Heterogeneity of Borderline Personality Disorder
Not all patients with borderline personality disorder are the same. Although DSM-IV-TR provides a broad definition of borderline personality disorder as a “pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity,” the diagnosis is determined by the presence of any five of the nine diagnostic criteria for the disorder. By this method, there are numerous combinations of criteria that can constitute an “official” diagnosis of borderline personality disorder
(1). In addition, some patients who have clinically significant symptoms of borderline personality disorder may have fewer than the five diagnostic criteria required for an official diagnosis.
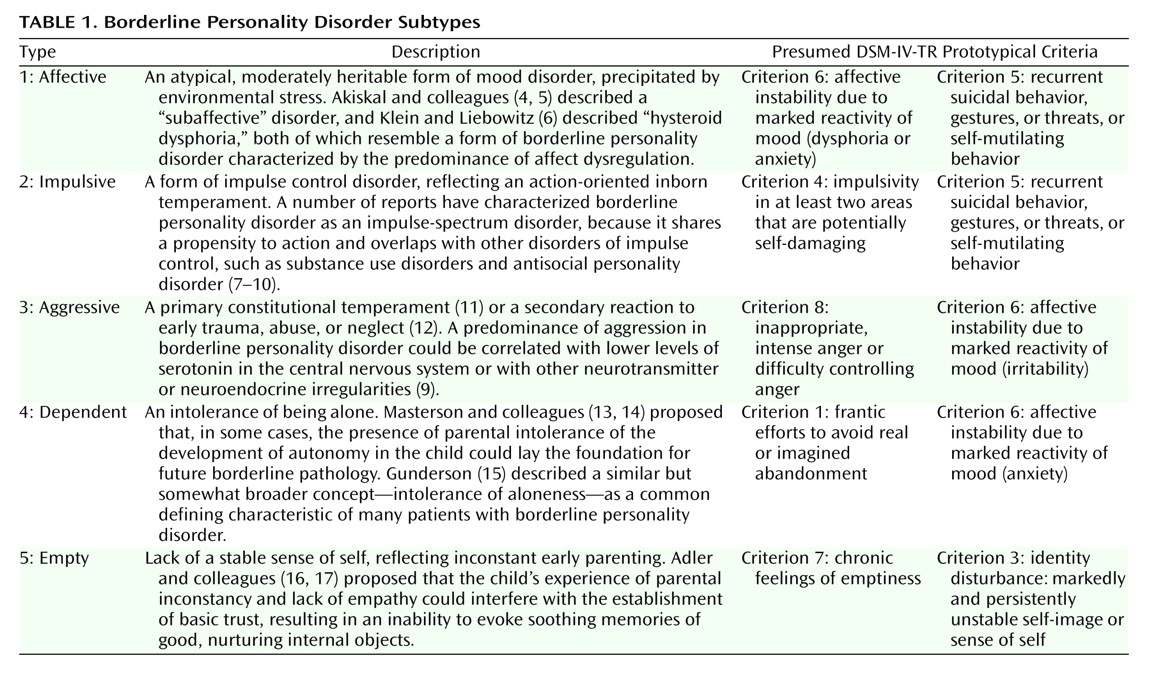
A subtyping system based on theories of the etiology of borderline personality disorder has been suggested
(2,
3) (
Table 1). Although this system has not been tested empirically, the typology suggests that suicidal symptoms (DSM-IV-TR criterion 5: “recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior”) would be especially prominent when dysregulation of either affect or impulse control (type 1 or type 2) predominates in the overall symptom pattern.
Suicidality Versus Self-Injurious Behavior
Self-injurious behavior is characteristic of patients with borderline personality disorder and is sometimes referred to as the borderline patient’s “behavioral specialty”
(7,
22). This type of behavior includes impulsive behavior that is potentially dangerous (e.g., excessive drinking, high-risk sexual activity), deliberate self-injurious behavior (e.g., superficial cutting or burning), suicide attempts, and completed suicide. In the literature, there is some variability in meaning for terms such as suicide attempt, suicide gesture, “parasuicide,” and self-injurious behavior. Stanley and Brodsky
(23) suggested that deliberate self-harm includes two forms of self-destructive behavior. One form, suicide attempt, consists of intentionally self-destructive acts accompanied by at least a partial intent to die. This definition would include suicide “gestures.” In contrast, self-injurious behavior is nonsuicidal self-injury or self-mutilation—i.e., intentionally self-destructive behavior with no intent to die. The term “parasuicide” refers to any nonlethal intentional self-injurious behavior. Stanley and Brodsky
(23) estimated that as many as 75% of patients with borderline personality disorder make at least one nonlethal suicide attempt, and even higher percentages of patients, especially of hospitalized patients, engage in self-injurious behavior. It is erroneous, however, to assume that patients with borderline personality disorder who show self-injurious behavior are not at risk for suicide. Both forms of self-destructive behavior may occur in the same patient, and it is estimated that the presence of self-injurious behavior in a given patient doubles the patient’s risk for suicide
(22).
Because of the frequency of self-injurious behavior in patients with borderline personality disorder and because such behavior is often viewed as an effort to elicit a desired response from another person, self-injurious behavior can be mistakenly thought of as willful, deliberate, and under the patient’s control. However, self-injurious behavior in patients with borderline personality disorder is incompletely understood, and it may be associated with different motivations, meanings, or goals from one patient to another or at various times in the same patient. It may produce relief of acute dysphoria
(23) and may be accompanied by analgesia, perhaps suggesting the release of endogenous opiates during acute intensification of dysphoric states
(24).
Comorbidity
Numerous studies have identified high rates of comorbidity in patients with borderline personality disorder. Intra-axis-II comorbidity is common
(25,
26), but little is known about whether particular combinations of disorders correlate with predictable patterns of suicidal behavior. Among personality disorders, antisocial personality disorder, like borderline personality disorder, is associated with suicide risk. The estimated lifetime suicide risk for patients with antisocial personality disorder is 5%
(27,
28). However, this estimate may be low, because patients with antisocial personality disorder have a high rate of risk-taking behavior, and it is difficult to differentiate suicide from accidental death. The relative rates of suicide in patients with comorbid borderline personality disorder and antisocial personality disorder, compared to patients with either condition alone, are unclear, although Soloff et al.
(29) found a higher level of lethality of suicide attempts in patients with the comorbidity, compared to patients with borderline personality disorder alone. In clinical populations, borderline personality disorder occurs predominantly in female patients
(7), but it is more evenly distributed among males and females in the general population
(30). One possible explanation for this difference in gender ratio in clinical versus nonclinical populations is that the comorbidity of borderline personality disorder and antisocial personality disorder occurs most often in non-treatment-seeking males.
Instead of approaching the question of comorbidity by using the DSM-IV-TR categorical system, many experts in personality studies prefer a dimensional approach. Using a dimensional framework, Links and Kolla
(28) identified three personality characteristics as relevant for suicidal behavior in psychiatric patients—impulsive aggression, perfectionism, and emotional dysregulation. Of these, impulsive aggression and emotional, or affective, dysregulation are the two most relevant factors for suicidal or self-injurious behavior in patients with borderline personality disorder.
Axis I/axis II comorbidity is also common
(26,
30,
31), and there is particular interest in the comorbidity of borderline personality disorder with major depressive disorder
(28,
30,
32–34) and with substance abuse
(28,
30,
35,
36). In a study of inpatients with borderline personality disorder, Soloff and colleagues
(37) reported that the comorbidity of borderline personality disorder and major depressive episode increased the number and seriousness of suicide attempts. They also identified impulsivity and hopelessness as independent risk factors for suicidal behavior in patients with comorbid borderline personality disorder and major depressive episode. In a patient with borderline personality disorder only, the symptoms of depression and suicidality are usually reactive to interpersonal or other real or perceived stresses and are usually of brief duration. If such a patient makes a suicide attempt, the attempt is often impulsive in nature. In contrast, in a patient with comorbid borderline personality disorder and axis I major depressive episode, symptoms of depression and suicidality develop and deepen gradually and may persist for weeks (or much longer if not treated). Such patients may show loss of appetite, sleep disturbances, loss of interest in ordinarily pleasurable activities, and other persistent signs and symptoms of depression.
The well-documented comorbidity of substance abuse with borderline personality disorder
(28,
30,
35,
36) increases patients’ risk for impulsive suicidal behavior and for impaired judgment. Because of the impaired judgment, a suicidal act made with a low level of intent to die could have lethal results in such patients. The APA Practice Guideline for the Treatment of Patients With Borderline Personality Disorder
(21) specified that patients with comorbid borderline personality disorder and substance abuse problems have a more guarded prognosis and are at greater risk for suicide or death from injury or accident, a heightened risk also noted by others
(28,
34–36).