Recent events have focused the world’s attention on the psychological effects of terrorism. Elevated rates of posttraumatic stress disorder (PTSD) symptoms have been found in the aftermath of major terrorist attacks in the United States
(1–
3). These symptoms tend to subside with time
(4), but a significant minority of those initially affected may develop chronic PTSD. The prevalence of PTSD among survivors of terrorist attacks and the rate in which the acute response to terrorist acts subsides with time have not been evaluated in controlled studies. With the current surge of terrorism, such knowledge is pertinent for clinicians and service planners.
DSM-IV-TR asserts that PTSD may be especially severe or long lasting when the stressor is of human design (p. 464). A meta-analysis of risk factors for PTSD
(5) further suggested that stressors occurring at the aftermath of traumatic events contribute to the occurrence of the disorder. Repeated acts of terror are associated with significant distress in affected communities (e.g., references
1,
2,
6) and thereby might interfere with the recovery from early PTSD symptoms and lead to a higher incidence of PTSD.
This work prospectively evaluates the incidence of PTSD in direct survivors of terrorist attacks, comparing them with survivors of motor vehicle accidents. It also compares the progressive attenuation of early PTSD symptoms during a period of continuous terror threat with that seen during years of sporadic terrorism. We hypothesized that 1) terrorist acts generate higher rates of PTSD, 2) a smaller decline in early PTSD symptoms will contribute to a higher prevalence of the disorder among survivors of terrorist attacks, and 3) the decline in early symptoms will be smaller during an era of frequent terrorism.
Method
Data for this study were collected among survivors of traumatic events that met DSM-IV PTSD criterion A and were admitted to a general hospital emergency room in Jerusalem between April 1996 and March 2002 (N=426). Within these boundaries, the period between April 1996 and October 2000 was characterized by sporadic acts of terror, as exemplified by an annual national average of 42 civilian fatalities from terrorist attacks (an annual population rate of 0.65 per 100,000). We refer to this period as one of infrequent terrorist acts.
In contrast, the period between October 2000 and March 2002 involved frequent terrorist attacks that caused 297 civilian fatalities in 2002 (a population rate of 4.56 per 100,000 per year), of which 77 occurred in the single month of March 2002. Suicide bombs became the deadliest weapon, causing 60% of all civilian deaths. Suicide bombs induce unparalleled horror by exposing survivors, rescuers, and witnesses to body parts and grotesque scenes of death and destruction. We refer to this period as one of frequent terrorist acts.
The data presented here come from an ongoing prospective study of physiological and biological predictors of PTSD. The parent study’s design has been described in previous publications (e.g., references
7–
9). Briefly, consecutive survivors of traumatic events were recruited during or shortly after their admission to a general hospital emergency room after trauma. Continuous measures of PTSD, peritraumatic dissociation, depression, and anxiety symptoms were collected 1 week and 4 months after the traumatic event. The Impact of Event Scale
(10), the Beck Depression Inventory
(11), and the State-Trait Anxiety Inventory by Spielberger et al.
(12) conferred continuous measures of PTSD symptoms, depression, and anxiety. The Peritraumatic Dissociative Experiences Questionnaire—Self Report
(13) evaluated the occurrence of dissociation during the traumatic event. Additionally, heart rate upon admission to the emergency room was measured in 272 survivors. Survivors with and without heart rate data had a similar age, gender distribution, and levels of symptoms at 1 week and 4 months. The Clinician-Administered PTSD Scale
(14) conferred a diagnosis of PTSD at 4 months. Each of the study’s participants signed an informed consent form after receiving detailed information about the study. Hadassah University Hospital’s institutional review board approved and monitored the study.
Thirty-nine of the study’s 426 participants were exposed to terrorist acts, 354 had motor vehicle accidents, and 33 had other traumatic events (domestic accidents [N=14], rape [N=2], assault [N=4], and work/sport accidents [N=13]). Survivors of terrorist acts were mostly victims of suicide bomb attacks on buses and public places in Jerusalem. Motor vehicle accidents comprised severe accidents involving life threats, injury, or death. To reduce the heterogeneity of traumatic events, we compared 39 survivors of terrorist attacks with 354 survivors of motor vehicle accidents (23 and 224, respectively, with measurements of heart rate in the emergency room). A comparison of terror survivors (N=39) with all other participants (N=387) yielded similar results.
Seven survivors of motor vehicle accidents (2%) had prior (lifetime) exposure to terrorist acts. Six survivors of terrorist acts (15.4%) reported previous exposure to motor vehicle accidents. Other lifetime traumatic events among motor vehicle accident survivors included work/other accidents (N=7), sexual assault, and rape (N=2). Lifetime exposure to traumatic events among survivors of terrorism included domestic violence (N=2) and work/other accidents (N=1).
Results
Terrorist Attacks and Motor Vehicle Accidents
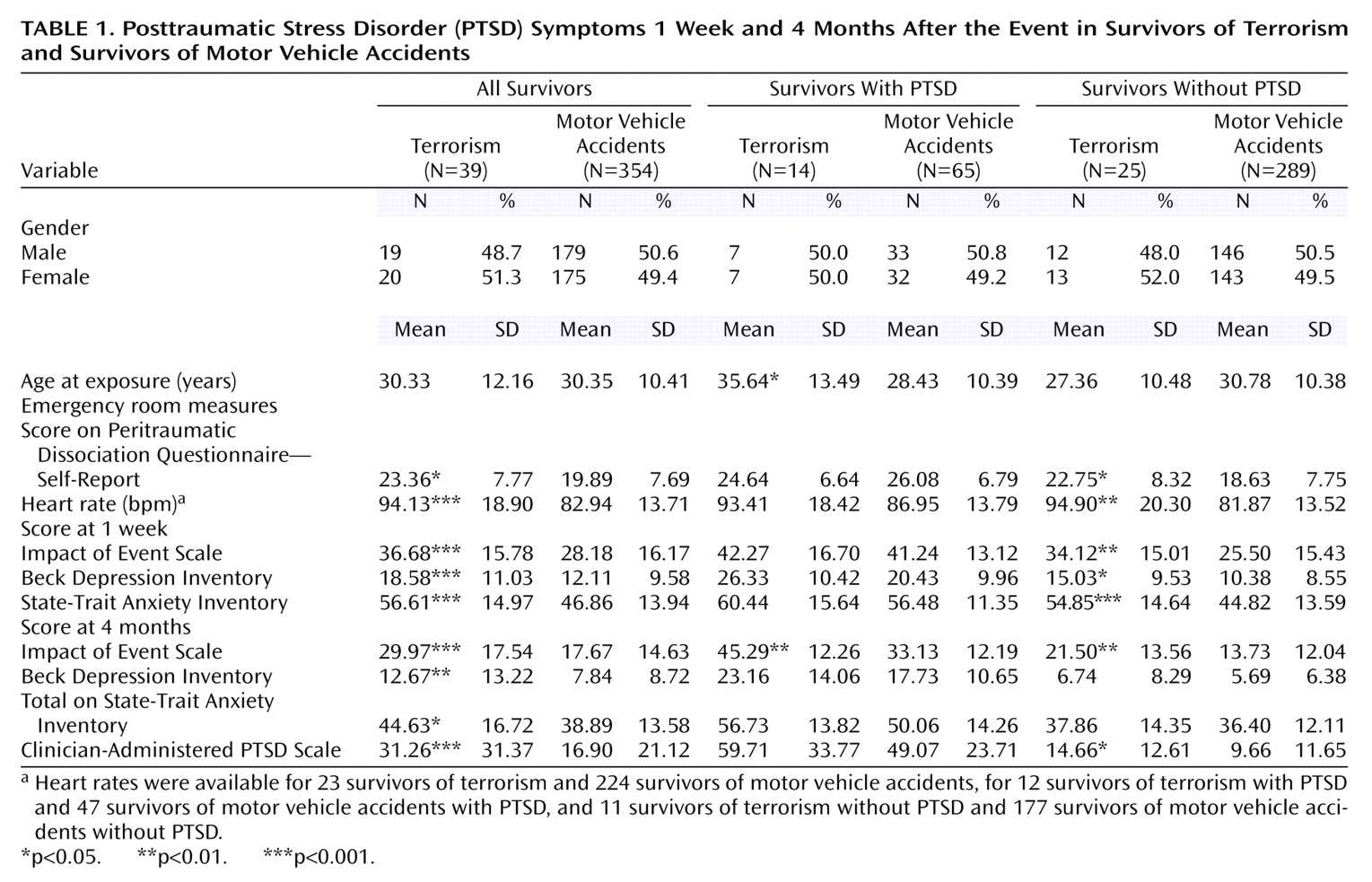
The study groups had a similar gender and age distribution (
Table 1). Fourteen survivors of terrorist attacks (36.8%) and 65 survivors of motor vehicle accidents (18.3%) met DSM-IV PTSD diagnostic criteria at 4 months (χ
2=7.34, df=1, p<0.01). Terror survivors had higher levels of dissociation, PTSD, depression, and anxiety symptoms at 1 week, and a higher heart rate at the emergency room (
Table 1). However, the difference between terror survivors and survivors of motor vehicle accidents was mainly due to higher responses among terror survivors
who did not develop PTSD (
Table 1), whereas survivors who developed PTSD had similar scores on the 1-week Impact of Event Scale, Beck Depression Inventory, State-Trait Anxiety Inventory, and Peritraumatic Dissociative Experiences Questionnaire. Terror survivors, both with and without PTSD, had a higher level of self-reported PTSD (Impact of Event Scale) symptoms at 4 months.
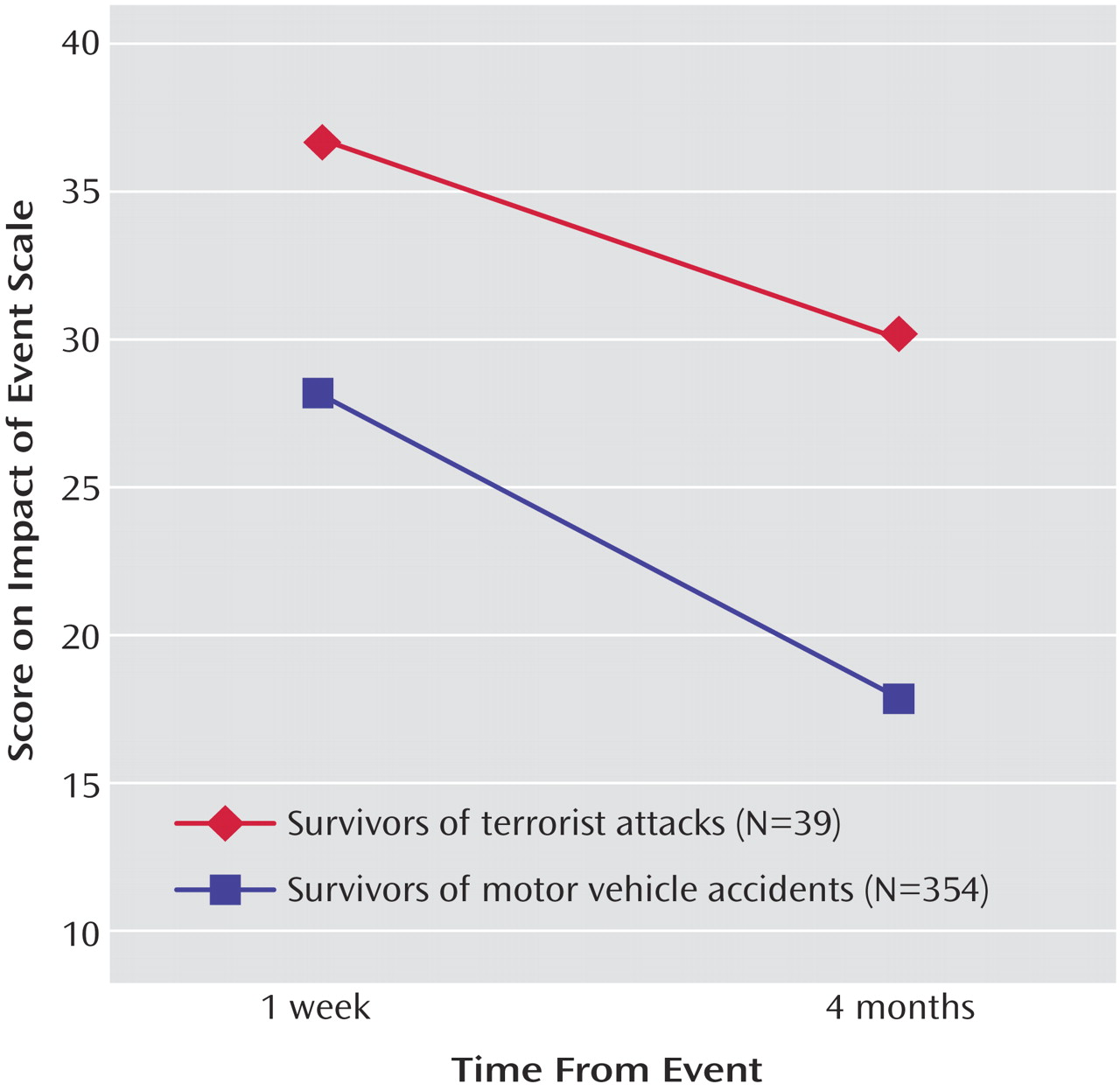
Repeated-measures analysis of variance (ANOVA) for Impact of Event Scale scores revealed a significant main effect of group (terror versus no terror: F=9.93, df=1, 386, p<0.002), a significant main effect of time (1 week versus 4 months: F=68.49, df=1, 386, p<0.0001), and no significant group-by-time interaction (F=0.10) (
Figure 1). Repeated-measures ANOVA for Beck Depression Inventory scores similarly revealed a significant main effect of group (F=6.30, df=1, 386, p<0.02), a significant main effect of time (F=48.20, df=1, 386, p<0.0001), and no significant group-by-time interaction (F=0.20).
Hierarchical logistic regression showed a significant contribution of heart rate to PTSD status at 4 months (maximum likelihood: χ2=6.63, df=1, p=0.01; odds ratio=1.29, 95% confidence interval [CI]=0.92–1.80); a significant added contribution of peritraumatic dissociation (model’s χ2=8.79, df=2, p=0.01; odds ratio=1.31, 95% CI=0.86–1.98, p<0.001 for the difference between models), and a significant additional contribution of Impact of Event Scale scores at 1 week (model’s χ2=30.77, df=3, p=0.0001; odds ratio=2.47, 95% CI=1.51–4.05, p<0.0001, for the difference between models). The type of traumatic event (terror versus motor vehicle accidents) did not add to predictions made from the initial responses (model’s χ2=32.11, df=4, p=0.25, for the difference between models).
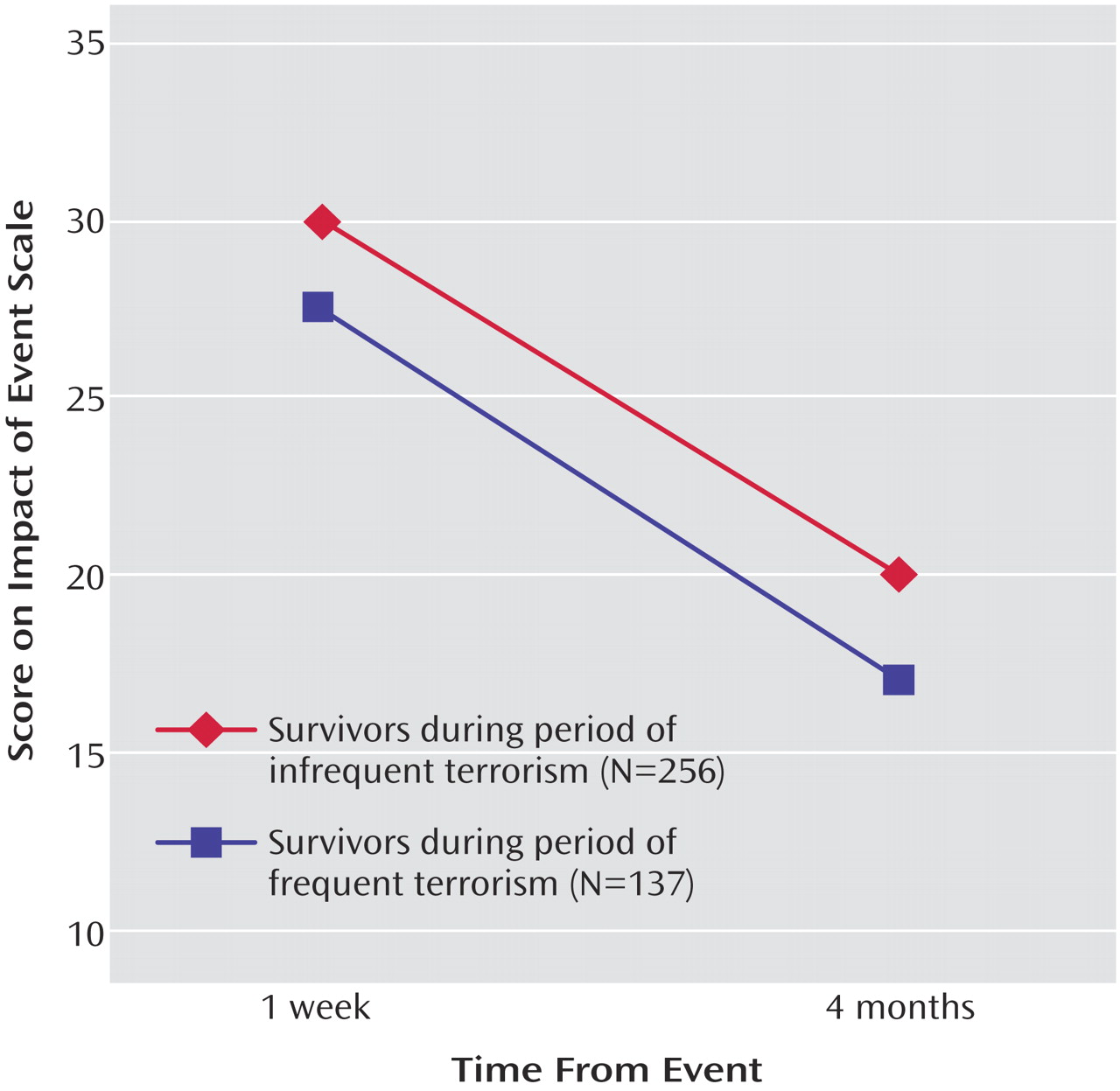
High and Low Intensity of Terrorism
In order to examine the effect of higher frequency of terrorism on the course of early PTSD symptoms, 256 survivors whose trauma occurred between April 1996 and September 2000 were compared with 137 survivors whose trauma occurred between October 2000 and March 2002. Twenty-three (9.0%) of the former and 16 (11.7%) of the latter were survivors of terrorist attacks (χ
2=0.72, df=1, p=0.39). The two groups had similar Impact of Event Scale scores at 1 week and 4 months, respectively (for the period of infrequent terrorism: mean=30.06, SD=15.62, at 1 week and mean=19.79, SD=14.15, at 4 months; for the period of frequent terrorism: mean=27.54, SD=17.15, at 1 week and mean=16.98, SD=15.29, at 4 months). Repeated-measures ANOVA for Impact of Event Scale scores showed a nonsignificant main effect of the period (F=0.82, df=1, 389), a significant main effect of time (F=185.91, df=1, 389, p<0.00001), and a nonsignificant period-by-time interaction (F=1.80, df=2, 389, p=0.15) (
Figure 2). Similar results were obtained when survivors of terrorist attacks were excluded from the analyses.
Discussion
Confirming the first hypothesis, the results of this study show that exposure to terrorist attacks is followed by a higher incidence of PTSD and higher levels of PTSD symptoms, anxiety, and depression. The decline in early symptoms, however, was not affected by the type of trauma (terror versus motor vehicle accidents) or by the occurrence of the traumatic event during a period of higher frequency of terrorist attacks. Heart rate, peritraumatic dissociation, and early PTSD symptoms contributed to subsequent PTSD.
This study did not measure trauma exposure (e.g., exposure to body parts, death, or injury). It is nonetheless plausible that the higher initial responses among terror survivors reflect the effect of the highly traumatic nature of the incidents. Once developed, however, early symptoms subside in a similar way, regardless of the original trauma. Thus, the idea that terror may somehow impair recovery from early PTSD symptoms is not supported by this work. Rather, the intensity of the early response seems to significantly determine the subsequent occurrence of PTSD.
The current study’s finding of a link between emergency room heart rate responses and PTSD replicates a previous finding
(8). However, emergency room heart rate levels in survivors of terrorist acts were high, regardless of subsequent PTSD. Indeed, the average initial heart rate among terror survivors who did not develop PTSD (mean=94.90, SD=20.30) resembles the one predicting PTSD (mean=96.4, SD=13.9) in a previous study
(8). This might reflect the highly distressing effect of terrorist acts on every survivor and possibly the very distressing atmosphere of a receiving emergency room shortly after an act of terror.
The lack of an effect of period might be explained by the fact that terrorism prevailed in Israel during the two periods. This, however, is compatible with the idea that an increment in hostilities does not necessarily change the trajectory of early PTSD symptoms. A survey of the response to terrorism in Israel
(5) has shown that continuous terror is associated with elevated levels of PTSD symptoms and also with more active coping and prevalent help-seeking. Accordingly, our negative finding might reflect an interaction between added distress on one hand and better adjustment or resiliency on the other. Resiliency during an era of
continuous terror deserves further study.
Israel has not known a time without hostilities. Therefore, an analogy between periods of “infrequent” terrorism in Israel and the situation that prevailed in the United States before Sept. 11, 2001, may not be accurate. Unfortunately, the analogy might be binding if further terrorist attacks reach the United States. In that sense, the comparison provided by this work suggests that recuperation from early distress will occur in a similar proportion despite an eventual incremental increase in the incidence of terrorism.
The results of this work show that intense initial responses are important risk indicators of PTSD across traumatic events. They support the rationale of assuming a common pathological outcome (i.e., PTSD) to various traumata. In that sense, it is remarkable that the reactions to the more frequent motor vehicle accidents behave like those that follow the responses to terrorism. Terror receives much attention and generates intense apprehension. However, the more frequent and less salient traumata may generate larger numbers of survivors with PTSD. Learning to prevent the latter may prepare the professional community to address terrorism if and when it occurs.