Brains of Bipolar Kids
Compared to adults with bipolar disorder, children and adolescents with this illness have more severe symptoms, a stronger genetic predisposition, and less past drug treatment. Their brains might therefore provide a clearer picture of anatomic abnormalities in bipolar disorder. Frazier et al. (p. 1256) measured three brain regions in 43 youths with bipolar disorder and 20 healthy youths. The amygdala and thalamus showed no difference between groups, but the hippocampus, which provides context for learning and memory, was smaller in the bipolar youths. The bipolar girls showed an especially pronounced difference from the same-sex comparison subjects, and their mania scores were higher than those of the bipolar boys. The total cerebral volume in the bipolar group was also smaller than normal. Since total cerebral volume generally is normal in affected adults, bipolar disorder in children and adolescents may follow a different neurodevelopmental path.
The Incredible Shrinking Hospital Stay
From 1989 to 1995, the average length of hospitalization for psychotic disorders in Suffolk County, N.Y., plummeted from 41 to 21 days. Nevertheless, Mojtabai et al. (p. 1291) found that posthospitalization symptoms and illness course and outcomes were no worse among patients admitted in 1995 than among those hospitalized in 1989. There was also no significant change in the number of rehospitalizations, the rate of suicide or homelessness, or use of outpatient mental health services. In fact, patients admitted in the later years were more likely to have returned to their highest level of functioning by 4-year follow-up. Introduction of atypical antipsychotic drugs did not account for this lack of decline in patient outcomes. One troubling finding was the greater likelihood of partial or no remission at discharge among patients hospitalized later in the study period. Linkage to outpatient services is especially important for these patients.
Protecting Burned Children From PTSD
Fire is a common cause of accidental injuries to children. Little is known about which of these children develop posttraumatic stress disorder (PTSD) and which do not. Saxe et al. (p. 1299) found two separate causal pathways to PTSD in 72 children admitted to a hospital for burn victims. Separation anxiety and dissociation of mental processes (e.g., amnesia for traumatic events) independently contributed to PTSD at 3 months after hospitalization. Each was itself influenced by the size of the burn. Separation anxiety was also greater for younger children and those with greater pain. Anxiety and dissociation appear to reflect different biological reactions to overwhelming stress—a fight-or-flight response versus freezing/immobilization. These two pathways to PTSD suggest specific interventions to help burned children: increased availability of their parents in the hospital, support of the parents, and psychosocial and biological treatments for pain, anxiety, and dissociation.
Kids Hospitalized for Self-Injury
Between 1990 and 2000, the overall rate of hospitalization for children and adolescents who intentionally injured themselves declined only slightly. However, the average length of these hospital stays decreased significantly, and diagnoses shifted toward more severe conditions, e.g., bipolar disorder. Olfson et al. (p. 1328) derived these findings from over 10,000 hospitalizations for self-inflicted injuries of patients ages 5–20 years. Although the rate did not change overall, hospitalizations increased for children ages 5 to 9 years, for ingestion of acetaminophen and antidepressants, and for injuries from cutting and from hanging or suffocating. Cutting may be more closely related to self-mutilation than to suicidal behavior, however, and without it the rate of hospitalizations for self-inflicted injuries shows an actual decline, from 47.2 per 100,000 population in 1990 to 39.4 per 100,000 in 2000.
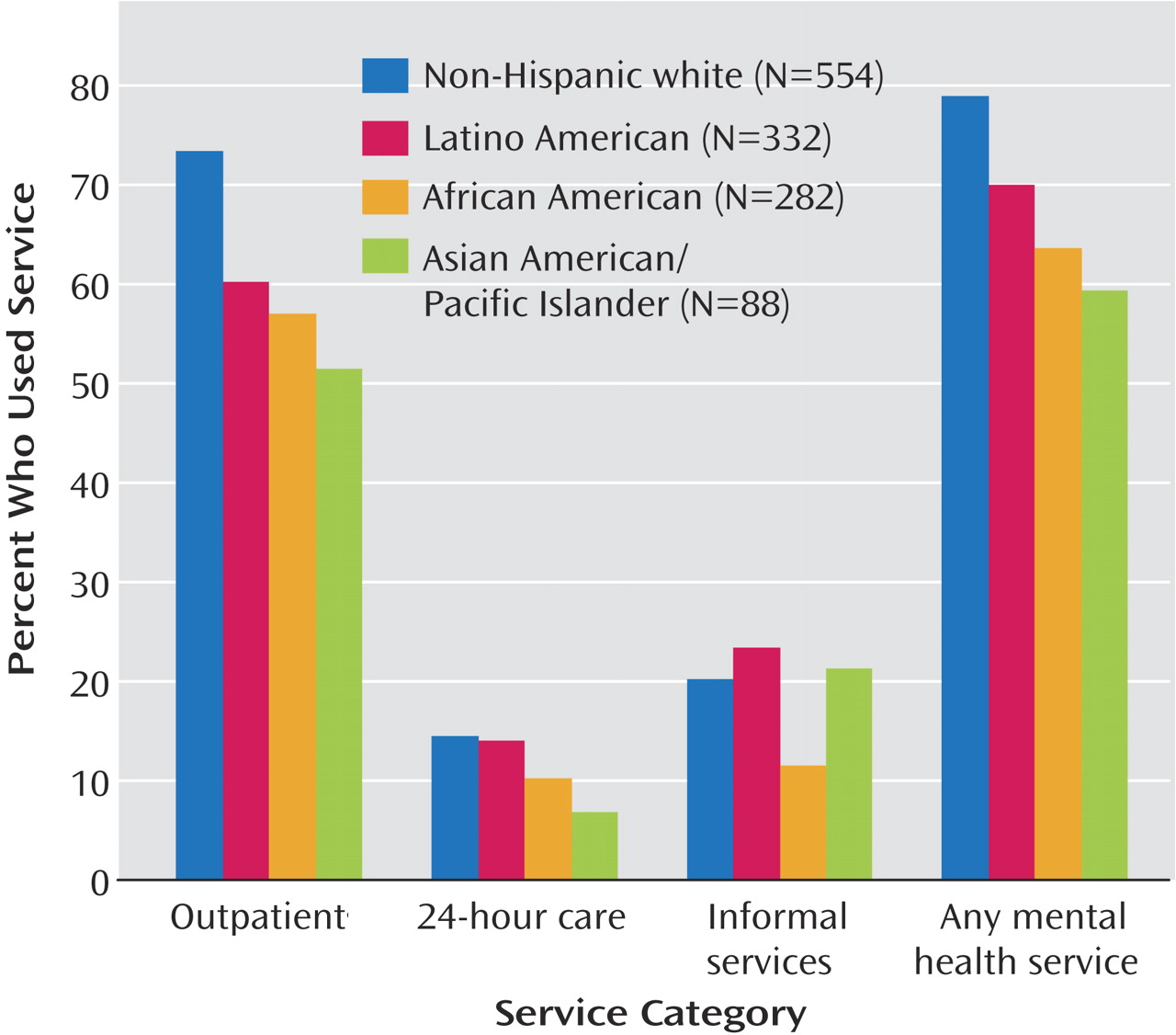
Race of High-Risk Youths Affects Use of Mental Health Services
Many children and adolescents in child welfare programs, the juvenile justice system, and other public care sectors need mental health services. The Surgeon General’s Report on Mental Health has identified racial/ethnic disparities in use of mental health services as a major public health problem. Garland et al. (p. 1336) examined whether ethnicity itself, apart from associated factors such as socioeconomic status, influenced the use of mental health services by 1,256 children and teens in five types of public care in San Diego County. Compared to non-Hispanic whites, African Americans and Asian Americans were approximately half as likely to receive outpatient services, as well as mental health services in general. Other predictors, such as caregiver strain, were also identified and suggest that attention to family- and system-level factors could open doors to young people needing help.
Images in Psychiatry
Milton Hyland Erickson, 1901–1980 (p. 1255).