The Sept. 11, 2001, terrorist attacks increased interest in treatments for posttraumatic stress disorder (PTSD). Most efficacious psychotherapies for PTSD are exposure-based
(1). Yet experts acknowledge that direct reexposure to reminders of traumatic events frightens many traumatized patients and deters them from treatment. Non-exposure-based PTSD treatments might be welcome alternatives. Interpersonal psychotherapy, a time-limited, diagnosis-targeted treatment, focuses on current social and interpersonal functioning rather than exposure. Interpersonal psychotherapy has demonstrated efficacy for mood disorders and has recently been adapted for anxiety disorders
(2–
4).
Interpersonal psychotherapy is a life-event-based treatment, and PTSD is a life-event-based disorder. Patients with PTSD manifest significant interpersonal difficulties, depressive symptoms, and affect dysregulation—all problems that interpersonal psychotherapy has been shown to alleviate. Interpersonal difficulties associated with PTSD include difficulty trusting others, low self-esteem, problems establishing boundaries, and fears of intimacy and of vulnerability in social interactions. Interpersonal psychotherapists encourage patients to focus on current life events and their relationship to mood and help patients make interpersonal changes that provide a renewed sense of mastery over their present situations while reducing PTSD symptoms. The medical model of interpersonal psychotherapy that employs defining PTSD as a medical illness may help patients relinquish guilty self-blame for their symptoms. The authors hypothesized that solving current interpersonal problems in interpersonal psychotherapy would yield generalized symptomatic improvement for PTSD subjects even in the absence of exposure techniques.
Method
Subjects with a primary DSM-IV diagnosis of PTSD were recruited by clinical referral and local advertising and signed written informed consent. Exclusion criteria were substance abuse/dependence in the past 6 months, history of psychotic symptoms, unstable medical conditions, and concurrent psychotherapy. Of approximately 100 telephone-screened callers, 25 were eligible for study evaluation. Evaluation for study entry used the Structured Clinical Interview for DSM-IV for Axis I Diagnoses, Patient Edition (SCID), the Structured Clinical Interview for DSM-IV for Axis II Diagnoses (SCID-II)
(5), and the Clinician-Administered PTSD Scale
(6) to assess lifetime and current DSM-IV PTSD symptoms and associated features. All 14 subjects meeting study inclusion criteria enrolled.
Outcome measures administered at baseline, mid-treatment, and the end of treatment were the 17-item total Clinician Administered PTSD Scale; the 24-item Hamilton Depression Rating Scale; the Posttraumatic Stress Scale—Self-Report Version
(7), a 17-item scale of frequency and severity of each DSM-IV PTSD symptom; the Beck Depression Inventory; the State-Trait Anger Experience Inventory
(8), a 44-item questionnaire measuring anger expression and experience; and the Social Adjustment Scale—Self-Report Version
(9), a 54-item questionnaire. Trained, experienced raters administered the SCID, the SCID-II, the Hamilton depression scale, and the Clinician Administered PTSD Scale.
The subjects were treated for 14 weeks with a protocol approved by an institutional review board by K.L.B. (N=11) or J.C.M. (N=3), research-certified interpersonal psychotherapists experienced in outcome studies and in treating PTSD. The subjects received up to two sessions the first week and one session weekly for the following 13 weeks. The median number of sessions was 14 (interquartile range=12–14). Interpersonal psychotherapy was easily adapted for treating PTSD. Therapy focused on the interpersonal sequelae of trauma, such as interpersonal hypervigilance, difficulty trusting and confronting others, and the manner in which PTSD symptoms, such as avoiding reminders of the trauma, interfere with current functioning and relationships. The goal was to decrease symptoms by improving social functioning.
Following the medical model, the therapist provided psychoeducation about PTSD symptoms and the impact of symptoms and trauma on social functioning, linked life events to mood changes, and helped the patient identify a focal problem area for treatment. The patient’s PTSD was often framed as a role transition—a process of recovering from trauma and transition to regaining the interpersonal functioning the trauma had fractured—or as a current conflict with a significant other (role dispute) precipitated or exacerbated by traumatic symptoms. PTSD’s traumatic event eliminates the troublesome, non-life-event interpersonal psychotherapy focal category of interpersonal deficits
(3). Focusing on current issues helps traumatized patients concentrate on the present and future and fosters a sense of mastery over the environment.
Response to treatment was determined with the Wilcoxon paired rank sum test to compare subjects’ symptoms before and after treatment. Within-group effect sizes (Cohen’s d) were calculated for each Wilcoxon test. Large effect sizes were defined as ≥0.80
(10). Analyses used the method of last observation carried forward.
Results
Eleven women and three men of a mean age of 33.1 years (SD=9.0, range=19–45) were treated between August 2000 and June 2003. Seven subjects were white, four were African American, two were Asian, and one was Hispanic. Eight were single, three were married or cohabitating, two were divorced, and one was separated. Precipitating traumas ranged from childhood sexual and physical abuse to armed mugging or rape in adulthood. The mean duration of PTSD symptoms was 7.6 years (SD=9.5, median=1.4, range=3 months–25 years). The mean baseline Clinician-Administered PTSD Scale score was 66.9 (SD=14.9), falling within the severe range for PTSD
(6). Eight subjects met the criteria for secondary diagnoses of major depression, seven for past cannabis and/or alcohol abuse, and three for axis II disorders: one apiece for avoidant, depressive, and obsessive-compulsive. No subjects were taking medication or had known antidepressant resistance.
Treatment response was defined as a ≥50% decrease in score on the Clinician-Administered PTSD Scale, a relatively stringent threshold for PTSD research. Remission was defined as a Clinician-Administered PTSD Scale score of ≤20, based on Davidson’s survey using a Clinician-Administered PTSD Scale-like instrument, which found that scores ≤20 in the general community were associated with negligible PTSD psychopathology
(11).
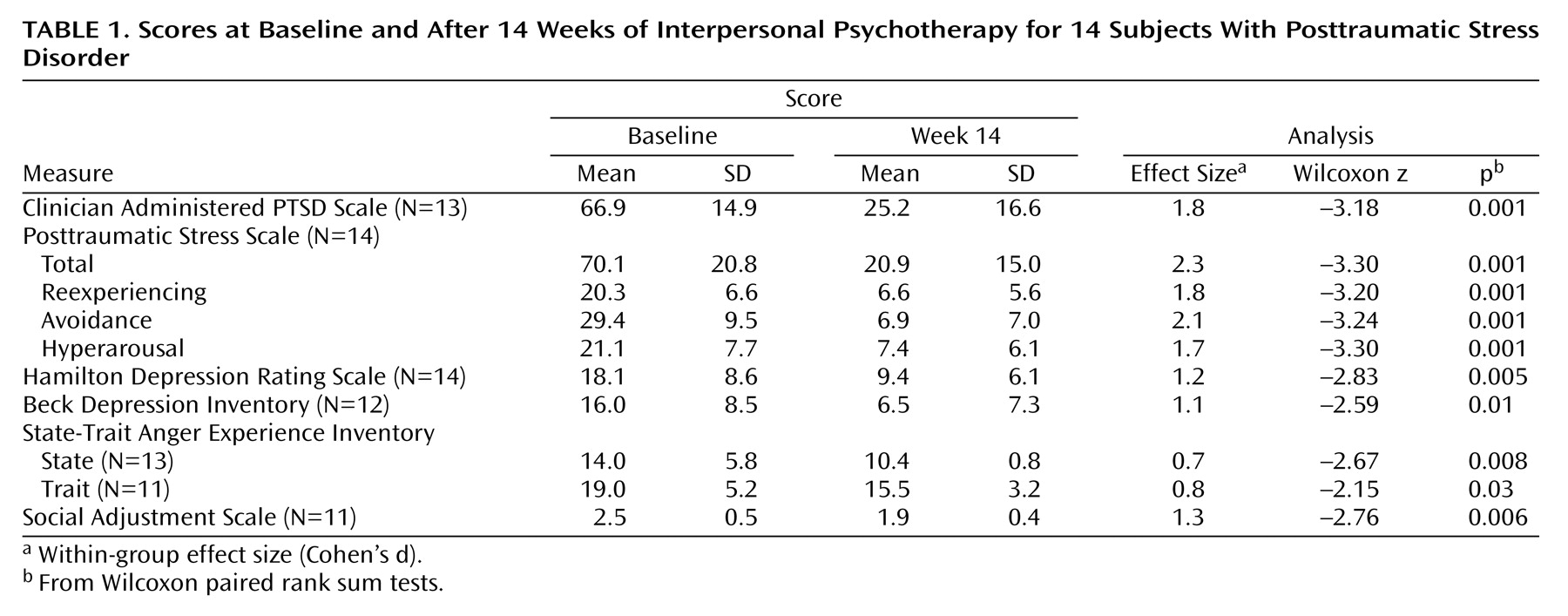
Treatment was well tolerated. Thirteen of 14 subjects completed 14 weeks of treatment. The one dropout came after 13 weeks. At termination, 12 of 13 subjects rated no longer met diagnostic criteria for PTSD on the Clinician-Administered PTSD Scale. Fourteen subjects reported declines in PTSD symptoms across all three symptom clusters (all p≤0.001) on the Posttraumatic Stress Scale, with large effect sizes (
Table 1). Response (50% improvement on the Clinician-Administered PTSD Scale) was 69%, and remission (Clinician Administered PTSD Scale score ≤20) was 38%. Depressive symptoms improved on the Hamilton depression scale and the Beck Depression Inventory, as did anger reactions measured by the State-Trait Anger Experience Inventory. Nine of 11 subjects reported improved interpersonal functioning on the Social Adjustment Scale.
Discussion
These pilot results suggest that focusing on one aspect of PTSD—interpersonal difficulties—may yield generalized improvement across symptom clusters and that PTSD may improve without focused reexposure to past trauma
(12). Interpersonal psychotherapy showed excellent retention and high response and remission rates. Interpersonal psychotherapy may help patients who have developed PTSD but refuse exposure-based treatment or pharmacotherapy. Some subjects reported that unprompted and after their interpersonal functioning and symptoms had improved, they spontaneously exposed themselves to reminders of the trauma they had been avoiding. Improved interpersonal functioning and symptom relief may motivate patient self-exposure to further master the trauma.
Although the results are promising, the several limitations to this open study include a small group size, heterogeneity of the traumas, the use of only two therapists, the lack of a comparison/control group, rater blindness to treatment (albeit self-report Posttraumatic Stress Scale scores mirrored scores on the Clinician-Administered PTSD Scale, as the Beck Depression Inventory scores did the Hamilton depression scale scores), and formal treatment-adherence monitoring. This group of PTSD patients may have had a better prognosis than others who abuse substances or take medication.
The limitations of interpersonal psychotherapy for PTSD are not yet known. This study yielded a treatment manual that will be used in a controlled trial. Follow-up of the 14 subjects is ongoing.