This study explored the phenomenology of psychiatric symptoms in the nursing home in an effort to help inform treatment strategies. Among geriatric psychiatrists, there is increasing awareness of the need for multimodal interventions for the elderly that are aimed at minimizing functional impairment and enhancing quality of life across multiple sources of disability
(1,
2). This multimodal approach contrasts with the typical method of employing psychotropic medications, i.e., targeting discrete psychiatric syndromes with specific medications. Discrete syndromes are difficult if not impossible to identify in the nursing home, since symptoms tend to overlap across disorders, and cognitive decline often complicates the clinical picture.
Particularly among the oldest-old, the cumulative burden of psychiatric symptoms and cognitive decline tends to manifest as a loss of social functioning. Even in the absence of overt dementia, functional impairment may be precipitated by the entire spectrum of age-associated cognitive and emotional changes. For example, mild cognitive impairment
(3) has been associated with psychiatric disturbances such as depression, and the presence of depression has been suggested to be predictive of future cognitive and functional decline
(4–
6).
In an effort to sort out these complexities, we systematically assessed nursing home subjects to determine which symptoms impinged most significantly on daily functioning across the full spectrum of psychiatric symptom severity. Previous work has supported deleterious effects of cognitive impairment, psychosis, and agitation on daily functioning among dementia patients
(7,
8). This study is unique in its use of cognitive status as a continuous rather than categorical measure and its focus on the nursing home setting. The nursing home patient has not yet been fully characterized across all levels of psychiatric symptoms and cognitive function. Having reached 1.6 million individuals in 1999, the long-term care population is quite literally growing in importance
(9).
Method
Subjects were approached for enrollment if they were over age 60 and were long-term residents. The presence of schizophrenia, bipolar disorder, or mental retardation was exclusionary. Subjects (N=69) were enrolled if they could participate in the consenting process or had a surrogate decision-maker willing to provide consent. Among those not enrolled, approximately 20 residents were unable to cooperate because of aphasia or profound dementia, and an additional 15 needed a surrogate decision-maker and no such person was available. Consenting subjects (N=46) and legal surrogates (N=23) signed written consent after a verbal discussion of study procedures. Subjects with surrogates provided verbal assent. Data were collected by a research assistant with established reliability through training with the Iowa Mental Health Clinical Research Center.
Assessments included the clinical dementia rating from the Mattis Dementia Rating Scale
(10) and Folstein’s Mini-Mental State Examination (MMSE)
(11). Depression severity was determined by the sum of the depression items (e.g., depressed mood, difficulty sleeping, appetite change) from the Columbia University Scale for Psychopathology in Alzheimer’s Disease
(12). Similarly, the delusion score was the sum of delusion ratings (e.g., unusual beliefs, delusions of infidelity, suspiciousness, delusions of abandonment or a plotting caregiver, somatic delusions, and perceiving intruders, impostors, and other false beliefs). Behavioral disturbance was quantified as the sum of the following items: wandering, verbal outbursts, physically threatening behavior or physical violence, agitation, restlessness, and nighttime confusion.
Daily living skills were assessed with the Social-Adaptive Functioning Evaluation
(13), in which a higher score reflects greater impairment. This scale measures 17 social-interpersonal, basic, and instrumental daily life skills on a 0–4 scale. Items include bathing, dressing, feeding, neatness, mobility, communication, conversational skills, instrumental social skills, social appropriateness, friendships, recreation, and participation in activities.
Data were recorded through a Microsoft Access database program and transferred to JMP statistical software for further analysis. Data were nonnormally distributed and therefore rank transformed before all analyses. A correlation analysis examined the zero-order correlations between symptoms, cognitive function, and daily living skills. Standard least squares regression was employed to examine the relative effects of psychiatric symptoms and cognitive function on the dependent measure of daily living skills, i.e., the symptom ratings were grouped into three categories (depression, delusions, and behavioral symptoms) and along with cognitive function were employed as independent measures in a regression model with the Social-Adaptive Functioning Evaluation score as the dependent measure.
Results
Sixty-nine subjects (54 women and 15 men) participated. The mean age was 86.7 years (SD=7.9, range=62–101). The subjects had a mean education level of 12.9 years (SD=2.9), mean MMSE score of 19.5 (SD=8.0), and a mean Clinical Dementia Rating score of 1.25 (SD=0.9). The mean Mattis Dementia Rating Scale was 90.7 (SD=34.9), and the mean Social-Adaptive Functioning Evaluation score was 26.4 (SD=16.3). From the Columbia University Scale for Psychopathology in Alzheimer’s Disease items, the subjects had mean psychiatric symptom ratings of 3.3 (SD=2.7, range=0–10) for depressive symptoms, 1.6 (SD=1.9, range=0–6) for delusional symptoms, and 2.1 (SD=2.1, range=0–6) for behavioral disturbance symptoms. Thirty-eight percent (N=26) of the subjects were receiving antipsychotic medication, 28% (N=19) were receiving anxiolytics, and 35% (N=24) were receiving antidepressants. Among all persons receiving psychotropics, three participants were receiving three or more agents, 18 were receiving two, and 16 were receiving one medication.
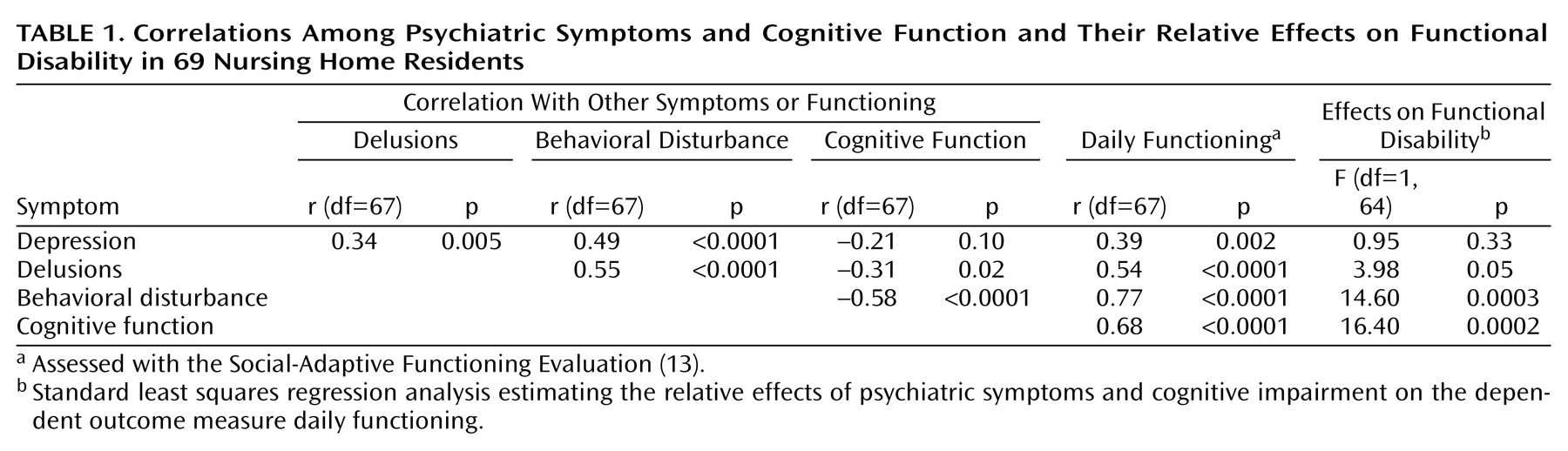
In the pairwise correlation analysis, impairment in social-adaptive functioning was most highly correlated with behavioral disturbance (r=0.77) followed by cognitive impairment (r=0.68) (
Table 1). A standard least squares model was performed, with the ranked values from the Mattis Dementia Rating Scale and psychiatric ratings entered as independent variables to determine their effects on the dependent measure of Social-Adaptive Functioning Evaluation ratings. The overall model suggested significant effects (F=34.9, df=4, 64, p<0.0001). Individual effects are reported in
Table 1.
Discussion
Cognitive decline was most highly associated with impairment in daily functioning in the nursing home setting after we accounted for the effects of depression, delusions, and behavioral disturbance. Among psychiatric symptoms, only behavioral disturbances were significantly associated with impaired functioning after we controlled for cognitive effects. This suggests that treatment strategies that may enhance cognitive status or improve behavioral dysregulation may be of greatest benefit for this population.
Cognitive function may be modestly enhanced by current pharmacologic approaches such as cholinesterase inhibitors. However, a comprehensive approach that includes optimizing nutrition, hydration, and pain control among other strategies will likely have the greatest positive effects on both cognition and behavior. This type of multimodal approach is likely the best suited for the interrelated nature of symptoms and function in this population, yet it is at times difficult to reconcile with pharmacologic trials designed for unitary syndromes.
Late-life behavioral disturbances in particular have defied categorization as a unitary phenomenon. Commendably, Harwood et al.
(14) employed factor analyses to discern behavioral subtypes in dementia. Five factors were reported: agitation/anxiety, psychosis, aggression, depression, and activity disturbance. This group also evaluated which symptoms were associated with the greatest degree of functional impairment after cognition was controlled. They noted that activity disturbances, diurnal disturbances, delusions, and hallucinations most significantly impaired the performance of important self-maintenance activities
(15).
We can conclude from our findings that treatable syndromes in the nursing home may be particularly difficult to decipher given the high degree of symptom intercorrelation. The influence of cognitive decline and behavioral dysregulation on daily functioning further complicates the treatment scenario. Multimodal intervention strategies with functional impairment as the outcome measure of interest may be of greatest benefit for the nursing home resident.