Although there is increasing diagnostic and longitudinal validation of the existence of a prepubertal and early adolescent bipolar disorder phenotype
(1), there is as yet, to our knowledge, no brief screen for this disorder. The absence of a published screening tool for a prepubertal and early adolescent bipolar disorder phenotype that is comparable to screening tools for adult bipolar disorder hampers epidemiological, twin, and service utilization studies. To address this need, the usefulness of the Conners’ Abbreviated Parent Questionnaire
(2), an instrument developed to assess attention deficit hyperactivity disorder (ADHD), was investigated. Dissimilar to screening tools for use with adults, a screen for a prepubertal and early adolescent bipolar disorder phenotype needed to differentiate ADHD from mania, because of the high comorbidity of ADHD among subjects with a prepubertal and early adolescent bipolar disorder phenotype
(3). To our knowledge, this is the first report of a brief screening tool for a prepubertal and early adolescent bipolar disorder phenotype.
Method
Details of the subject ascertainment method were previously published
(4). To optimize generalization, subjects with a prepubertal and early adolescent bipolar disorder phenotype and subjects with ADHD were identified through consecutive new case ascertainment from outpatient child psychiatric and pediatric sites. The healthy comparison group was identified through a random survey that matched the comparison subjects to subjects with a prepubertal and early adolescent bipolar disorder phenotype by age, gender, socioeconomic status, ethnicity, and zip code.
Details of study inclusion and exclusion criteria have been published previously
(4). Inclusion criteria were ages 7–16 years and good physical health. Both males and females were eligible for inclusion. Exclusion criteria were IQ <70, adopted status, pervasive developmental disorders, schizophrenia, epilepsy or other major medical or neurological disorder, and baseline substance dependency or pregnancy, and symptoms only while taking mania-inducing medication. There were no family history exclusions
(4).
Subjects in the prepubertal and early adolescent bipolar disorder phenotype group needed to exhibit at least one of the two cardinal symptoms of mania (i.e., elation and/or grandiosity) to avoid a diagnosis of mania only because of symptoms that overlapped with those for ADHD (e.g., hyperactivity and distractibility). Also, the prepubertal and early adolescent bipolar disorder phenotype group needed to have current DSM-IV mania for at least 2 weeks—a conservative duration chosen to address controversies in the field
(1)—and a Children’s Global Assessment Scale score ≤60, signifying impaired functioning
(5).
Inclusion criteria for ADHD subjects were current DSM-IV ADHD with a Children’s Global Assessment Scale score ≤60; exclusion criteria were no current or past mania, hypomania, or major depressive disorder. Subjects in the healthy comparison group needed a Children’s Global Assessment Scale score ≥70 and could not have current or past mania, hypomania, major depressive disorder, or ADHD.
After a complete description of the study to parents and children, informed written consent and written assent were obtained from parents and children, respectively.
The Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS)
(6), a semistructured interview, was administered by experienced research nurses separately to parents about their children and to children about themselves. The nurses were blind to the diagnostic group of the subjects. The Children’s Global Assessment Scale
(5) was used as a severity measure; the scale score was derived by the nurses who gave the WASH-U-KSADS.
Parents completed the Conners’ Abbreviated Parent Questionnaire about their children before the WASH-U-KSADS interviews. The Conners’ Abbreviated Parent Questionnaire, an instrument for assessing ADHD in children and adolescents, has 10 items, each with four possible answers. Each item has a minimum score of 1 and a maximum score of 4.
Data from the Conners’ Abbreviated Parent Questionnaire were analyzed by comparing item scores between study groups with logistic regression, with adjustment for the effects of age, pubertal status, and gender. These variables were controlled for because the ADHD subjects were significantly younger and more likely to be prepubertal and male, compared with the prepubertal and early adolescent bipolar disorder phenotype subjects and the healthy comparison subjects. Items that showed significant differences after Bonferroni correction for 10 comparisons (corrected p≤0.005) between the prepubertal and early adolescent bipolar disorder phenotype and ADHD groups were further analyzed by using receiver operating characteristic methods to determine sensitivity and specificity of the Conners’ Abbreviated Parent Questionnaire items, so that optimal cutoffs for the screen could be found. Sensitivities and specificities were obtained through Proc Logistic in SAS version 8.2 (SAS Institute, Cary, N.C.). This procedure was used to perform logistic regression with bipolar disorder status as the dependent variable and to determine sensitivity and specificity values at all possible cutoff values. Age and gender were analyzed as covariates, because optimal cutoff values could vary by age or gender.
Results
Subjects enrolled in the study included 93 with a prepubertal and early adolescent bipolar disorder phenotype, 81 with ADHD, and 94 healthy comparison subjects. Four subjects with missing values for the Conners’ Abbreviated Parent Questionnaire were excluded from the analysis, leaving 92 prepubertal and early adolescent bipolar disorder phenotype, 80 ADHD, and 92 healthy comparison subjects.
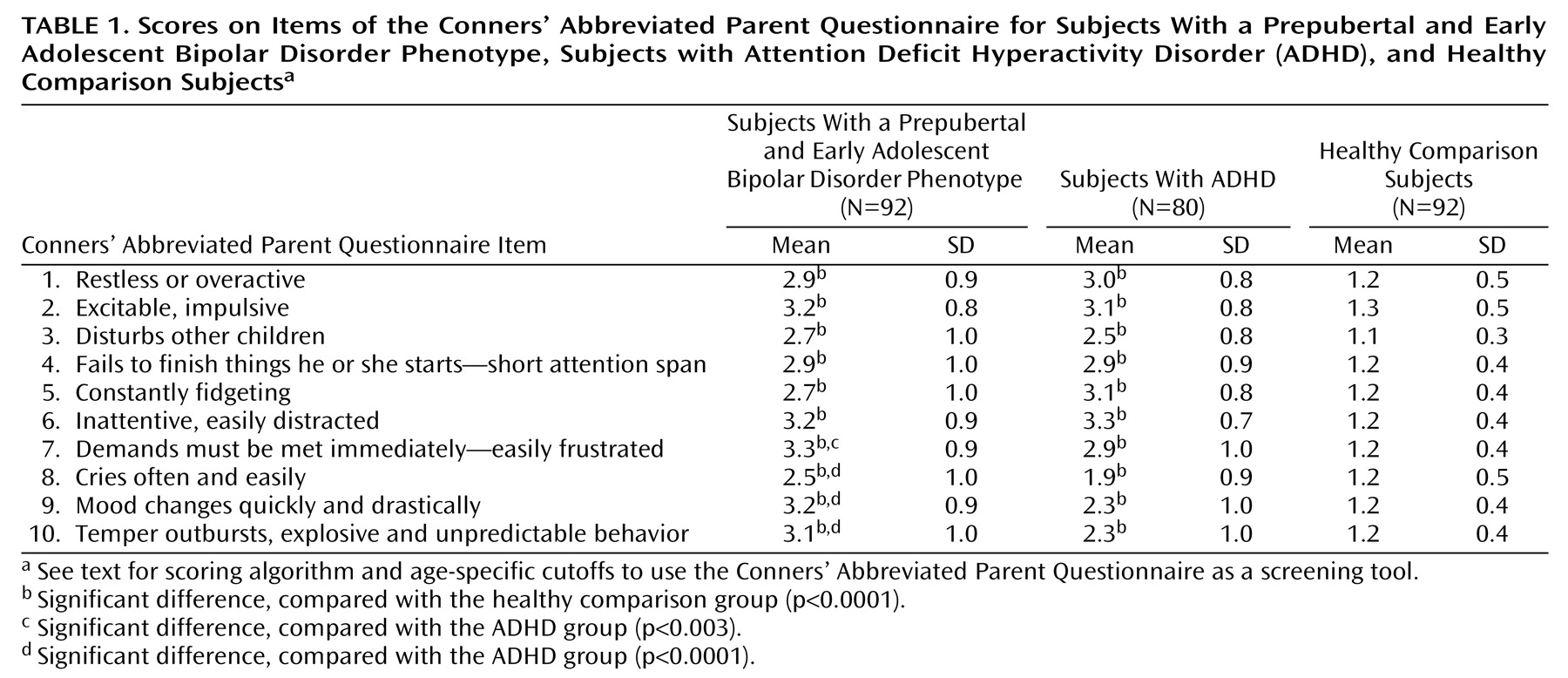
Scores for items 7, 8, 9, and 10 were all significantly higher in the prepubertal and early adolescent bipolar disorder phenotype group than in the ADHD group (
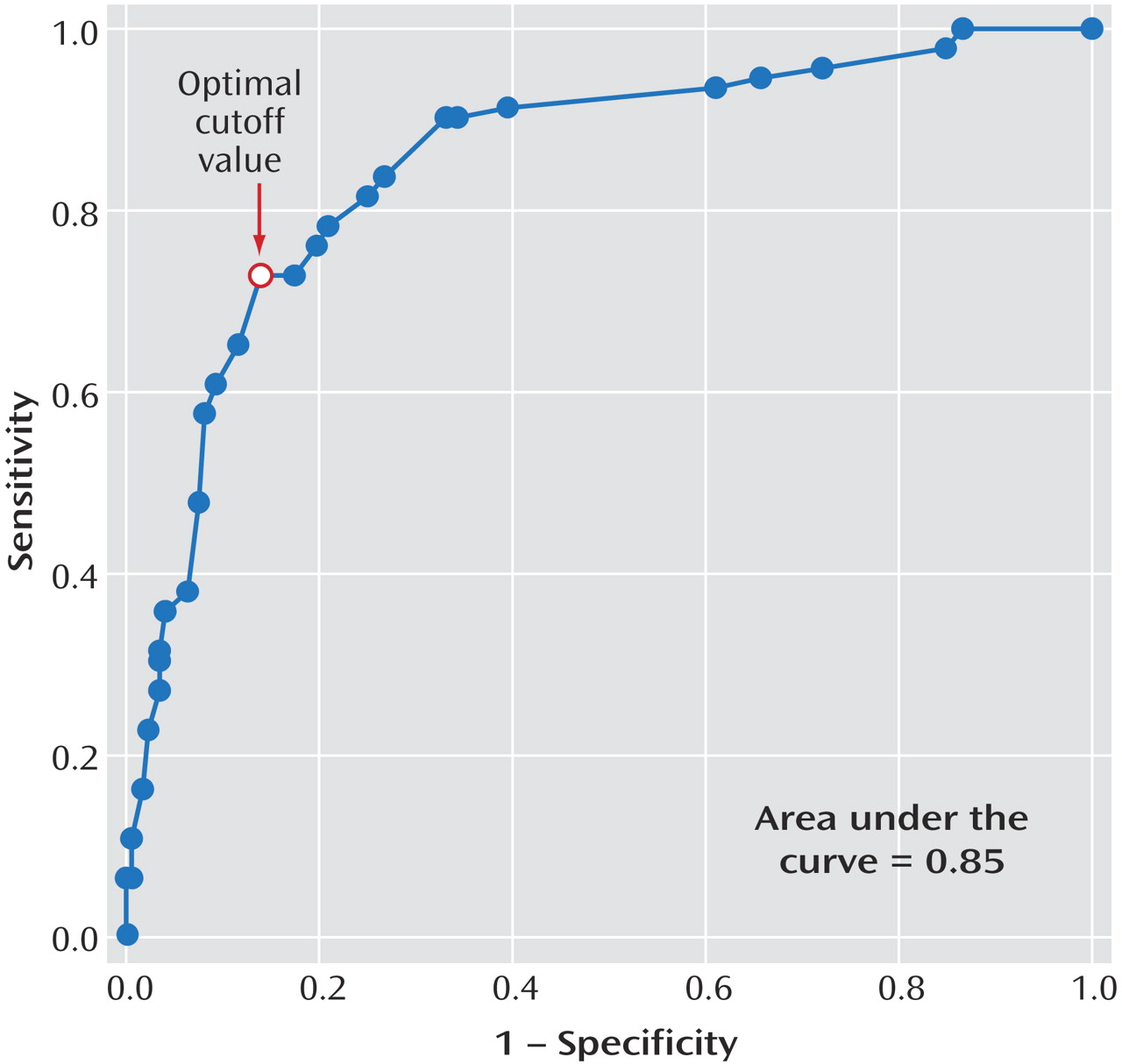
Table 1). Algorithms combining these items were compared by using receiver operating characteristic methods, and it was determined that the algorithm ([2 × item 8 score] + item 9 score) provided the best screen for a prepubertal and early adolescent bipolar disorder phenotype. Optimal cutoff values for ([2 × item 8 score] + item 9 score) were ≥9 for subjects ages 7–8 years, ≥8 for subjects ages 9–10 years, and ≥6 for subjects ages 11–16 years. The receiver operating characteristic curve is shown in
Figure 1. Utilizing age group as a covariate yielded a sensitivity of 0.73 and a specificity of 0.86. The screen identified 73% of the prepubertal and early adolescent bipolar disorder phenotype subjects, 26% of the ADHD subjects, and 3% of healthy comparison subjects. Using gender as a covariate did not improve the model.
To test that this procedure was not a failed use of the Conners’ Abbreviated Parent Questionnaire, the sensitivity and specificity for detecting ADHD were calculated by using data for all 10 items from the ADHD subjects and the healthy comparison subjects. The sensitivity was 0.99, and the specificity was 0.95.
Discussion
The Conners’ Abbreviated Parent Questionnaire is an easy-to-complete, 10-item scale that provided good psychometrics as a screen for an outpatient prepubertal and early adolescent bipolar disorder phenotype in a study group of children and adolescents that included subjects with ADHD.
The sensitivity and specificity found in this group were comparable to those reported in the literature on screening for adult bipolar disorder
(7–
9). Specifically, the Conners’ Abbreviated Parent Questionnaire performed similarly to the Mood Disorder Questionnaire, a screen used with adult outpatients
(8).
Limitations include that the Conners’ Abbreviated Parent Questionnaire screen may not generalize to phenotypes other than a prepubertal and early adolescent bipolar disorder phenotype
(1) or to hospitalized subjects. However, the similarity of inpatient and outpatient prepubertal and early adolescent bipolar disorder phenotype subjects has been discussed
(1). Performance of the Conners’ Abbreviated Parent Questionnaire may also vary in study populations with different comorbidity patterns
(3). It is likely, however, that the sensitivity and specificity reported here are conservative, because the discrimination of a prepubertal and early adolescent bipolar disorder phenotype from ADHD is the key differential diagnostic problem in the pediatric age group.