“Behavioral disinhibition” represents an extreme tendency to seek out novelty, approach unfamiliar stimuli, and display disinhibition of speech and action in unfamiliar settings
(1). This tempermental trait can be observed in the laboratory as early as toddlerhood. Studies have documented the moderate stability of behavioral disinhibition from toddlerhood through middle childhood
(2–
4). Prospective studies have found associations between behavioral disinhibition at preschool age and oppositional disorder
(5) or inattention
(6) at age
(7), delinquency at 10–13
(7), aggression at 11
(8), and antisocial behavior at 13–15
(9) and at 21
(10). In a preliminary study of children at risk for panic and depression
(11), we found that children ages 2–6 with behaviorial disinhibition had higher rates at a mean age of 6 of disruptive behavior disorders, mood disorders, and their comorbid state than noninhibited children, suggesting that behaviorial disinhibition may be an early marker of risk for dysregulatory disorders.
Behavioral disinhibition might be hypothesized to be elevated among the offspring of parents with bipolar disorder based upon two lines of evidence
(1). First, the cluster of behavioral outcomes associated with behavioral disinhibition (including oppositional-defiant, conduct, and comorbid mood disorders) are all common prodromes or associated features of bipolar spectrum disorders in affected individuals
(12–
16) and at-risk offspring
(12, 17– 18). Longitudinal studies have suggested that early externalizing or affective symptoms appear to precede the onset of bipolar disorder
(18–
19) and may in some cases represent its early manifestations in children. Second, studies have supported links between bipolar disorder and specific personality styles suggestive of behavioral disinhibition, including “hyperthymic” personality
(20–
21), novelty-seeking
(22–
23), extroversion
(22,
24), and the approach of novelty
(25). As Graham and Stevenson
(26) suggested, the temperamental characteristics most likely to indicate risk for bipolar disorder may represent less extreme behaviors on a continuum with the disorder in question. Therefore, offspring at risk for bipolar disorder may show a trajectory from behavioral disinhibition in the preschool years to disruptive behavior and bipolar disorder in childhood and adolescence.
Although it might be argued that behavioral disinhibition may be an early manifestation of bipolar disorder in children, we think it more accurate to regard it as a predisposing factor. The prevalence of behavioral disinhibition in the general population (estimated at 20%–30% in some studies) far exceeds the prevalence of juvenile bipolar disorder (estimated at 1%)
(27). Additionally, most disinhibited children followed in the studies cited above did not manifest bipolar disorder. Therefore, conceptually, we regard behavioral disinhibition as a marker of motivational or emotional dysregulation that might predispose a child to develop one of several dysregulatory disorders
(28), such as attention deficit hyperactivity disorder (ADHD); oppositional defiant disorder, conduct disorder, psychoactive substance use disorders; or bipolar disorder
(29–
30). As a potential prodrome of bipolar disorder, behavioral disinhibition shares some features of the dysregulation associated with bipolar disorder, just as prodromal indicators of schizophrenia in individuals at high risk include features that are also criteria for its diagnosis (e.g., negative symptoms, social withdrawal).
Testing the hypothesis that behavioral disinhibition may index risk for bipolar disorder requires identifying a group at clear risk for bipolar disorder (i.e., offspring of affected parents) and assessing behavioral disinhibition early in life. The older the child, the more likely that temperament will be obscured by overlap with other behaviors (e.g., onset of symptoms, learned modifications of behavioral tendencies). Therefore, we conducted a secondary analysis of a preexisting group of children at risk for panic disorder and depression in whom temperament and psychiatric disorders had already been assessed
(11). We stratified the children based on the presence or absence of parental bipolar disorder and compared rates of laboratory-observed behavioral disinhibition at ages 2–6 years between the offspring of parents who were and were not affected. Therefore, our study can be considered a “high-risk” design
(31).
Method
Participants
This study is a secondary analysis of data from a group of offspring at risk for panic disorder and major depression and a group of comparison offspring. We had recruited three groups of parents who had at least one child in the age range to be assessed temperamentally (2–6 years): 1) 119 parents treated for panic disorder with or without comorbid major depression and their 151 children, 2) 37 parents treated for major depression with no history of either panic disorder or agoraphobia and their 49 children, and 3) 60 comparison parents without major anxiety or mood disorders and their 84 children
(32). The parents with panic disorder and major depression had been recruited from outpatient settings and advertising and were included if they met full DSM-III-R criteria for panic disorder or a major depressive episode by structured psychiatric interview and had been treated for these disorders. Although the participants were not recruited based on treatment for bipolar disorder, a small subgroup of those treated for panic or depression was found, according to structured diagnostic interviews for the study, to have had a history of manic or hypomanic episodes (or to have spouses with such a history). Comparison parents who were free of major anxiety (panic disorder, agoraphobia, social phobia, and obsessive-compulsive disorder) or mood disorders (major depression, bipolar disorder, and dysthymia) had been recruited through advertisements and were included only if they and their spouses did not meet DSM-III-R criteria for these disorders. This study was approved by the institutional review board, and written informed consent was obtained from all parents. The children assented to the study procedures.
Diagnostic Assessments of Parents
We conducted direct assessments with each parent using the Structured Clinical Interview for DSM-III-R (SCID=NP)
(33). We documented the degree of impairment associated with each diagnosis. Bipolar disorder was assessed at study inception by using the SCID module for mania. The patients whose manic episodes were rated as causing “severe” impairment or leading to hospitalization were rated as having bipolar I, and those whose manic episodes were rated as causing only “moderate” or “mild” impairment were rated as having bipolar II. To be conservative in the assessment of bipolar II, hypomanic episodes (as well as manic episodes in bipolar I) were required to persist for a week or more. We assessed socioeconomic status with the Hollingshead Four-Factor Index of social status
(34).
Interviews were conducted by raters with bachelor’s degrees in psychology under the supervision of two senior psychiatrists (J.B. and J.F.R.). The raters underwent a training program that required them to learn DSM-III-R criteria, master the diagnostic instrument, participate in interviews performed by experienced raters, rate several subjects under the supervision of the project coordinator, undergo continued supervision of their assessments by senior project staff, and audiotape all interviews for random checking. All subjects were diagnosed based on consensus judgment by the two senior psychiatrists.
To confirm the reliability of the interview procedures, unweighted kappa coefficients of agreement
(35) were computed between the interviewers and board-certified psychiatrists who listened to a randomly selected subgroup of audiotaped interviews. On the basis of 173 interviews, the mean kappa across all diagnoses was 0.86. The kappa for the diagnosis of any bipolar disorder (I or II) was 0.94.
Assessment of Temperament
The children were assessed by examiners and raters who were blind to all diagnostic information about the parents. Blindness was ensured as follows: 1) examiners assessing children were blind to all diagnostic information about the parents, 2) interviewers of the parents were blind to all information about temperament, and 3) final diagnostic classifications of all parents were performed by clinicians blind to the original recruitment group and to child temperament.
Temperamental assessments were conducted in the Harvard Infant Study laboratory under the direction of Jerome Kagan and Nancy Snidman. They measured the child’s reaction to unfamiliar people, rooms, objects, and test procedures
(36). Evaluations consisted of a 90-minute battery in which the child (accompanied by the mother) interacted with an unfamiliar female examiner administering a series of tasks. Each child was evaluated once—at age 2, 4, or 6 years—with an age-specific protocol
(32).
The children were classified as showing behavioral disinhibition if they displayed novelty-seeking (approaching unfamiliar stimuli) and/or impulsivity (disinhibition of speech or action). Full details of the variables coded and their rationale are reported elsewhere
(11). Briefly, to be rated with behavioral disinhibition, 2-year-olds had to show minimal avoidance of unfamiliar stimuli, maximal approach of a clown (a stimulus most toddlers avoid), or maximal vocalization; 4-year-olds had to make more spontaneous comments than 75% of the children of comparison parents; and 6-year-olds had to make more spontaneous comments than 75% of their comparison peers and either be rated “extremely uninhibited” on a global rating or show impulsive style on the Matching Familiar Figures Test
(37).
The children from the group had also been assessed for behavioral inhibition, a tendency to display restraint, reticence, or fear in novel situations
(32) with the following three definitions:
1. Dichotomous behavioral inhibition: based on showing four or more fears or having minimal vocalizations or smiles (2-year-olds) or on displaying fewer spontaneous comments and smiles than the lowest 20th percentile of comparison children at their age level (4- and 6-year-olds)
2. Global behavioral inhibition: receiving 3 or greater on a 4-point global rating of behavioral inhibition (rated for 4- and 6-year-olds only)
3. Summary behavioral inhibition: a summary score derived from a principal factors factor analysis of all variables indexing inhibition; the children were rated as inhibited if they scored in the upper 20th percentile of comparison children their age. Consensus behavioral inhibition combined the three definitions: 2-year-olds had to meet both available definitions, and 4- and 6-year-olds had to meet two of three.
All temperamental variables were rated by a single rater (Jerome Kagan). As a reliability check, a random sample of 20 videotapes was rated by a second trained rater: the intraclass correlation (ICC[A,1])
(38) for spontaneous comments was 0.89 and for smiles, ICC(A,1)=0.82; the global 4-point rating of inhibition had an unweighted kappa=0.70
(35). The model ICC(A,1) assumes random effects for subjects and times of assessment
(38).
Group Size
Of the 284 children assessed temperamentally, three were excluded because they met criteria for both behavioral disinhibition and behavioral inhibition, and three were missing information about parental bipolar disorder. Therefore, the analysis focused on 278 children. Thirty-four children from 28 families in which one parent had bipolar disorder (12 fathers and 16 mothers) were compared with 244 children from 184 families whose parents did not have bipolar disorder. The 34 children included 15 children of 13 parents who had a parent with panic disorder and comorbid bipolar disorder, 12 children from 10 families who had one parent with panic disorder and one with bipolar disorder, and seven children of five parents who had been treated for a major depressive episode and were found on the SCID to meet criteria for bipolar disorder. Of the offspring with a bipolar parent, 18 children had a parent with bipolar I disorder, and 16 had a parent with bipolar II disorder. To ensure adequate power for comparisons, the offspring of bipolar I and II parents were combined.
Statistical Methods
We compared rates of child behavioral disinhibition or behavioral inhibition between the offspring of parents with and without bipolar disorder and between the offspring of parents with bipolar disorder and other subcategories of disorder (categorical variables, with offspring of bipolar disorder parents contrasted with each other group). Multiple siblings in a single family cannot be considered independently sampled because they share genetic and social risk factors. Therefore, we used logistic regression, with Huber corrections, and controlled for one or more potentially confounding variables as implemented in Stata
(39). All tests were two-tailed with alpha set at 0.05.
Potential confounders were treated as follows. First, we identified candidate confounders based on prior knowledge. These included the child’s age in years (continuous), sex, race (binary: white versus nonwhite), sibship size (continuous), socioeconomic status (Hollingshead class, treated as continuous), and family intactness (binary). These also included the following clinical variables (all binary): parental ascertainment based upon treatment for panic disorder, and parental lifetime history of ADHD, antisocial personality disorder, conduct disorder, or psychoactive substance use disorders—disorders shown to be associated with behavioral disinhibition
(7, 9–11,
29). The variables deemed “most relevant” were included in all models; for models predicting child behavioral disinhibition, these were parental ADHD, parental antisocial, parental conduct, and parental psychoactive substance use disorders; whereas for the model predicting child behavioral inhibition, the “most relevant” confounders was parental panic disorder
(32). Other variables were tested with the “10% method”
(40): models were run with and without the potential confounders, and if the odds ratio for parental bipolar disorder predicting child behavioral disinhibition or behavioral inhibition changed by 10% or more, the variable was included as a confounders in the model.
Results
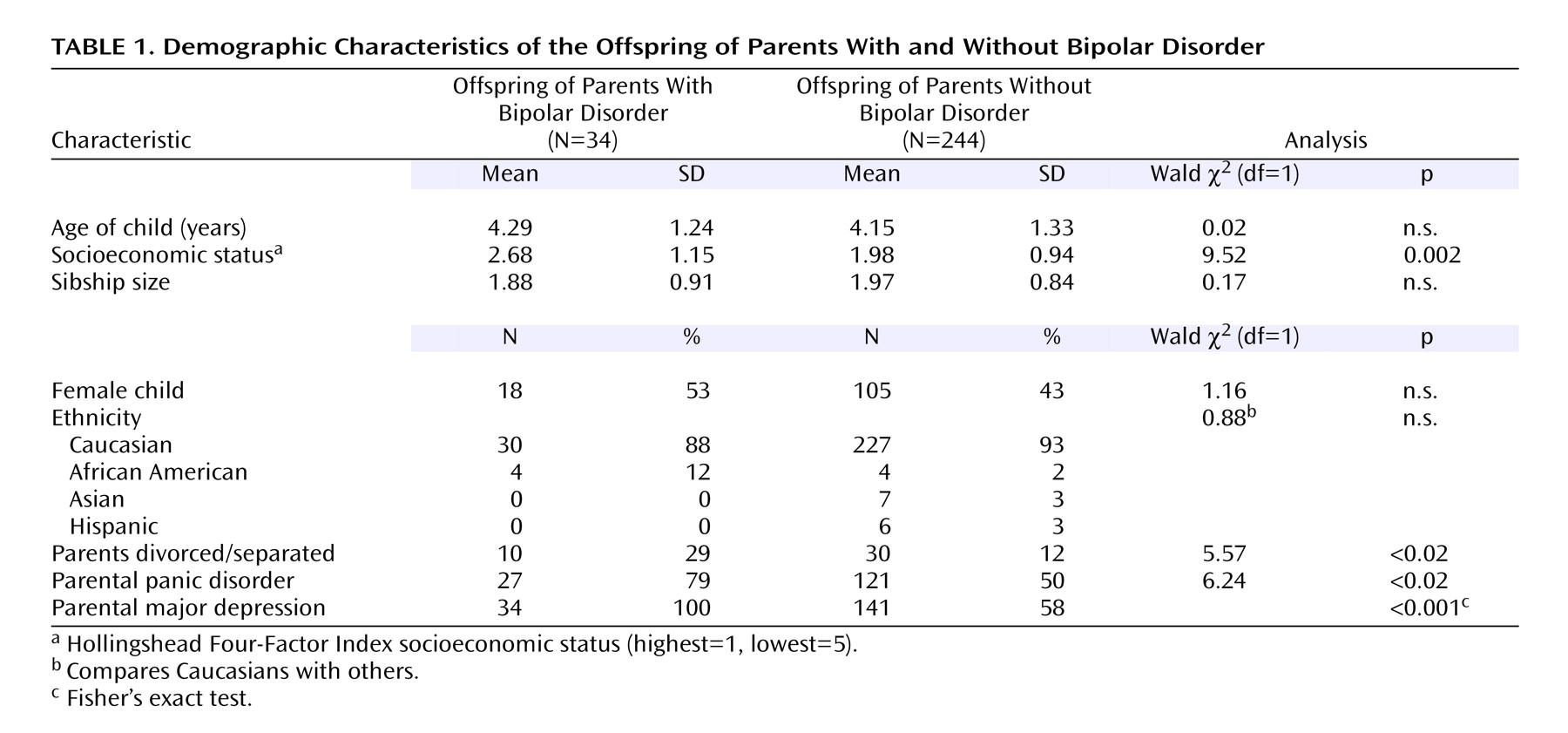
The offspring of bipolar and nonbipolar parents differed significantly by socioeconomic status, family intactness, and parental diagnosis (presence or absence of panic disorder or major depression) (
Table 1).
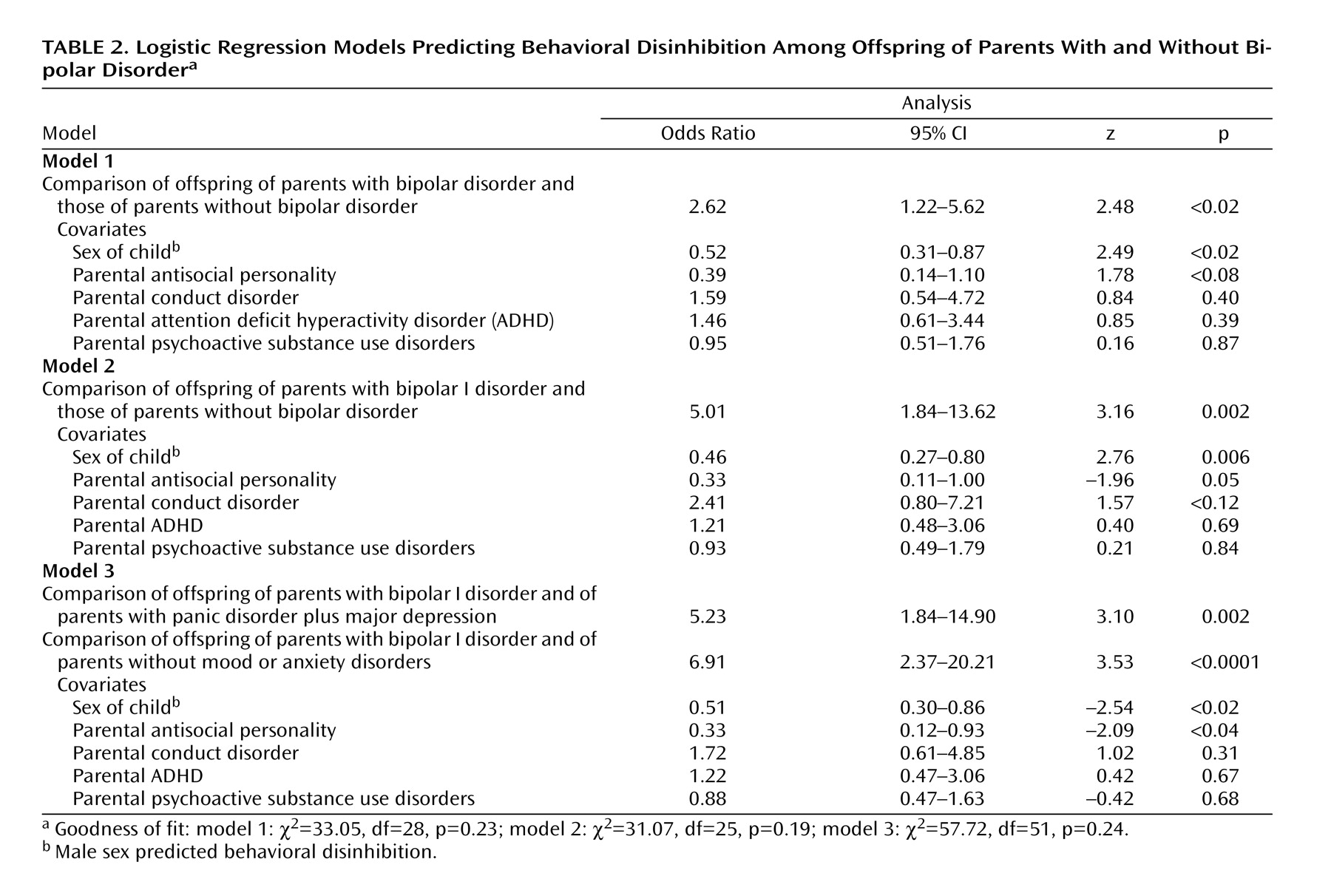
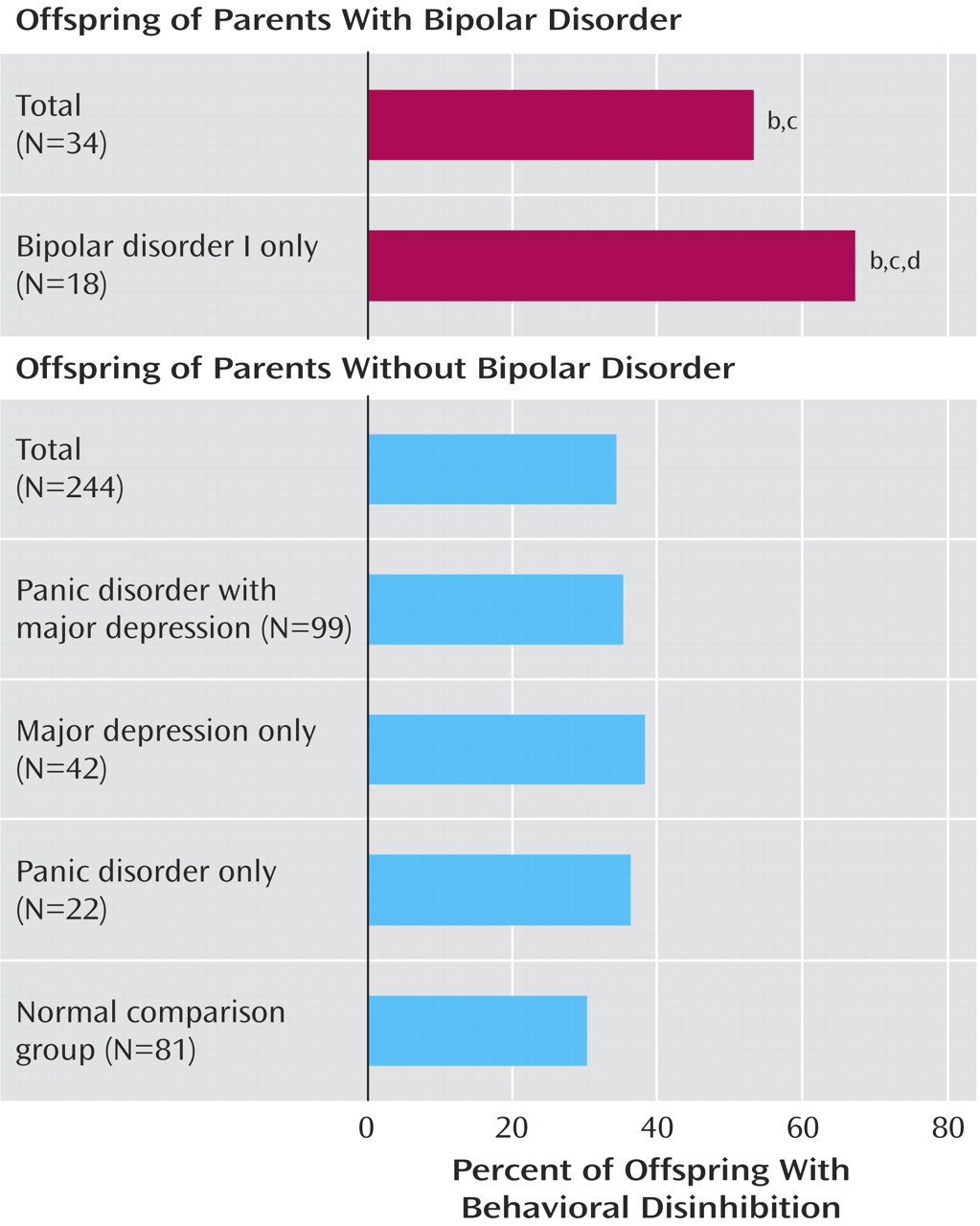
As seen in
Figure 1, the rate of behavioral disinhibition was significantly higher among the offspring of parents with bipolar disorder than among the offspring of parents without bipolar disorder: 53% versus 34% (odds ratio=2.62, 95% confidence interval [CI]=1.22–5.62). This model covaried parental history of antisocial personality disorder, conduct disorder, ADHD, and psychoactive substance use disorder and child sex, which was identified as a potential confounders with the 10% rule. Specifics of the logistic regression model used in this and subsequent analyses are presented in
Table 2.
The association between parental bipolar disorder and behavioral disinhibition was even stronger among the offspring of parents with bipolar I disorder: 12 of 18 (67%) versus 83 of 244 (34%) (odds ratio=5.01, 95% CI=1.84–13.62).
The rate of behavioral disinhibition in the offspring of parents with bipolar I disorder was significantly higher than that in the offspring of parents with panic disorder plus major depression: 12 of 18 (67%) versus 35 of 99 (35%) (odds ratio=5.23, 95% CI=1.84–14.90) and that in the offspring of comparison parents: 12 of 18 (67%) versus 24 of 81 (30%) (odds ratio=6.91, 95% CI=2.37–20.21) with child sex and parental antisocial personality, conduct disorder, ADHD, and psychoactive substance use disorders covaried. Because the division of groups included parental panic disorder in these models, parental panic disorder was not considered a potential confounder.
In contrast, the rate of behavioral inhibition did not differ between the offspring of parents with and without bipolar disorder (consensus behavioral inhibition: 11 of 34 [32%] versus 76 of 244 [31%], respectively, odds ratio=0.99 [95% CI=0.44–2.24]). The lack of difference between groups was observed regardless of the definition of behavioral inhibition used. In these models, parental panic disorder was included as a relevant covariate, and socioeconomic status emerged as a potential confounder. However, because the equations were not significant, socioeconomic status was not covaried. Because all parents with bipolar disorder had also had depressive episodes, major depression could not be covaried. When we compared the offspring of unipolar depressives (N=141) with the offspring of parents with bipolar disorder (N=34), we found no difference in the rates of behavioral inhibition.
Discussion
The rate of laboratory-observed behavioral disinhibition among the 2–6-year-old offspring of bipolar parents was significantly elevated compared with the offspring of parents without bipolar disorder. The offspring of parents with bipolar I disorder had even higher rates of behavioral disinhibition. These associations were not accounted for by comorbid lifetime ADHD, conduct disorder, antisocial personality, or substance use disorders in the parents. In contrast, behavioral disinhibition was not significantly elevated among the offspring of parents with panic disorder or with unipolar depression. In addition, behavioral disinhibition was significantly higher among the offspring of parents with bipolar disorder I than among the offspring of parents with panic disorder plus comorbid unipolar depression. This finding suggests that the higher rate of behavioral disinhibition observed in the offspring of bipolar parents was not simply due to higher comorbidity in the parents.
In contrast, behavioral inhibition showed no significant association with parental bipolar disorder. This finding lends indirect support to the specificity of the familial association between behavioral inhibition and panic disorder
(32,
41), social phobia
(42), and unipolar depression
(32) because behavioral inhibition was not associated with bipolar disorder. We reported a similar negative association between parental alcohol and substance use disorders and behavioral inhibition in this group
(43). Our findings also stress the importance of parental comorbidity in affecting child outcomes because the panic disorder in these parents predicted behavioral inhibition, whereas bipolar disorder predicted behavioral disinhibition. These results underscore the importance of refining analyses of risk conferred by parental disorders in at-risk groups to consider the effects of comorbid disorders as well, in order to better understand differing trajectories of psychopathology.
It might be argued that the association between parental bipolar disorder and behavioral disinhibition is accounted for by the presence of ADHD in some of the children. However, although some of the disinhibited children may have already had ADHD
(11), the two constructs (behavioral disinhibition and ADHD) differ in important ways. Conceptually, behavioral disinhibition is regarded as an early marker of motivational dysregulation that may predispose children to develop any of several different disorders whose symptoms might include dysregulated behaviors (including ADHD, conduct disorder, mania, or substance abuse)
(28–
30). As a prodrome, it may share features of the disorders (e.g., extreme talkativeness in ADHD), which is to be expected because the prodrome evolves into the disorder. Moreover, methodologically, the assessment of behavioral disinhibition uses laboratory observations under standard conditions to quantify and contrast vocalizations and behaviors with those of normal comparison children, whereas assessment of ADHD relies upon parent or teacher reports or clinical impressions. Additionally, behavioral disinhibition can be assessed very early in childhood (e.g., at ages 2–3 years), before ADHD can be confidently diagnosed. Finally, only a minority of disinhibited children in the group were found to emerge with ADHD by age 5–6 years (24%)
(11).
The strengths of our study include the blindness of temperamental assessment and the use of standardized observational protocols that enable the assessment of behavioral disinhibition in young children without reliance on parent reports, which may be subject to bias. However, the study also has several important limitations. First, because we used a preexisting group of parents recruited for panic disorder and depression, the results may not generalize more broadly. Therefore, future work should use a case-control design selecting parents on the basis of bipolar disorder. Other limitations include the small size of the bipolar offspring group, the low representation of non-Caucasians, and the fact that temperamental assessments were conducted only once per child so that information about the stability of behavioral disinhibition was unavailable. Finally, it is important to accept with caution the negative findings because of low power to detect small effect sizes.
Despite these limitations, our pilot results support the hypothesis that behavioral disinhibition represents an early risk factor for bipolar disorder, in particular, bipolar I disorder. Clinically, our findings suggest that young offspring of bipolar parents who exhibit behavioral disinhibition should be monitored closely for the onset of disruptive behavior or mood disorder symptoms. They also raise the possibility that these children might be fruitfully targeted for early interventive efforts.