An accumulating body of evidence shows that the structural brain abnormalities seen in schizophrenia are likely to be shared by close relatives
(1–
4). Healthy siblings of patients with adult-onset schizophrenia have been reported to have enlarged ventricles
(4,
5), gray matter loss in frontal and temporal regions
(2), and partial reduction in thalamic gray matter volume
(6).
Childhood-onset schizophrenia is a rare and severe form of the illness, and it is continuous with its adult counterpart
(7). Like children with many other early-onset illnesses, children with schizophrenia may provide a homogeneous population with more salient genetic factors than patients with adult-onset schizophrenia
(8). Initial brain magnetic resonance imaging (MRI) scans of patients with childhood-onset schizophrenia show lateral ventricular enlargement and reduction in total, frontal, and parietal cortical gray matter volumes
(9). During adolescence, patients with childhood-onset schizophrenia show progressive ventricular enlargement and a progressive loss of cortical gray matter that follows a back-to-front “wave” pattern
(10–
12).
A study using automated analyses of a large group of patients with childhood-onset schizophrenia (N=57), when divided into young and adult groups, showed a similar pattern of gray matter loss in the parietofrontal direction (Dr. Alexandra Sporn, unpublished data). We hypothesized that, as seen in siblings of patients with adult-onset schizophrenia, siblings of patients with childhood-onset schizophrenia share some of the structural abnormalities seen in the patients and possibly show age-specific patterns of progression.
We present anatomic brain MRI data from a group of healthy siblings of patients with childhood-onset schizophrenia. Since only one scan per subject was available, we compared sibling groups who were 18 years old or younger with those who were older than 18 to look for evidence of back-to-front progression of structural abnormalities.
Method
Fifteen psychiatrically healthy siblings from 15 families of patients with childhood-onset schizophrenia were selected. Ten of the siblings were male, and five were female; their mean age was 19.14 (SD=5.99). Characteristics of the patients with childhood-onset schizophrenia have been described elsewhere
(13,
14). None of the siblings met criteria for axis I or II diagnoses according to interviews with the Schedule for Affective Disorders and Schizophrenia for School-Age Children
(15), the Schedule for Affective Disorders and Schizophrenia
(16), and the Structured Interview for DSM-III Personality Disorders
(17). Thirty-two healthy community volunteers matched for age (p=0.84) and sex (Fisher’s exact p=1) were selected as comparison subjects. Twenty-two of the volunteers were male, and 10 were female; their mean age was 18.75 (SD=6.02).
Anatomic brain MRI scans were obtained with a GE 1.5-T Signa scanner (GE Medical Systems, Milwaukee), and all brain volumes were measured with an automated system
(18). Volumes for the two groups were compared with analysis of variance and corrected for total cerebral volume with analysis of covariance. The NIMH Institutional Review Board approved the project. Written consent (adults) and assent (minor children with parental consent) were obtained for all subjects.
Results
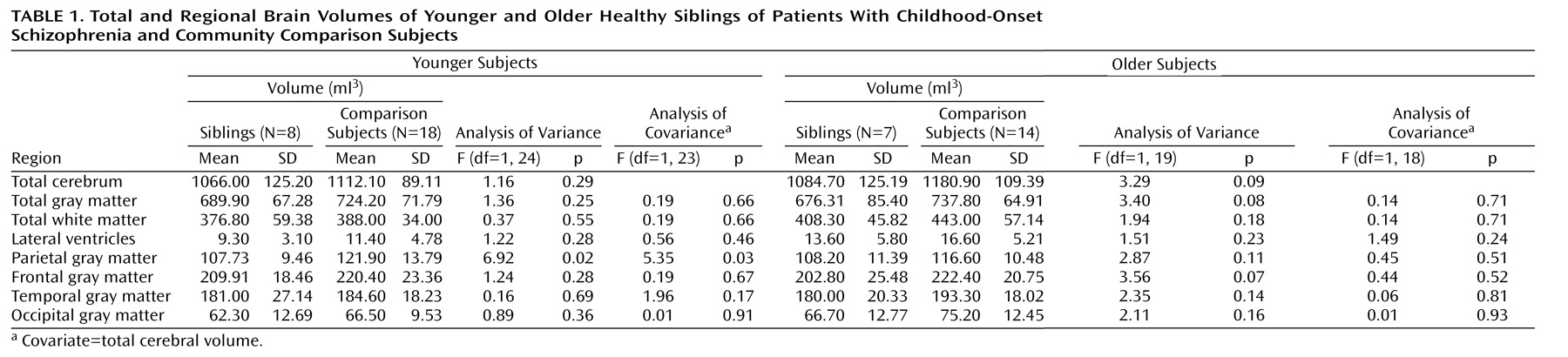
When siblings of patients with childhood-onset schizophrenia and their matched comparison subjects were separated into younger and older groups, younger siblings had significantly smaller parietal gray matter volume with and without adjustment for total cerebral volume (
Table 1). In contrast, in older subjects no differences were evident in parietal gray matter volume, and there was a nonsignificant difference in total cerebral volume and a nonsignificant difference in frontal and total gray matter volumes before adjustments for total cerebral volume (
Table 1). The mean age of the younger group of siblings of patients with childhood-onset schizophrenia was 14.4 (SD=3.3); five were boys and three were girls. The mean age of the younger group of comparison subjects was 14.2 (SD=3.1); 12 were boys and six were girls. The mean age of the older group of siblings of patients with childhood-onset schizophrenia was 24.5 (SD=2.7); five were men and two were women. The mean age of the older group of comparison subjects was 24.6 (SD=2.8); 10 were men and four were women.
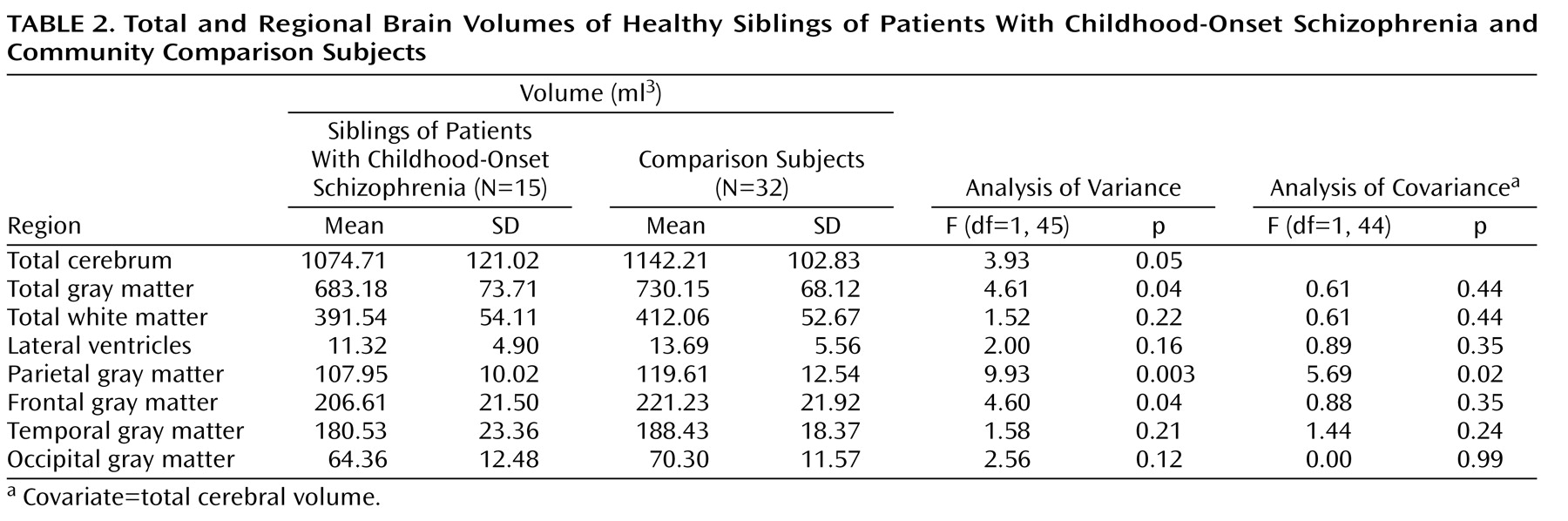
As a group, the siblings of patients with childhood-onset schizophrenia had significantly smaller total cerebral volume and total, parietal, and frontal gray matter volumes than the comparison subjects (
Table 2). After adjustment for total cerebral volume, the difference between groups in parietal gray matter remained significant (
Table 2). There were no significant differences in the lateral ventricular or white matter volumes.
Discussion
To our knowledge, this is the first study to examine brain MRI abnormalities in siblings of patients with childhood-onset schizophrenia. This study shows that healthy siblings of childhood-onset schizophrenia probands have smaller total and parietal gray matter volumes than normal comparison subjects. The parietal gray matter finding survived covariance for total cerebral volume. As with patients with childhood-onset schizophrenia, there was no difference between siblings and comparison subjects in the white matter volume. However, unlike patients, no ventricular enlargement was seen in the siblings. When divided into young and old siblings, younger siblings had smaller parietal gray matter volume and older siblings showed trends for total cerebral volume and frontal and total gray matter volume loss. This may suggest that the structural brain abnormalities in siblings of patients with childhood-onset schizophrenia may follow a similar back-to-front wave (parietofrontal) pattern as in the patients. However, a major caveat for our findings is the low power due to the small number of subjects in the study, especially after dividing the siblings into two age groups.
The current findings indicate that in families with a member who has schizophrenia, familial or genetic factors may contribute to shared structural brain abnormalities, and that these abnormalities could be genetic trait markers. Continued sibling accrual with prospective rescans is ongoing at the National Institute of Mental Health to validate and extend these findings.