However, caution must be exercised in investigations of psychosocial adversity in family studies with similar research designs. Examination of the effect of environmental factors on genetically mediated childhood psychopathology outside twin/adoption studies or molecular genetic paradigms makes it difficult to separate the effect of environmental factors from the genetic liability imparted by parents. Even with statistical adjustment of parental diagnostic status, residual confounding resulting from genetic factors may remain to obscure the relationship between an environmental factor and offspring outcomes. As such, empirical definitions of environmental adversity in family studies must be considered phenomenological, and the results must be interpreted with these issues in mind. Thus, positive findings about the impact of psychosocial factors should motivate genetic studies to clarify the role of genetics and environment in their genesis.
The purpose of this study was to reexamine the impact of psychosocial adversity indexed through Rutter’s indicators of adversity as risk factors for ADHD and its associated dysfunction relating to gender, parental ADHD, and maternal smoking during pregnancy. We hypothesized that the cumulative number of Rutter’s indicators would be risk factors for ADHD and its associated comorbidity in both genders, independent of parental ADHD and maternal smoking during pregnancy.
Method
Subjects were derived from two identically designed case-control family studies of male
(10) and female
(11) probands with (N=280) and without (N=242) DSM-III-R ADHD, who were ascertained from pediatric and psychiatric clinics. These proband children ranged in age from 6 to 17 years. All of the ADHD subjects met full DSM-III-R criteria for ADHD, according to clinical assessment at the time of the referral. Potential subjects were excluded if they had been adopted, if their nuclear family was not available, or if they had major sensorimotor handicaps (paralysis, deafness, or blindness), psychosis, autism, an inability to participate in the assessments because of language barriers, or a estimated IQ
(12) of <80. After receiving a complete description of the study, parents provided written informed consent for their children, and the children and adolescents provided written assent.
A three-stage ascertainment procedure was used to select the study subjects. For the subjects with ADHD, the first stage was the patient’s referral. The second stage included confirmation of the diagnosis of ADHD with a telephone questionnaire administered to the mother. The questionnaire asked about the 14 DSM-III-R symptoms of ADHD and questions regarding study exclusion criteria. The third stage involved confirmation of the diagnosis with face-to-face structured interviews with the mother. Only patients who received a positive diagnosis at all three stages were included in the study.
For the healthy comparison probands, we ascertained participants from referrals to medical clinics for routine physical examinations. In stage 2, the mothers of the healthy comparison subjects responded to the telephone questionnaire. Eligible healthy comparison subjects who met the study entry criteria were recruited for the study and received the third-stage assessment (a structured interview). Only subjects classified as not having ADHD at all three stages were included in the comparison group.
Psychiatric assessments of the probands relied on the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (K-SADS-E)
(13). Diagnoses were based on direct interviews with the mothers and the children. Children <12 years were not interviewed directly. Diagnostic assessments of parents were based on direct interviews with each parent with the Structured Clinical Interview for DSM-III-R (SCID)
(14), supplemented with modules from the K-SADS-E to assess childhood diagnoses in the parents. Not all families were intact at the time of assessment. To obtain assessments on noncustodial parents of nonintact families (always the father), we directly interviewed as many fathers as were available or conducted indirect interviews with the mother. In the latter cases, we collected as much information as the mothers could provide and thoroughly examined the data with the review committee to determine if diagnoses could be assigned. Although only a small proportion of the subjects were affected, we do not have exact data on how many of the fathers from nonintact families were indirectly assessed. However, nearly all of the fathers were assessed, either directly or indirectly—comparison boys: 99% (119 of 120), boys with ADHD: 100% (140 of 140), comparison girls: 95% (116 of 122), and girls with ADHD: 96% (134 of 140). All of the mothers were also directly assessed.
All interviews were conducted blind to the child’s diagnosis and ascertainment site. Diagnoses were considered positive if DSM-III-R criteria were unequivocally met. A committee of board-certified child and adult psychiatrists who were blind to the subject’s ADHD status and all other data resolved diagnostic uncertainties. Diagnoses presented for review were considered positive only if a consensus was achieved that criteria were met to a degree that would be considered clinically meaningful.
All interviewers had undergraduate degrees in psychology and were trained to high levels of interrater reliability. First, they underwent several weeks of classroom-style training: learning interview mechanics, examining diagnostic criteria, and coding algorithms. Then, they observed interviews by experienced raters and clinicians. They subsequently conducted at least six practice (nonstudy) interviews and at least two study interviews while being observed by senior interviewers. The principal investigator (J.B.) supervised the interviewers throughout the study. These same raters performed the telephone screenings for potential probands. Kappa coefficients of agreement
(3) were computed between raters and board-certified psychiatrists who listened to audiotaped interviews made by the raters. On the basis of 173 interviews, the median kappa was 0.86, and kappa was 0.99 for ADHD diagnosis.
Using the methods of Sattler
(15) we estimated IQ from the vocabulary and block design subtests of the Wechsler Intelligence Scales for Children—Revised (WISC-R)
(16) for participants younger than 17 and the Wechsler Adult Intelligence Scales—Revised (WAIS-R)
(17) for subjects older than 17, including the parents. Since the group of boys had been ascertained in the late 1980s, the WISC-R was used instead of more recent versions of the WISC that were not available at the time. We used WISC-R data from the group of girls (ascertained in 1993) in the interest of comparability, even though WISC-III data was available. Again, more recent tests were not used because of the time of data collection for the group of boys. We assessed academic achievement with the arithmetic subtest of the Wide-Range Achievement Test—Revised
(18). Participants from the study of boys with ADHD were administered the Gilmore Oral Reading Test
(19), while participants from the study of girls with ADHD were administered the reading subtest of the Wide Range Achievement Test—Revised
(18). We used the procedure recommended by Reynolds
(20) to define “learning disability.” We first converted the estimated IQ and achievement scores to z scores, z
IQ and z
A, respectively. We then estimated the expected achievement score, z
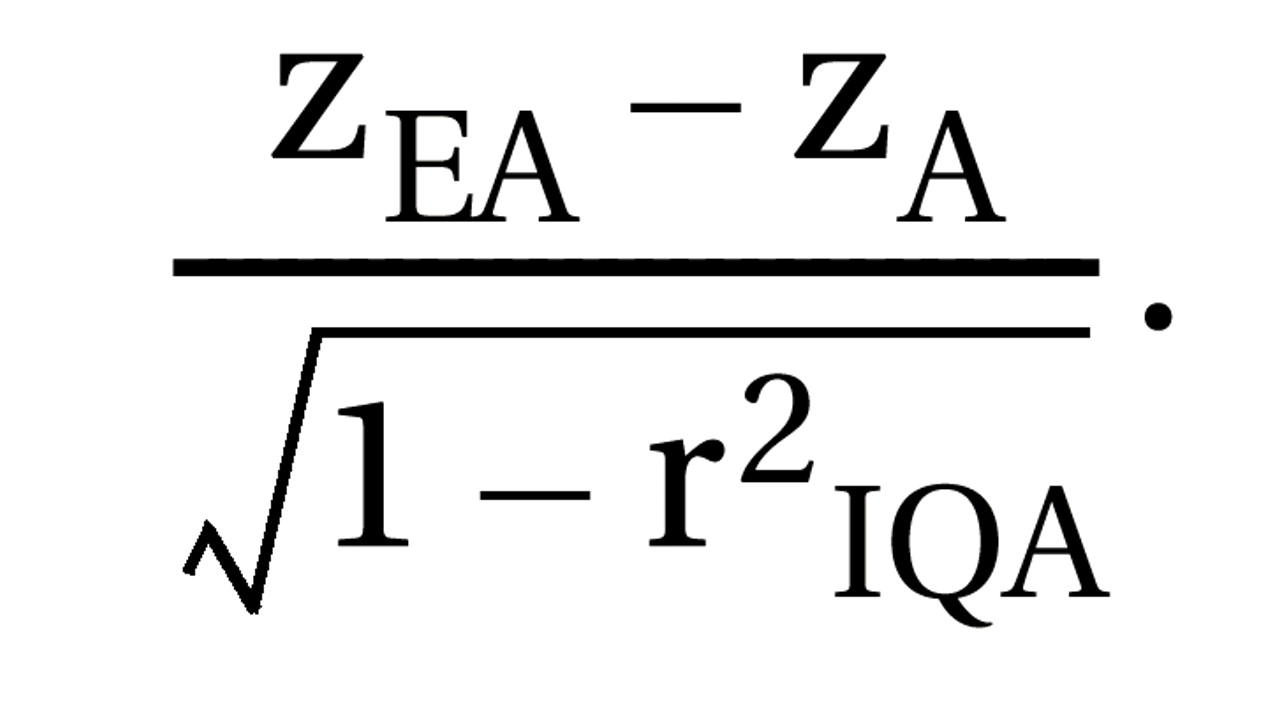
EA, by the regression equation

where r
IQA is the correlation between the IQ and achievement test scores. Then the discrepancy score is z
EA–z
A, and its standard deviation is
We defined as “learning disabled” any subject who had discrepant arithmetic or reading scores based on scoring more than 1.65 on the standardized discrepancy scale:
The interviewers who performed the cognitive testing were the same as those who executed the diagnostic interviews. The training for cognitive assessments was similar to the training methods for the interviewing. First, the interviewers underwent several weeks of classroom-style training. Then they observed cognitive test administration by experienced testers. They subsequently conducted at least six practice (nonstudy) tests and at least two study tests while being observed by senior testers.
Social functioning was assessed with the Social Adjustment Inventory for Children and Adolescents
(12), a semistructured interview schedule that assesses adaptive functioning. As a measure of overall functioning, we used the DSM-III-R Global Assessment of Functioning Scale. Socioeconomic status was measured with the 5-point Hollingshead scale
(21). We used the Moos Family Environment Scale
(22,
23) to assess family environment. The Family Environment Scale has high internal and test-retest reliability and availability of norms and measures the quality of family relationships along three dimensions: 1) cohesion, 2) expressiveness, and 3) conflict. We combined these Family Environment Scale measures to generate a binary indicator of familial conflict. Details of this procedure have been described previously
(7).
As an index of environmental adversity, we used the indicators identified in the work of Rutter et al. as being associated with childhood mental disturbances: severe marital discord, low social class, large family size, paternal criminality, maternal mental disorder, and placement in foster care. Since none of our subjects had been placed in foster homes, the latter variable was not used. Our summary measure of family conflict was used as a proxy for “severe marital discord.” “Low social class” was defined as being in the lowest two socioeconomic classes in our study group (socioeconomic status III and IV). “Large family size” was defined as the families with three or more children. We defined sibships larger than two as being large because two was the modal sibship size. A history of antisocial personality disorder in the father was used to index “paternal criminality,” as measured with the SCID. “Maternal mental disorder” was measured as the mother having had at least two psychiatric disorders during the child’s lifetime. These five variables were summed to create a total index of Rutter’s indicators of adversity. Since only a relatively small number of subjects had all five indicators, we created a collapsed category (≥4) so that the resulting data were categorized as follows: 0, 1, 2, 3, or ≥4 indicators.
Non-ADHD psychopathology was measured as having any history of conduct disorder, major depression with severe impairment, bipolar disorder, or multiple (≥2) anxiety disorders. The relationships between Rutter’s indicators of adversity with learning disability, score on the Global Assessment of Functioning Scale, school problems (defined as a lifetime history of repeating a grade, attending a special class, or receiving extra help), estimated IQ, and social functioning (as measured by total score on the Social Adjustment Inventory for Children and Adolescents) were also examined.
To examine whether the effect of environmental adversity on the risk of ADHD differed by gender, we used logistic regression to model the effect of adversity, gender, and the gender-by-adversity interaction, with ADHD status as the outcome. If the interaction term was significant, that would indicate that the effect of adversity on ADHD differed by gender, prompting us to present results separately for boys and for girls. If the interaction term was not significant, then we would assess the effect of adversity on both genders together, modeling gender as a covariate.
Using the above methods, we also examined the relationship between Rutter’s index of adversity and the following functional outcome measures: school problems, psychiatric comorbidity, social functioning, estimated IQ, score on the Global Assessment of Functioning Scale, and learning disability. As a secondary analysis, we examined each outcome (ADHD status and the six functional outcome measures denoted) in a model with the five environmental adversity factors as independent variables.
Statistical models were fit with the statistical software package STATA
(24). We used generalized estimating-equation models with the logit link and binomial family specification for binary outcomes and the identity link and gaussian family specification for continuous outcomes. All statistical tests were two-tailed. The statistical significance of each covariate in these regression models was determined by Wald’s test, and alpha was set at 0.05.
Results
Associations between demographic features, Rutter’s indicators of adversity, and ADHD risk factors are shown in
Table 1. There was a small but statistically significant difference in age between children with and without ADHD. There was also a significant difference in socioeconomic status between the groups. All of the social adversity indicators were significantly associated with ADHD status, with the exception of large sibship size. Also, as expected, parental history of ADHD and maternal smoking during pregnancy were associated with ADHD status. The overwhelming majority of the study group was Caucasian; there were five Hispanic (1.0%), three Asian (0.6%), and 14 African American (2.7%) participants.
We found no significant interaction between gender and environmental adversity in risk for ADHD (z=–0.1, N=500, p=0.90). Subsequent analyses examined the associations between Rutter’s indicators of adversity and the risk for ADHD, with statistical adjustment for gender, parental history of ADHD, and maternal smoking during pregnancy. The risk for ADHD increased as the number of risk factors increased (relative to the absence of risk) in a dose-dependent fashion. This association attained statistical significance when having one adversity factor was compared to having none (z=2.0, N=500, p=0.04) and continued to show a significantly greater risk with two adversity factors (z=2.2, N=500, p=0.03), three adversity factors (z=4.0, N=500, p<0.01), and four or more adversity factors (z=2.1, N=500, p=0.03). In addition, there was a significant test for a linear trend, with the risk of ADHD increasing as the number of adversity factors increased (z=3.8, N=500, p<0.01).
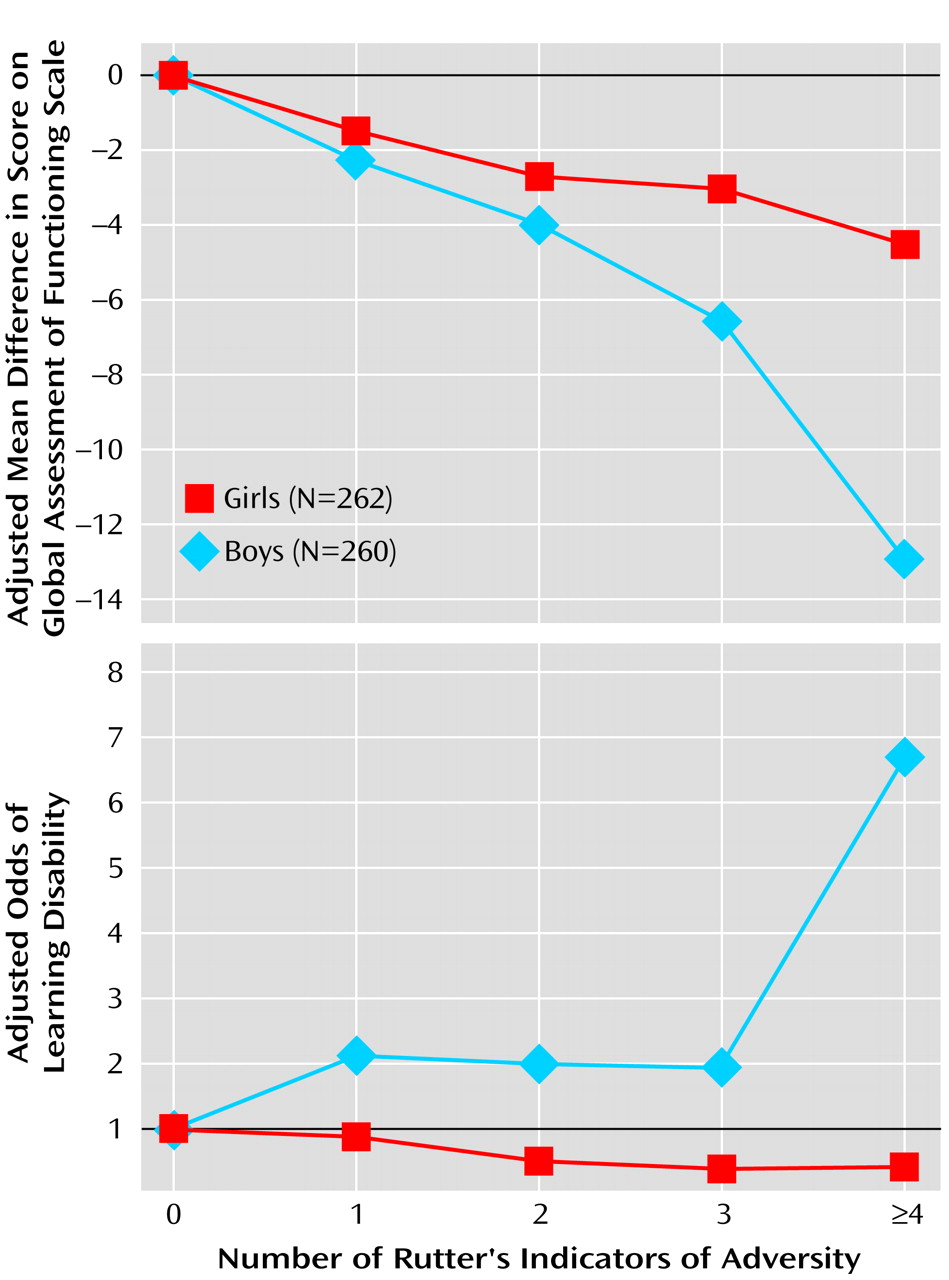
We examined the interactions between Rutter’s indicators of adversity and gender for the functional outcomes listed. These analyses found significant adversity-by-gender interactions for Global Assessment of Functioning Scale score and the risk for learning disability. Specifically, compared to boys with no adversity factors, boys with four or more adversity factors exhibited a 12.9 adjusted mean worsening in score on the Global Assessment of Functioning Scale, but girls demonstrated only a 4.5 adjusted mean worsening. This was a statistically significant effect (beta=–8.43, z=–2.5, N=522, p=0.01). Also, in a test for linear trend, we found that boys suffered a statistically greater decrease (indicating more impairment) in score on the Global Assessment of Functioning Scale than girls as the number of adversity factors increased (z=–2.7, N=522, p=0.007) (
Figure 1).
A similar pattern was observed in the risk for learning disability. Boys with four or more adversity factors exhibited an adjusted odds for learning disability that was 6.6 times the odds for boys with no adversity factors, while girls with four or more adversity factors had an adjusted odds ratio that was only 0.43 times the odds of girls with no adversity factors. This effect was statistically significant (odds ratio=15.3, z=2.0, N=506, p=0.05). In addition, a test for linear trend revealed evidence that boys exhibited a statistically greater increase in learning disabilities than girls as the number of adversity factors increased (z=2.5, N=506, p<0.01) (
Figure 1).
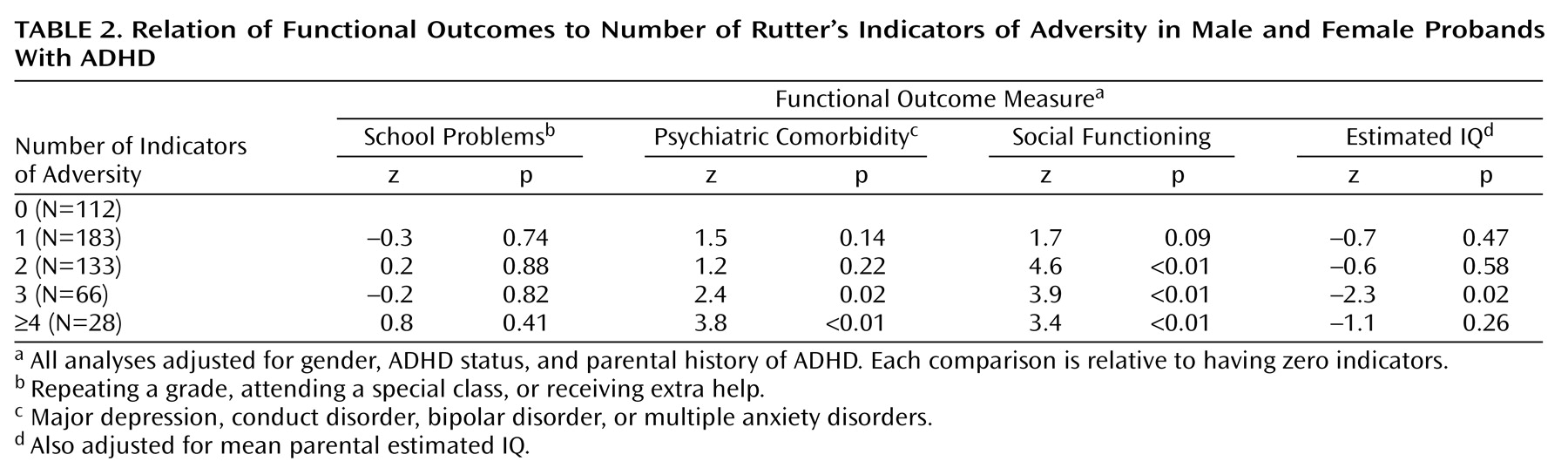
Since we found no statistical evidence for a differential effect of Rutter’s indicators of adversity by gender for the other four functional outcomes assessed (all p>0.05), we ran four additional models, using gender as a covariate. As shown in
Table 2, the rates of psychiatric comorbidity and scores on the Social Adjustment Inventory for Children and Adolescents increased significantly with increasing environmental adversity. Similar findings were observed for IQ, although the comparison of having four or more indicators relative to having none did not attain statistical significance. There was no association between Rutter’s indicators of adversity and school problems.
In an exploratory analysis, we examined the interaction of ADHD status with the indicators of adversity to test the hypothesis that the association between each of our adversity measures and functional outcome may differ by ADHD status. Also, we tested the interactions between age modeled as a binary indicator (6–11 years versus 12–18 years) and the indicators of adversity. However, no statistically significant interaction effect was found for any of the outcomes examined.
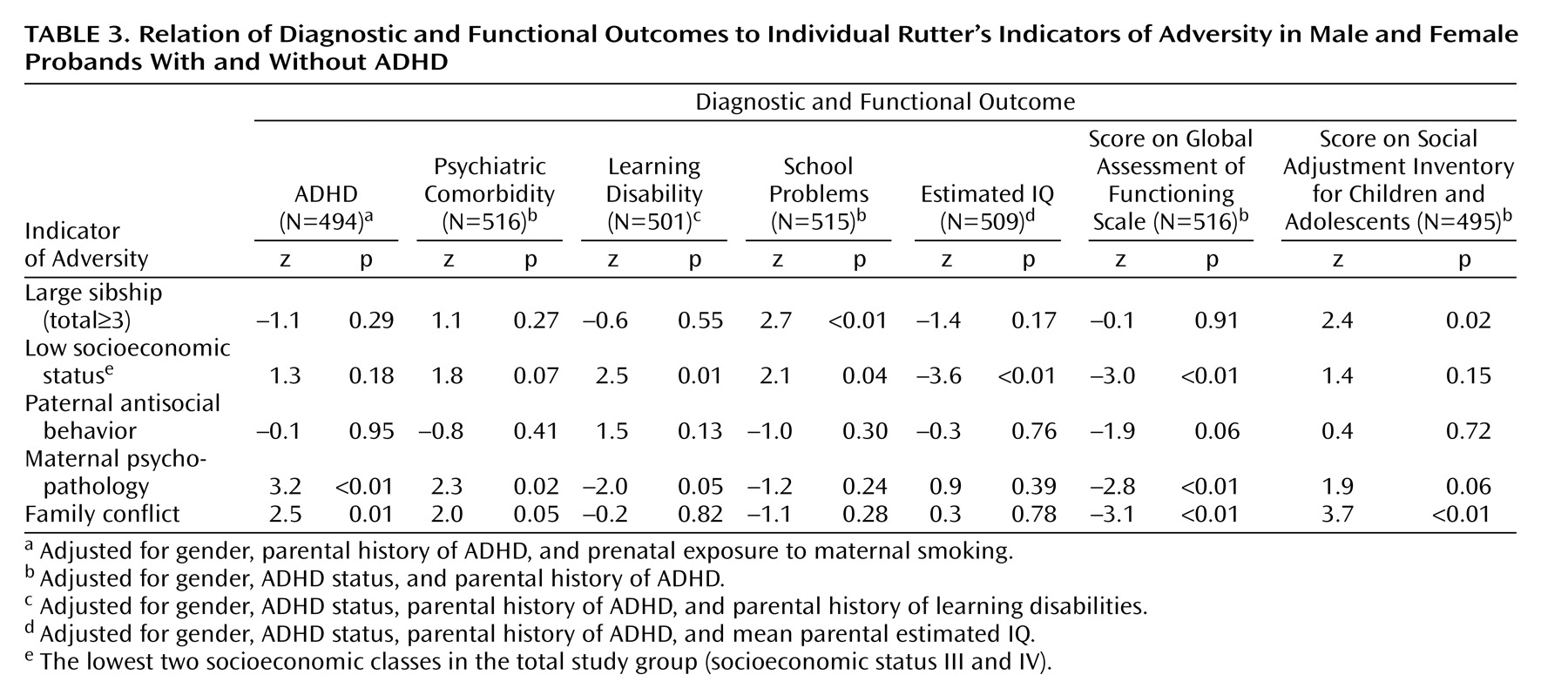
To further clarify the contribution of individual components of Rutter’s indicators of adversity to the risk of ADHD and associated morbidity, we examined the associations between each individual adversity factor and each of the six outcomes under study. As shown in
Table 3, maternal psychopathology and family conflict were significantly associated with both ADHD status and psychiatric comorbidity. In contrast, low socioeconomic status was significantly associated with learning disability, school problems, and IQ. Rates of school problems were also associated with large sibship size, while learning disability was associated with maternal psychopathology. However, this association was in an unexpected direction, with maternal psychopathology being associated with lower rates of learning disability. Maternal psychopathology, family conflict, and low socioeconomic status were all independently associated with more impaired scores on the Global Assessment of Functioning Scale, while large sibship size and family conflict were significantly associated with higher scores on the Social Adjustment Inventory for Children and Adolescents, which reflected more compromised interpersonal functioning.
Discussion
In a large group of children of both genders with and without ADHD, we found Rutter’s indicators of adversity to be significantly associated with the risk for ADHD and several measures of adverse functional outcome, even after control for parental ADHD, maternal smoking during pregnancy, and gender. Although the effect of the cumulative adversity on the risk of ADHD did not differ by gender, the effect of adversity on learning disabilities and impaired scores on the Global Assessment of Functioning Scale was greater for boys than for girls. These findings provide further support for the contribution of adverse psychosocial factors to the risk for ADHD and its associated morbidity and dysfunction.
The present results showing that the association between environmental adversity and risk for ADHD does not differ by gender are concordant with our prior finding of a similar family genetic risk for ADHD for boys and girls
(25). However, since ADHD is less prevalent in girls than in boys, future work will need to examine other risk factors to determine which account for gender differences in the prevalence of ADHD. For example, boys may be more vulnerable than girls to other environmental risk factors that cause ADHD, resulting in an actual higher rate of risk of ADHD in boys. Or factors such as disruptive behavior disorders, symptoms of hyperactivity and impulsivity, and rates of learning disability—which have all been shown to be more prevalent in boys than in girls with ADHD
(26)—may be driving the clinical referral of boys. If so, representative community research designs could reveal a smaller gender discrepancy in the occurrence of ADHD.
Although female gender did not afford protection from the impact of adversity on ADHD risk, it did show a protective effect for global functioning and learning disabilities. Our findings regarding learning disability are consistent with a report from our group
(27) suggesting that girls with ADHD may be less vulnerable to executive deficits in cognitive functioning. If confirmed, our findings suggest different pathways to academic underachievement and cognitive deficits in girls and boys with ADHD.
The finding of a significant negative relationship between maternal psychopathology and offspring learning disability was unexpected and defies an intuitive interpretation. We find it difficult to endorse the notion that a mother’s psychiatric illness is independently protective for learning disability in her children. There are alternate plausible explanations. For example, this could be a type I error, the random false positive result of sampling variability. Second, there could have been residual unmeasured confounding that spuriously induced the relationship.
Although our results show that psychosocial adversity is associated with ADHD risk, it is not possible to separate the effects of genetic and environmental influences on our measures of adversity. That is, the pathogenic genes that make a child susceptible to ADHD can lead to psychopathology in the parents and adversity in the family environment. Indeed, prior work in behavior genetics cautions us from concluding that our measures of adversity are simply measures of environmental influences
(3). For example, twin studies have shown that genes explain a substantial amount of the variance for putative “environmental” measures, such as social support and life stress
(28,
29). Because our family study design cannot disentangle environmental and genetic effects, twin and adoption studies are needed to fully evaluate the relationship between psychosocial adversity and genetics.
Our results must be viewed in light of some limitations in our methods. The groups of boys and girls were ascertained 5 years apart from each other, so cohort effects could be misconstrued as gender effects. While the baseline risk of psychopathology and other functional characteristics examined here could be expected to change with time, the relative effect (odds ratio) in comparison with contemporaneous healthy comparison subjects should remain constant. Thus, with the assumption of no other confounding, a statistically significant interaction could not be due to a cohort effect and may reasonably be attributed to gender. We do not know to what degree our findings will generalize to nonreferred children with ADHD in the community. Previous studies of the family environment have mostly studied either population samples or clinical groups that were not selected for specific disorders. Thus, without further work, our conclusions regarding ADHD and the family environment cannot be generalized beyond the constraints of our study group. An additional source of possible bias stems from the lack of direct interviews with children <12. Although this method may have led to an underrepresentation of psychopathology in this age group, a reanalysis of our data restricting the study group to youth >12 led to similar results.
Despite these considerations, our results suggest that environmental adversity is significantly associated with ADHD and its comorbid impairments and that this effect is moderated by gender for learning disability and global functioning. If future research efforts, particularly twin and adoption studies, concur with our finding that adversity factors have a positive association with impaired outcome in both boys and girls, then a case can be made for developing intervention efforts aimed at reducing them. However, because the specific impact of adversity varies with gender, future research should attend to gender differences in tailoring intervention efforts.

 We defined as “learning disabled” any subject who had discrepant arithmetic or reading scores based on scoring more than 1.65 on the standardized discrepancy scale:
We defined as “learning disabled” any subject who had discrepant arithmetic or reading scores based on scoring more than 1.65 on the standardized discrepancy scale: