriorating: 11%, N=25) than those with schizoaffective disorder (stable–good: 40%, N=16; stable–poor: 48%, N=19; deteriorating: 13%, N=5) or schizophrenia (stable–good: 36%, N=93; stable–poor: 45%, N=118; deteriorating 19%, N=51) (χ2=37.6, df=4, p<0.006).
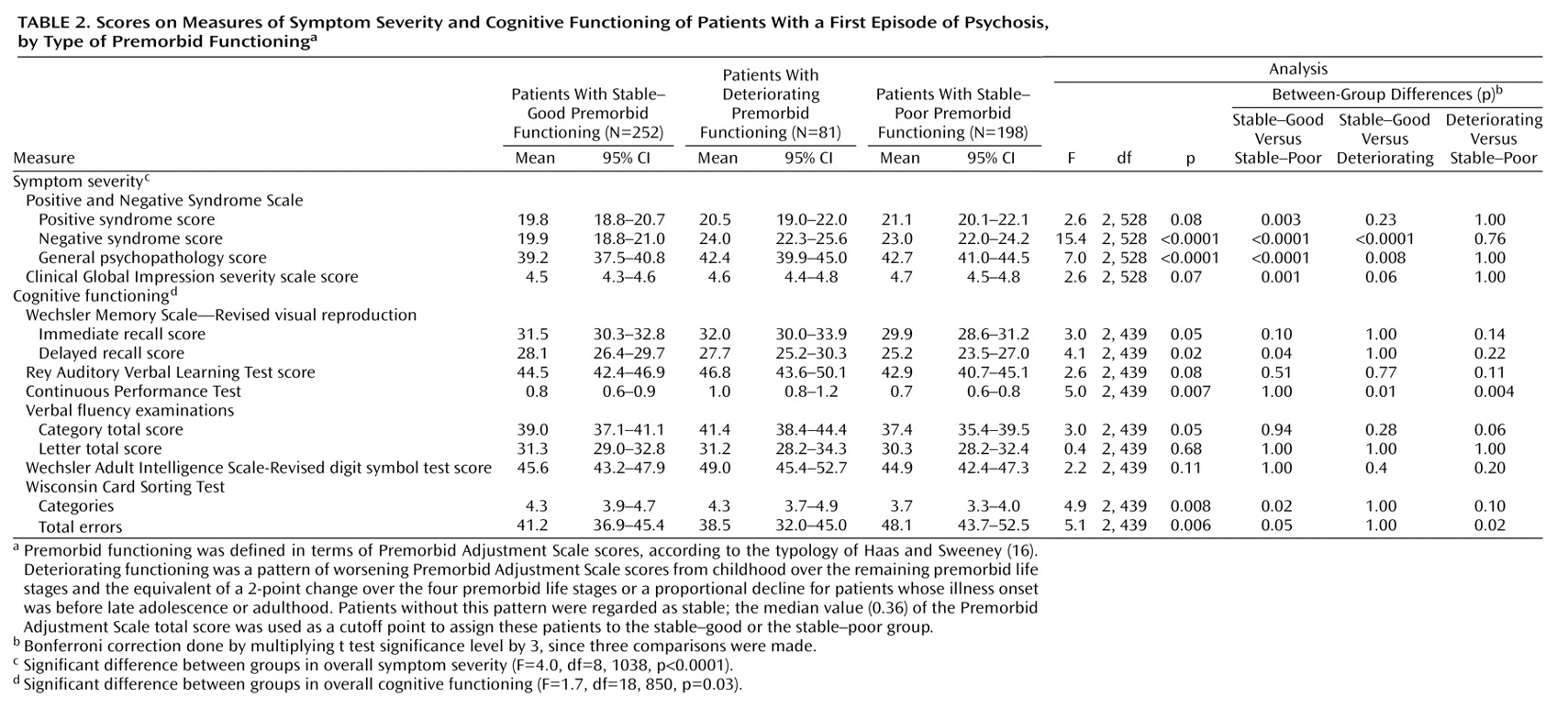
Table 2 presents mean scores on the Positive and Negative Syndrome Scale and cognitive measures for the patients with stable–poor, stable–good, and deteriorating premorbid functioning. Overall there were significant differences in both symptoms and cognition (multivariate tests presented in footnotes “c” and “d” of
Table 2). Significant differences were found in the Positive and Negative Syndrome Scale negative syndrome and general psychopathology scores. Nearly significant differences were found in the Positive and Negative Syndrome Scale positive syndrome score and the CGI severity scale score. Significant differences were found on six of the nine cognitive measures, and the difference between groups for one more cognitive measure was nearly significant. The patients classified as having stable–good premorbid functioning had significantly better scores on the Positive and Negative Syndrome Scale negative syndrome, positive syndrome, and general psychopathology subscales, on the CGI severity scale, and on three cognitive measures, compared to the stable–poor group. Similarly, the stable–good group had significantly better scores than the deteriorating group on the Positive and Negative Syndrome Scale negative and general psychopathology subscales and the CGI, and significantly worse scores on one cognitive measure. The stable–poor group had significantly worse performance on three cognitive measures, compared to the deteriorating group, but the scores on the CGI and Positive and Negative Syndrome Scale were not different between those groups.
Discriminant function analysis with the stepwise procedure based on Wilks’s lambda was conducted to examine the relative importance of scores on the Positive and Negative Syndrome Scale subscales, the CGI, and the cognitive variables in discriminating between the three types of premorbid adjustment. The two variables that significantly discriminated between the groups were the Positive and Negative Syndrome Scale negative subscale score, which was the first variable entered in the model (F=18.9, df=2, 434, p<0.0001), and the score on the category test of the verbal fluency examinations, which was the second variable added to the model (F=12.3, df=4, 866, p<0.0001).
Discussion
More than half of the subjects in this study, who were experiencing a first episode of psychosis, had some disturbances long before the episode. Although 88% of the patients had onset of psychosis after age 18, 84% showed a disturbance in functioning, relative to the functioning of normal comparison subjects, before age 18, almost 70% before age 15, and 58% before age 11. Poorer premorbid functioning long before onset of psychosis was associated with more severe manifestations of illness at the first psychotic episode, both in terms of symptoms and cognitive functioning. The results presented here are consistent with reports indicating that deviations in functioning, particularly in social adjustment, are present in many, but not all, individuals affected by psychosis and schizophrenia long before the psychotic illness is formally diagnosed or even manifested
(1–
4). The deviations can take the form of poor interpersonal relationships, withdrawal behavior, eccentricity, or even attenuated psychotic symptoms. For some individuals, these deviations might manifest as shyness and poor scholastic achievement during childhood, continuing as a crescendo of progressive deterioration during adolescence. For others, the deviations may be barely detectable, manifesting as few putative behavioral abnormalities shortly before the diagnosis of the first psychotic episode.
Furthermore, the transitions from premorbid to prodromal manifestations and then to the emergence of the symptoms that define the first episode of psychosis and the subsequent diagnosis are not always clearly distinct points in time or distinctive illness-related events. Family structure and education or access to care might affect when the diagnosis occurs
(17–
19), hence determining the length of the premorbid and prodromal manifestations as well as determining which manifestations are classified as premorbid, prodromal, or part of the first psychotic episode.
The results presented here indicate that, as a group, individuals affected by psychosis are likely to show continuous deterioration of social functioning from childhood through adolescence, as the first episode of psychosis approaches. However, only 15% of the subjects (those with deteriorating premorbid functioning) showed a clear transition from a higher to a lower level of social functioning. Hence the data lend tentative support to the existence of a subgroup of patients with gradual premorbid social deterioration and a subgroup who lack developmental progress.
Limitations of the data in this study and previous studies may account for the variation in findings about the quality and timing of premorbid manifestations. The data were limited in part because they were derived from cross-sectional assessments conducted at the patient’s first contact with a mental health professional
(20). In addition, the data were based on the subjective recollections of a variety of sources, including the patient, family members, and other collateral informants. It is conceivable that a true prospective follow-up study, specifically designed to detect signs of premorbid psychosis and schizophrenia and conducted from birth through age of risk, would reveal a specific trajectory of social maladjustment for the majority of individuals destined to be affected by psychosis. Alternately, the premorbid and prodromal manifestations may be obligatory precursors of the illness for only some individuals or for only a subgroup of the schizophrenias. Another limitation of this study is the potential for a selection bias, given that the data were obtained from patients who agreed to be enrolled in a medication trial. However, it is not obvious how such a bias might affect the conclusions that can be drawn from the study.
In this study, approximately half of a group of subjects with a first episode of psychosis retrospectively reported poor premorbid social adjustment. This finding is consistent with data that have been collected prospectively. In a prospective historical study in which social adjustment was assessed in apparently healthy adolescents, poor social adjustment was reported regarding as many as 44% of subjects assigned a diagnosis of schizophrenia 1 or more years (mean=4 years), compared to only 7% of the subjects of the same age who remained healthy
(21). This finding supports the accuracy of the prevalence of premorbid maladjustment reported in this study.
The results of this study are consistent with previous reports about first-episode schizophrenia. Most studies in this area have found that individuals with poorer (as opposed to better) premorbid functioning also have more severe symptoms, as reflected by the negative syndrome subscale of the Positive and Negative Syndrome Scale and the CGI, as well as worse cognitive performance, as measured with standard neuropsychological tests. The relationships between the Premorbid Adjustment Scale scores and the Positive and Negative Syndrome Scale, CGI, and cognitive scores can be interpreted in a number of ways. The different scales may assess similar domains, or there may be overlap between scales in the content of individual scale items. Scoring on one scale could be affected by scoring on another scale, particularly if the two scales are scored during the same session by the same rater.
Alternatively, a particular subgroup of schizophrenic disorders may be defined by an early pathophysiological process that manifests as poor social adjustment during childhood and adolescence. This process may then evolve into more severe negative and general symptoms, as well as poorer cognitive performance in early adulthood and at the onset of psychosis. A number of scenarios could be responsible for these pathophysiological processes. An accumulation of genetic and environmental risk factors (or lack of environmental protective factors), consistent with a “multiple-hit” hypothesis, may lead to the premorbid manifestations, and an environmental insult or a gene expressed later in life may be necessary for the full syndrome of schizophrenia to develop. Depending on the nature of the additional, later insults, the same early-life manifestations (e.g., marginal social adjustment) might remain stable through life, evolve into milder mental disorders such as schizotypal personality disorder, or lead to schizophrenia. If indeed the phenotype of schizophrenia reflects the consequences of an accumulation of genetic and environmental risk factors, research examining the course of the disease from birth through the age of risk may be required to identify specific etiological patterns.