The most recent edition of the DSM allows borderline personality disorder to be diagnosed in younger patients when maladaptive traits have been present for at least 1 year and are “pervasive, persistent, and unlikely to be limited to a particular developmental stage or an episode of an Axis I disorder” (DSM-IV, p. 631). Except for shortening the duration criterion, however, the diagnostic criteria themselves are identical to those for adults. Although the clinical significance of the borderline personality disorder diagnosis and criteria in adolescents remains largely unclear, the past decade has brought several empirical investigations of this area of psychopathology (e.g., references
1–4). One group
(2) focused on developmental histories and trauma exposure in patients with borderline personality disorder, although they did not use DSM criteria in defining borderline personality disorder. Pinto and colleagues
(4) used DSM-III-R criteria and a non-DSM-based semistructured interview to study borderline personality disorder in hospitalized adolescents and demonstrated some degree of concurrent validity for this diagnostic construct. However, they found that with the exception of poor self-concept (e.g., “emptiness” and “identity disturbance”), other affective and cognitive phenomena were not specific to borderline personality disorder in this study population. Meijer and co-workers
(3) also used DSM-III-R definitions and a non-DSM-based semistructured interview to evaluate stability of the borderline personality disorder diagnosis and symptoms in hospitalized adolescents. They found low stability of borderline personality disorder, which was attributed to low persistence of self-mutilation, suicidal threats, and dissociative/paranoid experiences.
The Yale Psychiatric Institute Adolescent Follow-Up Study used semistructured diagnostic interviews for DSM-III-R disorders to examine a broad range of psychopathology and personality disorders in general; some of these results also shed light on borderline personality disorder in particular. These inpatient studies have demonstrated that personality disorders in adolescents can be reliably diagnosed, occur frequently, and have concurrent validity but that they have only modest predictive validity and are relatively unstable over time
(5–
7). These general findings for hospitalized adolescents are consistent with those of other studies involving community samples
(8,
9).
We further examined personality disorder construct validity in hospitalized adolescents by evaluating internal consistency of personality disorder criteria within diagnoses as well as criterion overlap between diagnoses
(10). Compared with an analogous group of adult inpatients, we generally found personality disorder criteria in adolescents to have lower internal consistency and less discriminant validity. Borderline personality disorder did not show lower internal consistency in the adolescents, but the pattern of criterion overlap for borderline personality disorder was broader, which suggests that this disorder represents a more diffuse range of psychopathology in this age group. Similarly, our comparison of adolescent and adult inpatients with regard to axis II comorbidity of borderline personality disorder indicated a broader pattern of personality disorder co-occurrence in the adolescents
(1).
Another approach to understanding the nature and significance of borderline personality disorder and its symptoms in adolescents is by studying the diagnostic efficiency of borderline personality disorder criteria. The seminal article of Widiger and colleagues
(11) illustrates both an overall approach to studying diagnostic efficiency and its application to borderline personality disorder in particular. Diagnostic efficiency is the extent to which diagnostic criteria (or symptoms) are able to discriminate individuals with a given disorder from those without that disorder, as determined by the application of conditional probabilities
(11,
12). Four such conditional probabilities can be useful in studying the diagnostic efficiency of symptoms: sensitivity, specificity, positive predictive power, and negative predictive power.
Despite their frequent use in research, sensitivity and specificity have limited utility in the process of clinical diagnosis. Widiger and colleagues
(11) emphasize that diagnosticians are more interested in the likelihood of a disorder given that the patient has a symptom than in the likelihood of a symptom given that the patient has a disorder, and that, similarly, negative predictive power is more useful than specificity. A symptom’s positive predictive power indicates whether it will have utility as an inclusion criterion. Moreover, the relative values of the positive predictive powers for various symptoms of a disorder can provide information about which symptoms are the strongest predictors of the disorder. This feature represents a potential improvement over the symptom lists provided in the DSM, where all inclusion criteria are generally viewed as equivalent in predictive capacity. Similarly, a symptom’s negative predictive power tells us whether the absence of that symptom will have utility as an exclusion criterion. Finally, some authors
(12) have employed total predictive value as an index of a symptom’s utility in making a correct diagnosis. Although not a conditional probability, total predictive value is a measure of percent agreement and represents the total probability of correct classification.
Sensitivity and specificity are independent of the base rate of a disorder. By contrast, positive predictive power, negative predictive power, and total predictive value will vary with disorder base rates
(11,
12). It can be shown that for any given sensitivity and specificity values, symptoms are more likely to be valid indicators of the presence of a disorder than of its absence (i.e., positive predictive power >0.50) when disorder base rates are higher
(11). Put differently, positive predictive power will tend to increase with increasing disorder base rates; negative predictive power, by contrast, will tend to decrease with increasing disorder base rates.
Widiger and colleagues
(11) applied these concepts to adult outpatients with personality disorders, although they did not use a research diagnostic interview for DSM-III
(13). In this group, the disorder base rate was 0.34. Positive predictive powers averaged 0.67 and ranged from 0.56 to 0.73, indicating that all borderline personality disorder criteria had a degree of diagnostic efficiency, although some had more than others. Pfohl and colleagues
(14) also reported diagnostic efficiency of DSM-III personality disorder criteria in a clinical sample of adults; these investigators did use a structured diagnostic instrument. For borderline personality disorder, the disorder base rate was lower (0.22) than that reported by Widiger’s group; as expected, the average positive predictive power was also lower (0.58), ranging from 0.42 to 0.76. Also, these investigators reported negative predictive powers for borderline personality disorder criteria that were higher than the positive predictive powers, averaging 0.94.
Conditional probabilities have also been used to study the diagnostic efficiency of the criteria for disruptive behavior disorders in children
(12,
15). To our knowledge, however, there have been no similar studies of personality disorders in younger populations. Such investigations in adolescents may help us to understand better the extent to which these disorders may be different in this age group than in adults.
This study aimed to evaluate the diagnostic efficiency of DSM-III-R criteria for borderline personality disorder in a group of adolescent inpatients who had been reliably assessed with a semistructured diagnostic interview. For comparison, we performed the same analysis on a group of concurrently recruited adult inpatients who had been subjected to identical assessment procedures.
Method
Subjects
Adolescent subjects were drawn from 138 consecutive admissions to the Adolescent Inpatient Unit of the Yale Psychiatric Institute, a tertiary care psychiatric facility. A detailed description of this heterogeneous group is given elsewhere
(7). For this study, we used all patients from the consecutive series for whom there was complete borderline personality disorder criterion data (N=123).
Of these 123 adolescents, 67 were male and 56 were female. They ranged in age from 13 to 18 years (mean=15.9, SD=1.3). With regard to ethnicity, 104 were Caucasian, 10 were African American, four were Asian American, and five were of other backgrounds. Subjects were predominantly of middle-class socioeconomic status. At admission, the mean Global Assessment of Functioning score (from DSM-III-R) was 38.7 (SD=6.4).
A group of 106 adult inpatients, drawn from a series of 117 consecutive admissions to the same hospital during the same time period, was used for comparison. This group consisted of 56 male and 50 female subjects, with a mean age of 23.8 years (SD=5.4). Again, most (N=102) were Caucasian, and most were of middle-class socioeconomic status. The mean admission Global Assessment of Functioning score was 35.3 (SD=11.1).
After complete explanation of study procedures, written informed consent was obtained from all subjects. In the case of minors, assent was obtained from subjects, and consent was obtained from their parents or guardians.
Procedures
All subjects received a diagnostic evaluation that included the Personality Disorder Examination
(16), a semistructured diagnostic interview that assesses DSM-III-R personality disorders. Traits must be pervasive and persistent for at least 5 years in adults and for at least 3 years in adolescents
(16).
Interviews were conducted by a trained and monitored research team that functioned independently of the clinical team and that was blind to study aims. Interrater reliability of Personality Disorder Examination diagnoses was assessed by independent, simultaneous ratings by pairs of raters on 26 subjects from the overall study group; kappa coefficients were high (mean=0.84, SD=0.14); for borderline personality disorder, kappa=0.84.
Final research diagnoses were assigned at an evaluation conference, attended only by the research team, approximately 4 weeks after admission. These diagnoses were established by the best-estimate method on the basis of structured interviews and additional relevant medical record data (e.g., admission notes, clinician descriptions, and information obtained from family), following the LEAD (longitudinal, expert, all data) standard
(17). Agreement was high between final research diagnoses and Personality Disorder Examination diagnoses; among the 229 subjects in this study, concurrence for the borderline personality disorder diagnosis was 88% (kappa=0.76).
For each borderline personality disorder criterion, sensitivity, specificity, positive predictive power, negative predictive power, and total predictive value were calculated. These statistics were determined separately for adolescents and adults, then the groups were compared.
Results
The adolescent and adult groups were statistically compared with respect to demographic and severity variables. No significant differences were found for gender or socioeconomic status. The adult group had a significantly greater proportion of Caucasian subjects (χ2=7.3, df=1, p=0.007) and a lower mean admission Global Assessment of Functioning score (F=7.3, df=1, 195, p=0.008). Sixty-five (53%) of the adolescents and 50 adults (47%) were diagnosed with borderline personality disorder; these proportions were not statistically different. Among the adolescents, 45% (N=30) of the male and 63% (N=35) of the female subjects had borderline personality disorder; among the adults, 43% (N=24) of the male and 52% (N=26) of the female subjects had borderline personality disorder. For neither group were these proportions statistically different.
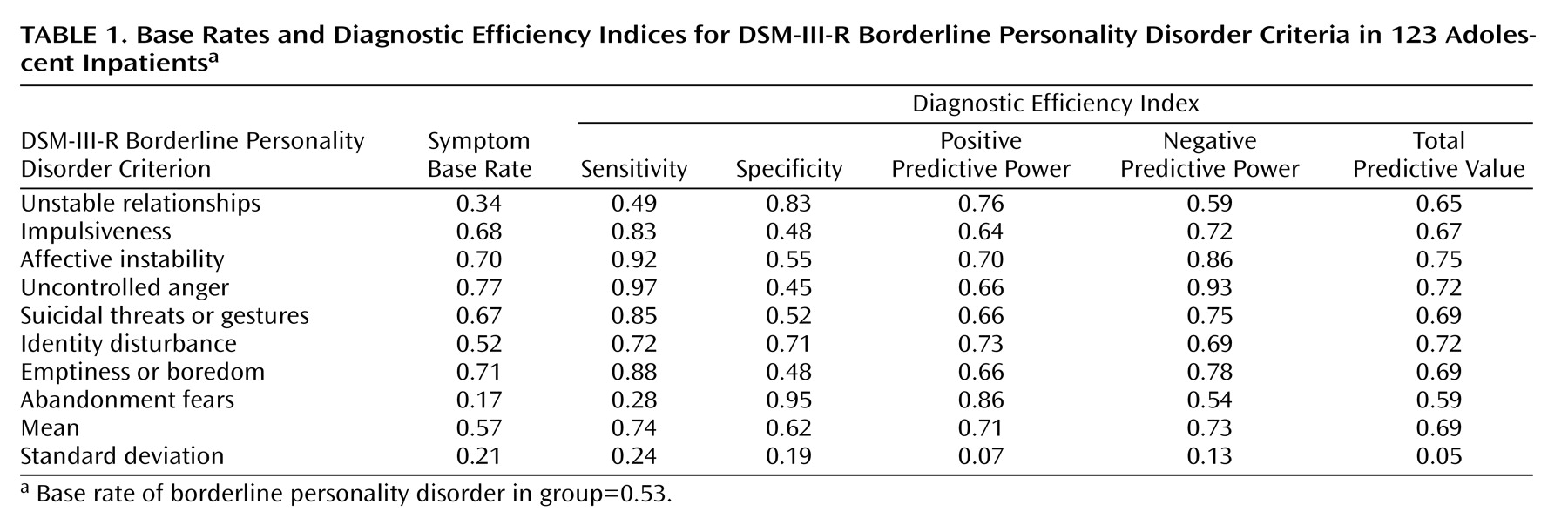
Table 1 shows symptom base rates and diagnostic efficiency indices for the eight DSM-III-R borderline personality disorder criteria in the adolescent group. Five symptoms were found in at least two-thirds of the subjects. It is interesting that in this adolescent study group, identity disturbance was found in only about one-half of the subjects. Unstable relationships were found in about one-third of the subjects, and abandonment fears were even less frequent. It is not surprising that the five symptoms with the highest frequencies also had relatively high sensitivities (>0.80) and that the two with the lowest frequencies had similarly high specificities.
The positive predictive powers indicate that all symptoms had some positive predictive value in the diagnosis of borderline personality disorder (i.e., for all symptoms, positive predictive power >0.50). This result is not surprising, given that the disorder base rate was about 50%. Positive predictive power ranged from 0.64 for impulsiveness to 0.86 for abandonment fears. Negative predictive power formed a broader range, from 0.54 for abandonment fears to 0.93 for uncontrolled anger. Taking both positive and negative predictive capacity into account, the total predictive values indicated that affective instability, uncontrolled anger, and identity disturbance have the most overall utility in correctly diagnosing borderline personality disorder.
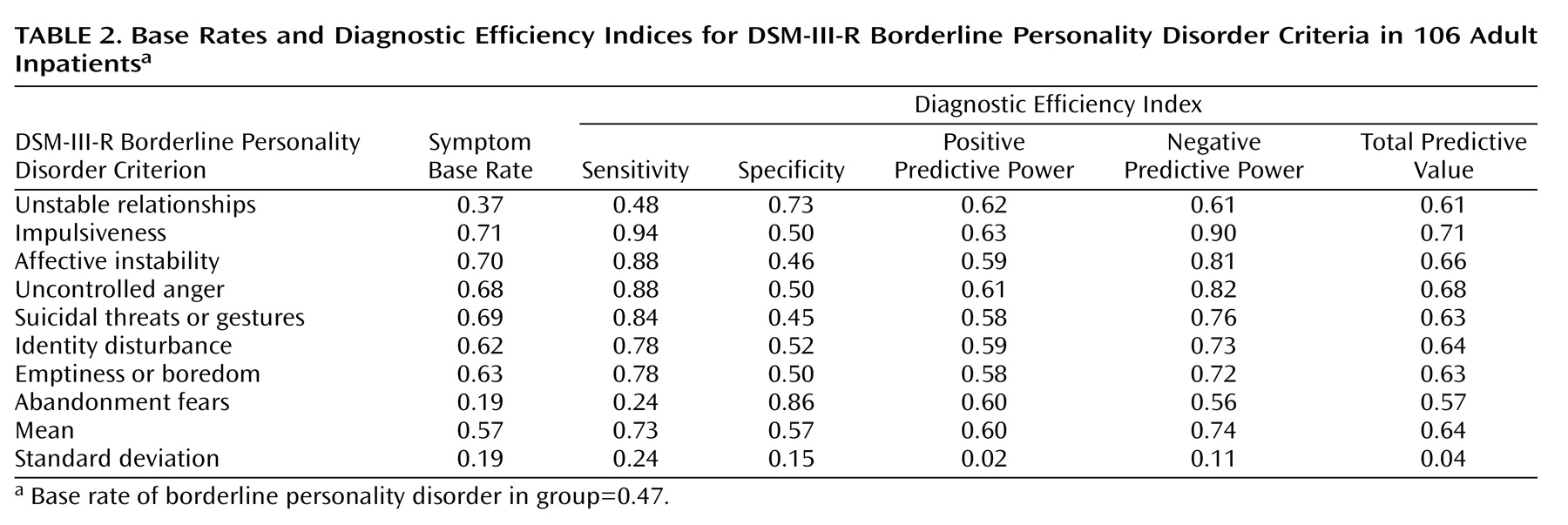
Table 2 shows symptom base rates and diagnostic efficiency indices for the borderline personality disorder criteria in the adult group. The symptom frequencies were similar to those in the adolescents. Again, abandonment fears were the least frequent symptom, followed by unstable relationships. The other six symptoms occurred in at least 60% of the subjects. Chi-square analysis revealed no significant differences between the two groups with respect to any of the symptom frequencies. The ranges for the sensitivities and specificities of the borderline personality disorder criteria were similar to those of the adolescent group.
The range of the negative predictive powers in the adults was comparable to that of the adolescents, although the pattern was slightly different, with abandonment fears still having the lowest negative predictive power but impulsiveness having the highest negative predictive power. Again, the positive predictive powers in the adult group were all greater than 0.50, although the range was more narrow, with none being distinctly higher than the others. The total predictive values indicated that for the adults, impulsiveness has the most overall utility in diagnosing borderline personality disorder.
Finally, we used a nonparametric statistical approach to compare the two groups with respect to the symptom base rates and diagnostic efficiency indices presented in
Table 1 and
Table 2 and found that the groups differed only for positive predictive power (p<0.0002, Mann-Whitney U exact test).
Discussion
Our study, which examined the diagnostic efficiency of DSM-III-R borderline personality disorder criteria in study groups of adult and adolescent inpatients—from diagnostic and criterion data obtained with reliably administered structured research interviews—contributes to a growing literature on borderline personality disorder and its symptoms in adolescents. Our adult and adolescent study groups had similar base rates for the borderline personality disorder diagnosis and also had similar base rates for the borderline personality disorder criteria. These findings suggest some general similarities between the age groups with respect to borderline personality disorder.
Despite these surface similarities between the groups with respect to symptom patterns, we found several differences at the level of the diagnostic efficiency of borderline personality disorder criteria. In adults, no symptom had clear advantage as an inclusion criterion, which is consistent with the DSM’s approach in which all symptoms are viewed as equivalent in their predictive capacities. In adolescents, by contrast, some symptoms had distinctly higher positive predictive powers, with abandonment fears having the most utility as an inclusion criterion. While all borderline personality disorder symptoms demonstrated some positive predictive value in both age groups, in the adolescents the symptoms had significantly higher overall positive predictive power. In other words, adolescent individuals with a single borderline personality disorder symptom are more likely to warrant the borderline personality disorder diagnosis than are adults with a single borderline personality disorder symptom. We also found differences between groups with respect to negative predictive power. The absence of impulsiveness was shown to be the best exclusion criterion for the adults, whereas the absence of uncontrolled anger was the best exclusion criterion for the adolescents. Taking both positive and negative predictive capacity into account, the highest total predictive value was found for impulsiveness in the adults and for affective instability in the adolescents.
Our findings regarding adults vary somewhat from those reported by Widiger and colleagues
(11) in their study of adult outpatients. They found a broader range for positive predictive power than we did, with unstable relationships and emptiness or boredom being the best inclusion criteria. Pfohl and colleagues
(14) also found a broader range for positive predictive power, with unstable relationships and suicidal threats or gestures having the highest values. These discrepancies are perhaps attributable to study group differences or to differences in diagnostic methods.
Our findings in adolescents do not support the observation by Pinto and colleagues
(4) that emptiness or boredom is among the best discriminators of borderline personality disorder in adolescents, although our findings are consistent with their results in showing that identity disturbance is more useful than most borderline personality disorder symptoms in leading to a correct diagnosis. The only symptoms with equal or better total predictive value in adolescents are affective instability and uncontrolled anger, which suggests that in general, symptoms of poor affective regulation may be most characteristic of the borderline personality disorder diagnosis in this age group.
Strengths of this study include our use of two nearly consecutive series of patients concurrently admitted to similar levels of care within the same hospital. Moreover, the groups were subjected to identical axis II assessment protocols administered by the same evaluation team. Our methods therefore tended to reduce sampling and selection confounds and allowed for meaningful comparisons between groups. Also, while we relied solely on the Personality Disorder Examination to provide data regarding the individual criteria, diagnoses were made according to the LEAD standard. Finally, our use of a conservative duration criterion
(16)—more stringent than either DSM-III-R or DSM-IV—may have minimized trait-state artifacts
(18), suggesting that our results are not simply reflective of acute axis I pathology.
Our study also has several limitations. First, we used DSM-III-R criteria for borderline personality disorder. While the wording of some items was modified slightly for DSM-IV, there are no substantial changes except for the addition of one item (“transient paranoia”). Second, we relied on just one semistructured diagnostic interview, the Personality Disorder Examination. Given the modest convergence between different instruments
(19), our results may have been different had we used an alternative diagnostic interview. Also, the Personality Disorder Examination may have elicited slightly different responses in adults and adolescents. Finally, these inpatient subjects, with a relatively high base rate of borderline personality disorder, were representative of severely ill populations; our results therefore may not be generalizable to community settings or to the many clinical settings in which disorder base rates may be lower.
Clinical Implications
Despite these limitations, several conclusions can be drawn from our data. First, comparison of the symptom base rates for the two groups suggests that symptoms of dysregulated affect, behavior, and identity—once thought to be characteristic of adolescence—are not more commonly found in hospitalized adolescents than in hospitalized adults. Second, in adolescents, but not in adults, some borderline personality disorder criteria appear to be more likely than others to predict the borderline personality disorder diagnosis. This finding may be clinically useful in acute treatment settings, where complete symptom data can be difficult to collect. Also, clinicians who arrive at the borderline personality disorder diagnosis through a traditional clinical interview
(20), while not necessarily conducting an exhaustive inventory of DSM criteria—may find confirmatory evidence for their diagnosis by specifically inquiring about one or two symptoms. For instance, in hospitalized populations represented by our adolescent study group, patients who endorsed the symptom of abandonment fears had about an 85% chance of meeting full DSM criteria for borderline personality disorder. Conversely, such patients who did not endorse uncontrolled anger had better than a 90% chance of not meeting diagnostic criteria.
Third, in adolescents, the symptoms with the highest likelihood of leading to a correct diagnosis with respect to borderline personality disorder were identity disturbance and two criteria that involve aspects of affective dysregulation. That identity disturbance has specific value in discriminating the diagnosis of borderline personality disorder is of interest, since this trait is often viewed as a common and nonspecific manifestation in this age group. That symptoms of affective dysregulation also have specific value in discriminating the diagnosis of borderline personality disorder may shed light on the underlying nature of this syndrome in adolescents. Several investigators have suggested that borderline personality disorder has statistically meaningful components and, moreover, that such components or symptom groupings may be clinically significant and may respond to specific treatment interventions
(21–
25). For instance, some researchers have argued that impulsiveness is a core feature of borderline personality disorder in adults and that the course of borderline personality disorder in this age group can best be influenced by pharmacologic and psychosocial interventions aimed at this symptom area
(22,
23). Indeed, our own total predictive value results in the adult group would tend to support this view. To the extent that affective dysregulation, instead, may be a core feature of borderline personality disorder in adolescents, it might suggest an alternative set of preferred interventions in this age group
(24,
25).
Implications for the DSM
While the DSM has included a category of personality disorders since the first edition was published a half century ago, the third edition placed these disorders on a distinct axis II in order to ensure that clinicians consider “the possible presence of disorders that are frequently overlooked when attention is directed to the usually more florid Axis I disorder” (DSM-III, p. 23). This separation of personality disorders reflected, in part, clinical lore that these disorders are different from other mental disorders, primarily in terms of their presumed refractoriness to treatment and their persistence or stability over time
(26).
Although research on personality disorders has burgeoned over the past two decades, basic questions have remained regarding the nature and validity of these disorders
(26). Some of these concerns, including that of questionable reliability
(27), highlight the need for basic psychometric work to guide the continued refinement of the criteria and diagnoses
(28). Some psychometric approaches have yielded findings regarding the convergent and discriminant validity of personality disorder criteria and diagnoses
(10,
29). In this study, we have focused our attention on complementary analyses that have relevance to the utility of specific criteria for arriving at a specific diagnosis.
Our findings illustrate the potential advantages of considering the various diagnostic criteria as having unequal value in leading to the diagnosis of personality disorder. Also, our somewhat divergent results for the two age groups suggest that there may be merit in developing personality disorder criteria for adolescents that are distinct from those used for adults. The present results suggest that there may be core features of borderline personality disorder in adolescents. It is possible that diagnostic criteria that emphasize these features could lead to a borderline personality disorder construct with enhanced predictive and discriminant validity and with improved stability over time.