Refining Personality Disorder Diagnosis: Integrating Science and Practice
Abstract
Why Revise Axis II?
Overview and Goals
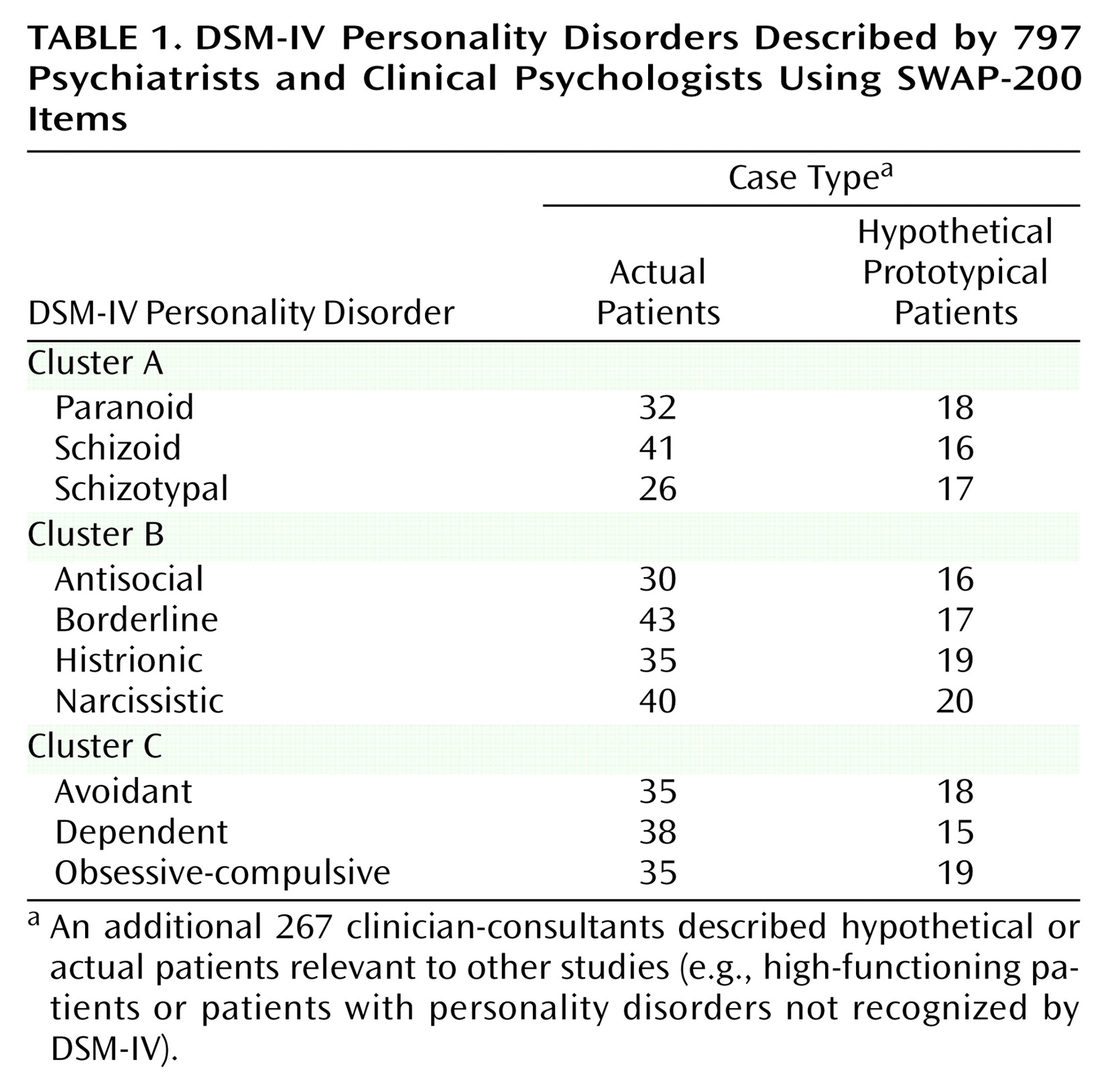
Method
Clinician-Consultants
The SWAP-200: Quantifying Clinical Observation
Identifying Core Features of Personality
Procedures
We are asking you to use the SWAP-200 to describe a hypothetical patient with histrionic personality disorder. We do not want you to describe a real patient. Rather, we are interested in learning what the term “histrionic personality disorder” connotes for you. We would like you to describe a prototypical histrionic patient, a hypothetical person who illustrates histrionic personality disorder in its purest form.
Results
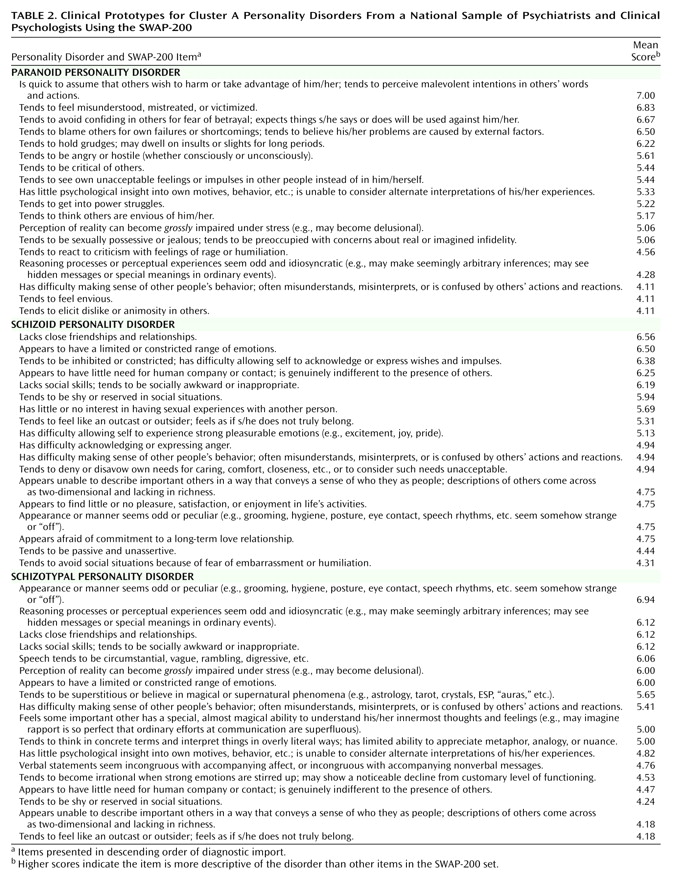
Clinician Conceptions of Cluster A Personality Disorders—The “Odd” Cluster
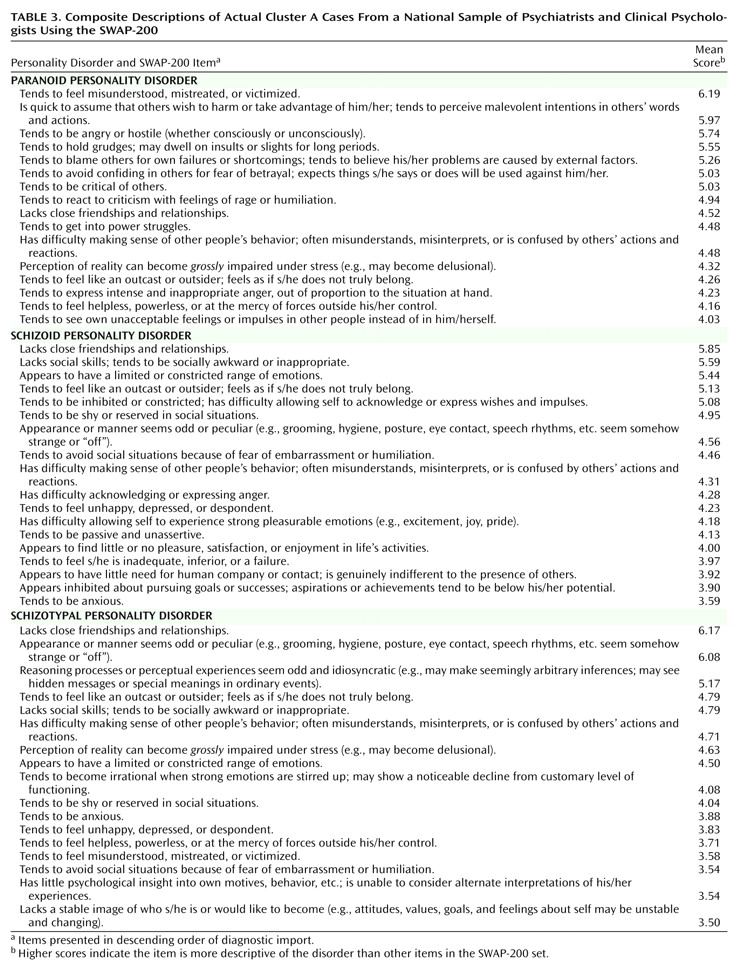
Empirically Observable Features of Cluster A Personality Disorders
Paranoid personality disorder
Schizoid and schizotypal personality disorders
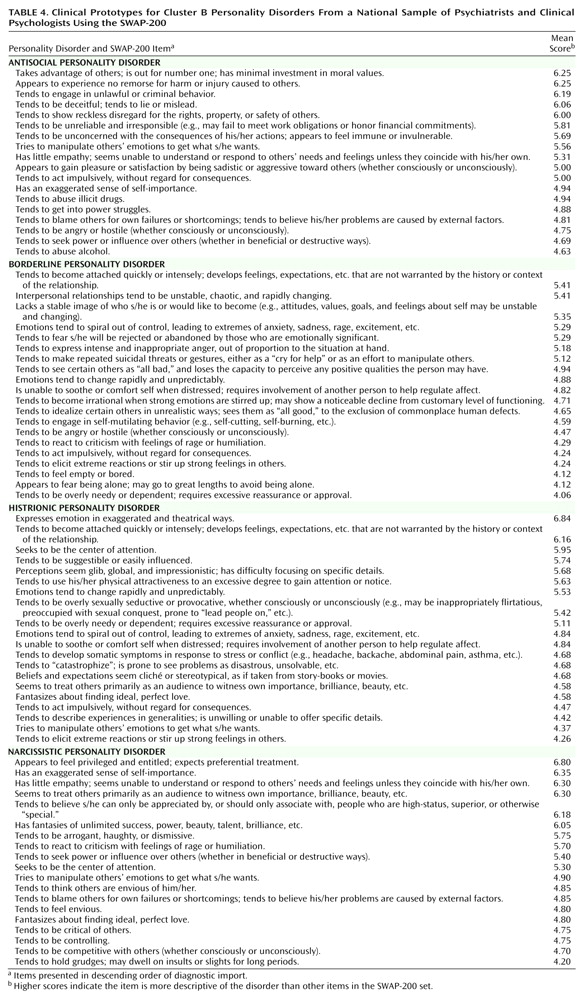
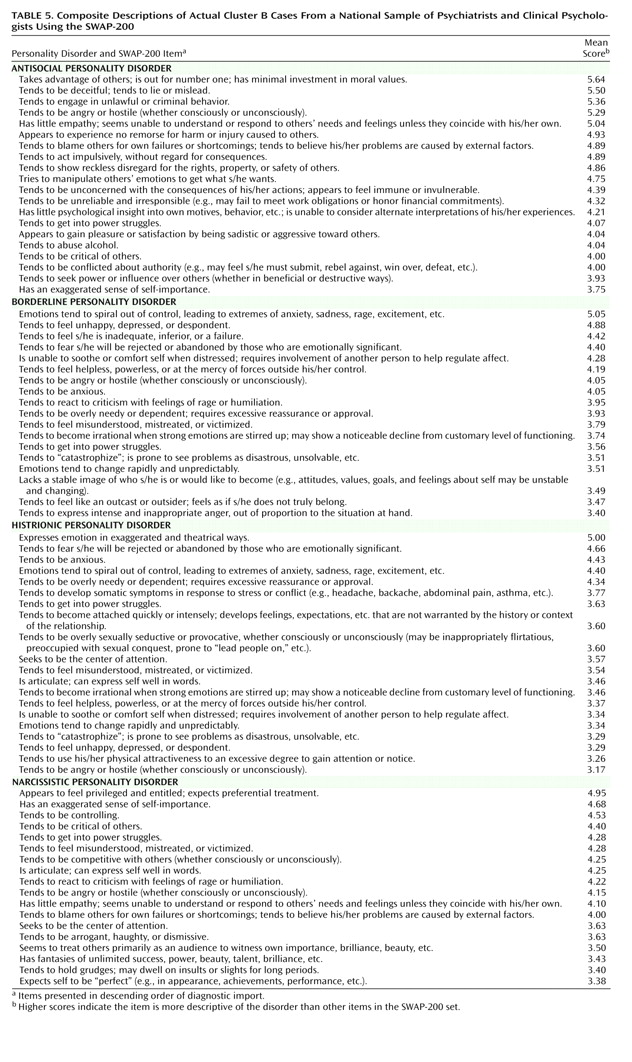
Clinician Conceptions of Cluster B Personality Disorders—The “Dramatic” Cluster
Empirically Observable Characteristics of Cluster B Personality Disorders
Antisocial personality disorder
Borderline personality disorder
Histrionic personality disorder
Narcissistic personality disorder
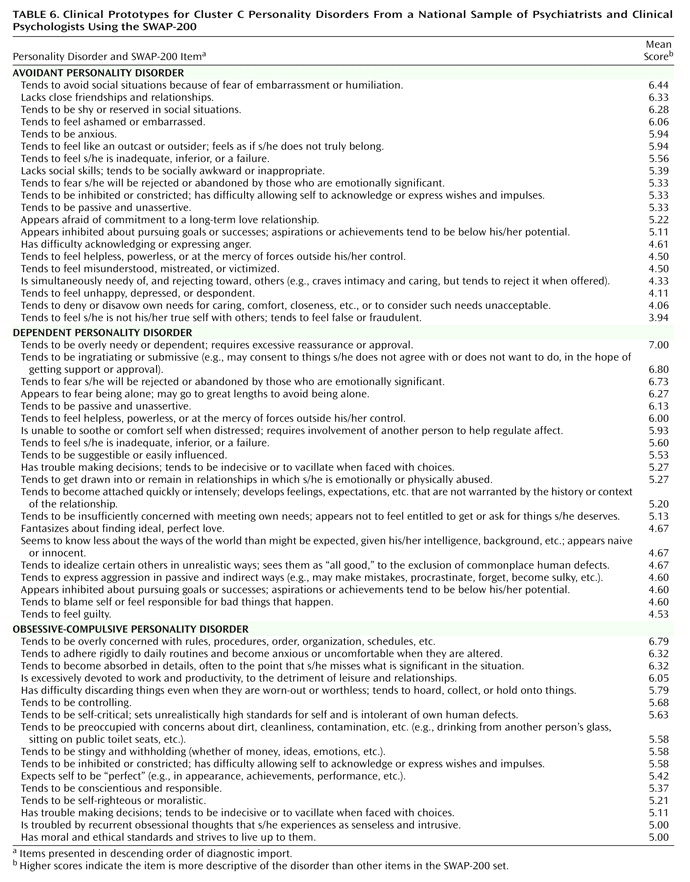
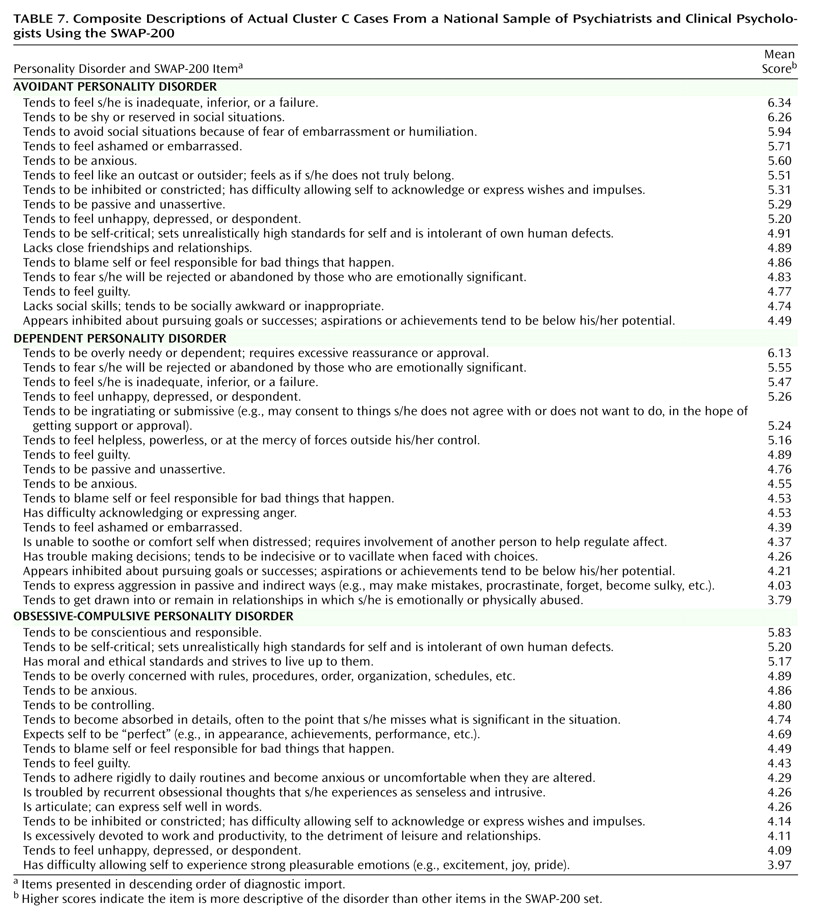
Clinician Conceptions of Cluster C Personality Disorders—The “Anxious” Cluster
Empirically Observable Characteristics of Cluster C Personality Disorders
Avoidant and dependent personality disorders
Obsessive-compulsive personality disorder
Discussion
Advantages of Expanded Criterion Sets
Addressing Inner Experience
Identifying Distinct Diagnoses
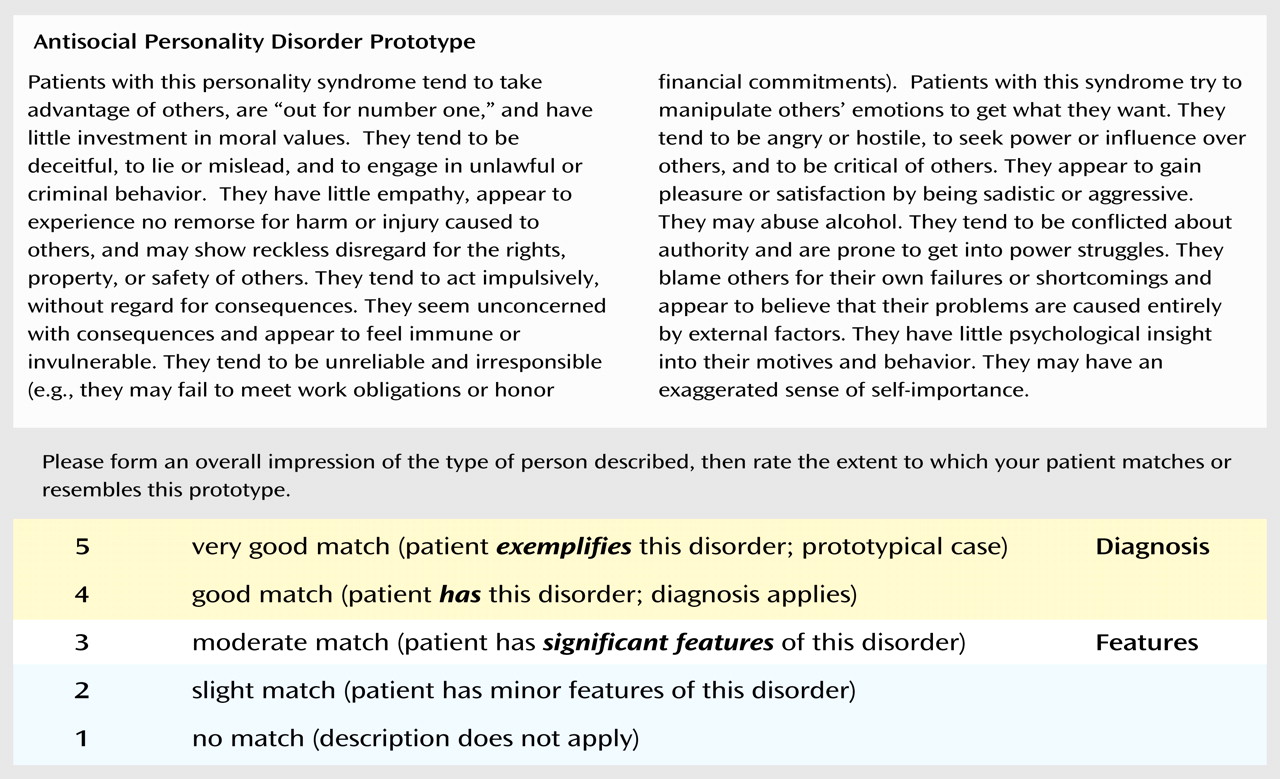
A Prototype Matching Approach to Diagnosis
Limitations
Conclusions
Footnote
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

