Positron emission tomography (PET) studies of antipsychotics, focusing in particular on dopamine D
2 receptor occupancy, have proven valuable in understanding the relationship between dose, clinical response, and D
2-related adverse events (e.g., extrapyramidal symptoms). Most of this work has involved oral antipsychotics
(17–
20), although at least one report with haloperidol decanoate has suggested that peak occupancies for the depot are in line with what is observed in oral formulations
(21).
Building upon the existing clinical evidence for long-acting risperidone, we set out to evaluate the D2 receptor occupancy of various doses using PET. The study was not designed as a clinical efficacy trial but rather was intended to provide occupancy data that, in the context of our current understanding, could provide additional in vivo evidence regarding appropriate dosing with this new formulation.
Method
Subjects were recruited from a multicenter study investigating the use of long-acting risperidone administered every 2 weeks at three different doses (25, 50, or 75 mg) in individuals with schizophrenia or schizoaffective disorder
(13). The PET investigation was approved by the Human Subjects Review Committee of the University of Toronto, and subjects provided written informed consent after receiving detailed information about the protocol.
Details of the multicenter trial have been published elsewhere, including design and clinical results
(13). Briefly summarizing, patients were candidates for a switch to long-acting risperidone if they met DSM-IV criteria for schizophrenia or schizoaffective disorder and had been stabilized on an oral antipsychotic regimen for at least 4 weeks. Exclusion criteria were current treatment with clozapine, presence of DSM-IV-defined substance abuse or dependence within the preceding 3 months, a neurological or medical condition that could adversely influence patient safety or evaluation, pregnancy, demonstrated lack of response to oral risperidone in the past, or concomitant medications that could compromise D
2 evaluation (e.g., nonantipsychotic agents with dopamine agonist or antagonist properties).
During a 2-week run-in phase, antipsychotics other than oral risperidone were discontinued and replaced with oral risperidone at flexible doses ranging from 1 to 6 mg/day. Thus, all subjects were receiving oral risperidone during this phase, and the dose of long-acting risperidone that they received thereafter was dependent on the oral risperidone dose at the end of the run-in phase. Specifically, they were assigned to one of the three doses of long-acting risperidone as follows: those receiving 1–2 mg/day or 3–4 mg/day of oral risperidone were assigned to the 25-mg and 50-mg doses of long-acting risperidone, respectively; subjects assigned to the 75-mg dose of long-acting risperidone were those receiving 5–6 mg/day of oral risperidone. Supplementary oral risperidone doses (1–6 mg/day) could be used for the first 2–3 weeks following the switch, although this was not required in any of the cases reported here.
Long-acting risperidone was administered every 2 weeks, and at least five consecutive injections were administered before PET was carried out. Participants were scanned twice during the 2-week injection interval: within 3 days following injection (postinjection) and within 5 days before the next injection (preinjection).
D
2 occupancy was established using [
11C]raclopride following the same procedure employed at our center and detailed previously
(22). PET scanning was conducted using a GEMS PC2048-Plus PET scanner (GE Medical Systems, Milwaukee) that produced 15 slices (thickness: 6.5 mm) with a resolution of about 5–6 mm in air. Patients were scanned lying down, with fixation of their heads achieved by use of a thermoplastic face mask (Tru-Scan Imaging, Annapolis, Md.).
Following injection of 10 mCi of high-specific-activity [
11C]raclopride (>300 Ci/mmol) using a bolus plus infusion protocol
(23–
26), a series of emission scans were obtained for 75 minutes. The regions of interest were the caudate/putamen, with the cerebellum used as a reference region. The regions of interest were drawn directly on averaged PET images and transferred to the dynamic PET images to obtain a time activity curve. An average of the striatum/cerebellum ratio minus one obtained between 30 and 75 minutes of scanning was taken as a measure of the equilibrium binding potential
(27). Receptor occupancy was then calculated as the percentage reduction of receptor binding potential with drug treatment relative to baseline, using age-corrected measures of binding potential from a previously collected dataset of unmedicated comparison subjects obtained with a similar methodology. This comparison group consisted of 22 healthy subjects and nine antipsychotic-naive patients with a diagnosis of schizophrenia or schizophreniform disorder (mean age=31.5 years, SD=8.51, range=19–47). Since the mean binding potential in the healthy subjects (mean=2.7, SD=0.4) did not differ significantly from that of the antipsychotic-naive subjects (mean=2.9, SD=0.4) (t=0.98, df=29, p=0.30), the data from the two groups were combined to obtain the regression equation for the age-matched estimate of binding potential in the occupancy calculation (binding potential=age ×0.03 + 3.8; R
2=0.6).
Venous blood was drawn for drug and prolactin concentrations at the time of the PET scans. For risperidone, blood samples were collected in heparinized tubes and centrifuged for 10 minutes at 2500 rpm within 2 hours of collection. Separated plasma was stored at –20°C for transport, and concentrations of risperidone plus 9-hydroxyrisperidone were determined by means of a validated radioimmunoassay method
(11). Prolactin levels were determined by using a two-site chemiluminometric immunoassay with a minimal detectable limit of 0.3 ng/ml and a coefficient of variance of 3.6%–4.5% (ACS, CIBA-Corning Diagnostics, East Walpole, Mass.).
Statistical analyses were carried out using SPSS (SPSS Inc., Chicago). Bivariate correlation analysis was used to examine the relationship between the primary variables of interest. Nonlinear regression analysis was used in the estimation of plasma risperidone plus 9-hydroxyrisperidone level associated with 50% D2 receptor occupancy.
Results
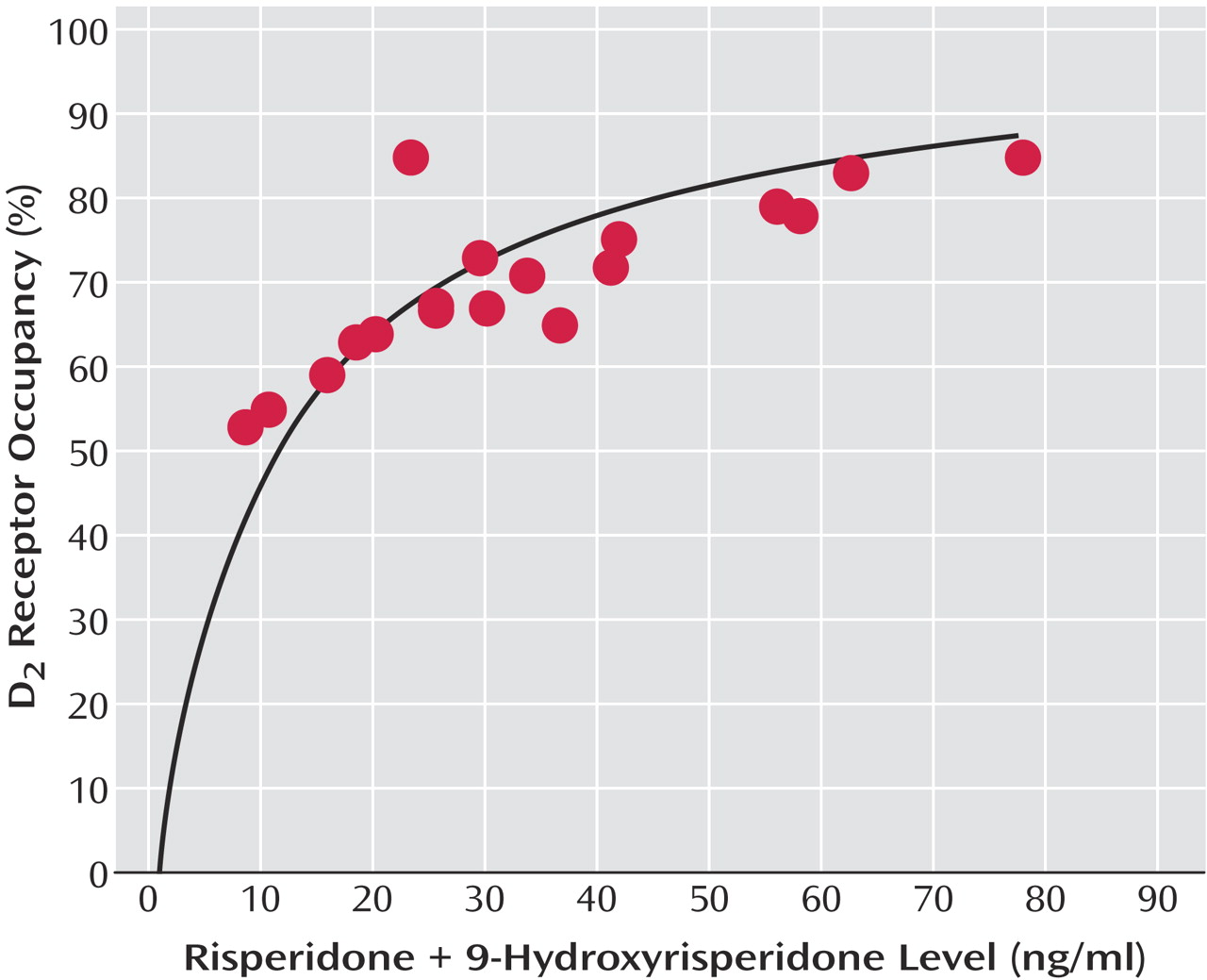
Nine participants (seven men and two women) completed the study. The group’s mean age was 34 years (SD=9, range=21–46), and the dosage breakdown was as follows: 25 mg (N=2), 50 mg (N=5), and 75 mg (N=2).
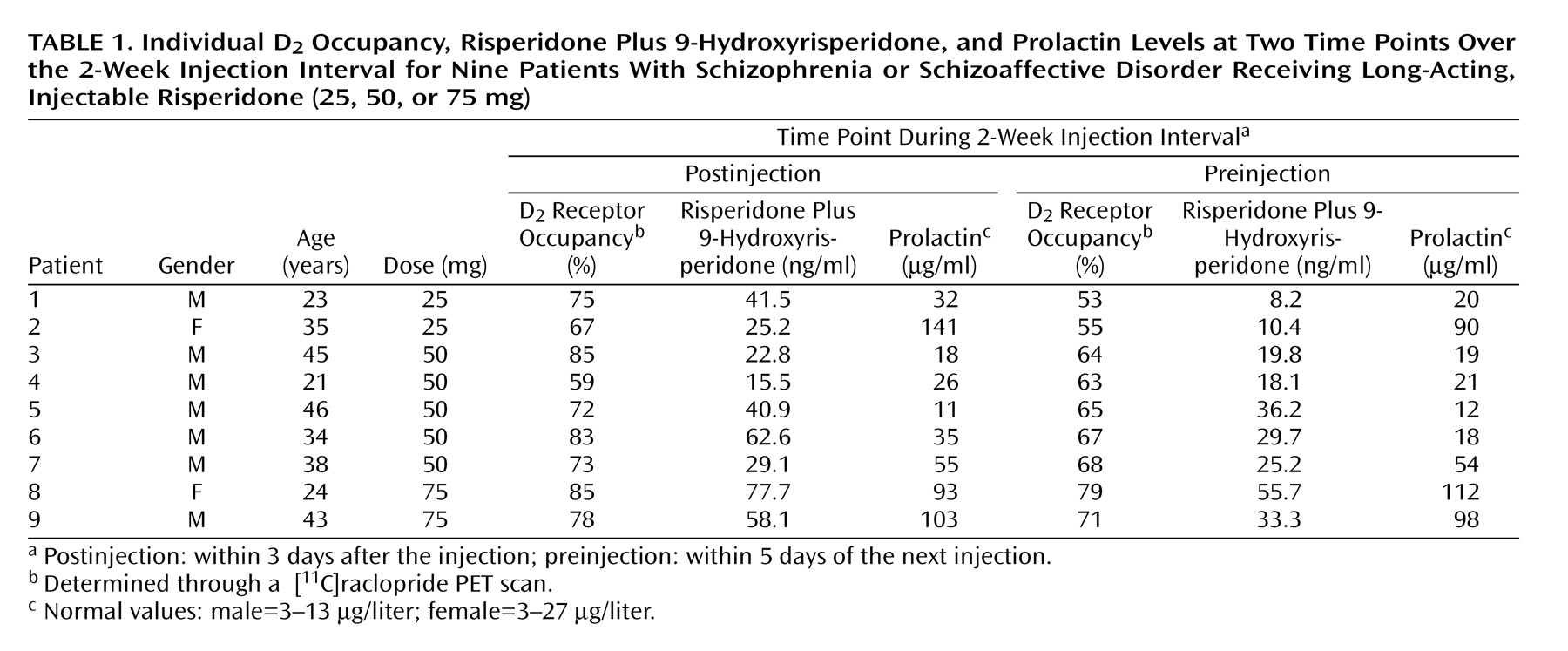
As seen in
Figure 1, D
2 occupancy levels, measured at the two time points (postinjection and preinjection) over the 2-week injection interval, increased in a dose-dependent fashion (25 mg: mean=71.0% [SD=5.7] and 54.0% [SD=1.4], respectively; 50 mg: mean=74.4% [SD=10.4] and 65.4% [SD=2.1]; 75 mg: mean=81.5% [SD=5.0] and 75.0% [SD=5.7]). Conversely, a comparison across all doses over the two time points indicated a significant reduction in both D
2 occupancy (t=3.67, df=8, p=0.006) and plasma concentrations of risperidone plus 9-hydroxyrisperidone (t=3.35, df=8, p=0.01). Eight of nine participants showed an expected decline in both of these measures over the course of the injection interval (
Table 1). One participant showed a small increase in occupancy that paralleled a modest increase in plasma levels (patient 4), but given the test-retest standard deviation of 6% in our lab this change is not significant.
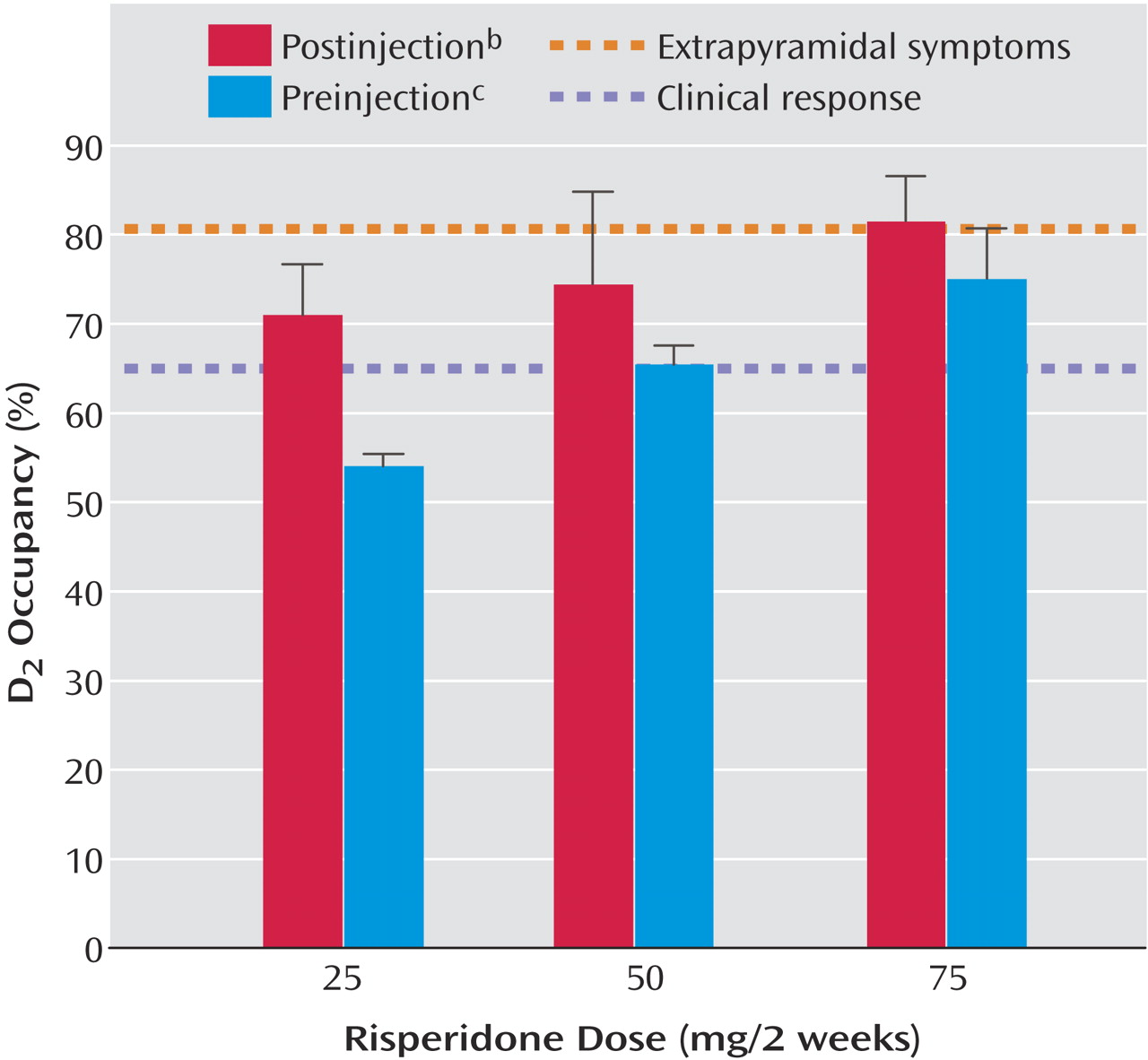
Dose showed a significant correlation with plasma risperidone plus 9-hydroxyrisperidone concentrations (r=0.63, df=7, p=0.006), even after we controlled for time (r=0.69, p=0.002). The relationship between plasma concentration and D
2 occupancy was captured by a saturating hyperbola (B
max constrained to 100%), with the estimated plasma concentration associated with 50% D
2 occupancy (ED
50) being 11.06 ng/ml (95% confidence interval=9.15–12.96) (
Figure 2).
Mean prolactin values at the two time points (postinjection and preinjection) over the 2-week injection interval were 57.11 μg/liter (SD=44.97) and 44.59 μg/liter (SD=38.30), respectively, representing a nonsignificant difference (t=0.74, df=23, p=0.47). There was no significant correlation between prolactin concentrations and plasma concentrations of risperidone plus 9-hydroxyrisperidone (r=0.32, p=0.12) or D2 receptor occupancy (r=0.34, p=0.10).
We sampled only a small subgroup of the larger clinical sample, and the specific findings of the latter have been reported elsewhere
(13). All subjects participating in the PET study either remained stable or showed clinical improvement during the trial, with the exception of one individual (patient 8) who showed a 1-point Clinical Global Impression deterioration. Extrapyramidal symptom scores, as measured by the Extrapyramidal Symptom Rating Scale, remained low in all dose groups throughout the PET study.
Discussion
With any new medication, it is critical that guidelines regarding optimal dosing be established. Previous PET data have indicated that optimal clinical response occurs when at least 65% of striatal D
2 receptors are occupied, while the risk of extrapyramidal symptoms increases notably at D
2 occupancy levels above 80%
(17,
18). The present findings indicate that long-acting injectable risperidone, even at a dose of 25 mg every 2 weeks, exceeds the threshold associated with clinical response. As expected, D
2 occupancy was dose-dependent, with only the highest dose employed (75 mg) approximating the threshold that has been associated with extrapyramidal symptoms in previous studies.
These findings suggest that for most patients treated with long-acting risperidone, clinical efficacy should be expected at doses of 25–50 mg. This corroborates the existing clinical evidence showing no additional clinical benefit at higher doses
(14). Moreover, our PET results suggest that dosing at 75 mg every 2 weeks may be associated with some degree of increased risk of extrapyramidal symptoms, supporting the observation of a dose-dependent risk of extrapyramidal symptoms in the clinical setting
(14).
Mean D
2 occupancy levels toward the end of the injection interval for the 50- and 75-mg doses exceeded 65%, while for the 25-mg dose the end-of-interval occupancy level was 54%. At first glance, these data might be seen as suggesting that individuals receiving 25 mg would be vulnerable to relapse toward the end of the injection interval. However, maintenance of D
2 occupancy levels above the 65% threshold may not be necessary for clinical response. It has been shown, for example, that individuals can be stabilized on a regimen of haloperidol decanoate administered every 4 weeks, despite mean D
2 occupancy levels decreasing from 73% (range=60%–82%) at week 1 to 53% (range=20%–74%) at week 4 (21). Indeed, there is a growing body of evidence to suggest that there may be clinical advantages to avoiding sustained, high D
2 blockade
(28).
Previous work from our center with oral risperidone, which evaluated the relationship between D
2 occupancy and risperidone plus 9-hydroxyrisperidone, established an ED
50 of 6.08 ng/ml (95% CI=4.8–7.3) (29). In contrast, the calculated ED
50 here was 11.06 ng/ml (95% CI=9.15–12.96). This discrepancy may reflect study group size: in the first report the curve was established based on nine data points, including one significant outlier, whereas the current estimate was constructed from twice as many data points. There are well-recognized concerns regarding the impact of inter- and intraindividual variability in plasma antipsychotic levels and efforts to establish “therapeutic windows”
(30–
32). Bearing in mind this caveat, the current estimate actually dovetails nicely with a more recent review of this topic suggesting an optimal therapeutic range for risperidone plus 9-hydroxyrisperidone of 20–60 ng/ml
(33). As seen in
Figure 2, 20 ng/ml is associated with 65% D
2 occupancy, while 60 ng/ml represents 84% D
2 occupancy. Thus, the lower level meets the threshold associated with optimal clinical response, whereas the upper limit is just over the threshold linked to increased extrapyramidal symptom risk
(18), which in turn may compromise clinical outcome.
The lack of correlation between prolactin and D
2 occupancy was not entirely unexpected, since factors mediating prolactin secretion are complex
(34). Our own examination of this issue has in the past provided mixed results
(17,
22), and efforts to establish a threshold for hyperprolactinemia in the same fashion as clinical response and extrapyramidal symptoms have not met with the same degree of agreement
(17,
35).
A comment is warranted regarding timing of the PET scans in this study and the actual pharmacokinetics of long-acting risperidone. The two points used here were chosen to reflect the time frame of the recommended 2-week injection interval, and in so doing provide a reflection of occupancy through the cycle of treatment at steady state. This needs to be distinguished, however, from the actual pharmacokinetics of single- and multiple-dose long-acting risperidone
(11). According to single-dose data an injection’s peak occurs approximately 4–6 weeks later, meaning that the main release phase is not observed until after several injection intervals. Over the course of an injection interval at steady state, concentrations of the active moiety (C
max to C
min) decrease by approximately 50%–60%, and while this rate of decrease is notably greater than what is observed in terms of changes in D
2 occupancy, we are reminded that a significant dissociation between brain and plasma kinetics in this regard has been reported with antipsychotics
(36).
At least several limitations qualify our conclusions. PET studies of this sort involve limited numbers of patients, much smaller than what would be required to definitively analyze the relationship between dose/receptor occupancy and response/side effects. As a result, to make clinical inferences we must extrapolate the D
2 occupancy data to other larger clinical trials
(13,
14). In addition, by focusing on the D
2 story we do not address the potential contribution of other receptors and systems in a class of medications that are best characterized by their pharmacological heterogeneity
(37–
39). Even confining our comments to D
2, the use of [
11C]raclopride as the ligand focuses on striatal D
2 receptor occupancy. However, it can be argued that D
2 receptor occupancy in other areas is involved in clinical response and that, further, there is evidence that atypical agents may show differential D
2 occupancy between striatal and extrastriatal regions
(40–
47). However, having raised each of these concerns, we are somewhat reassured by the fact that the present data are in line with existing clinical trial and plasma drug data
(13,
14,
33) as well as recently published PET data from another center
(48).
In this particular study, patients were first switched to oral risperidone and then to the depot risperidone formulation on the basis of the final oral dose. Establishing comparable doses between the two formulations is complicated by the more complex pharmacokinetics of long-acting risperidone and differences in bioavailability. However, the PET data now available lend support to the position that long-acting risperidone doses of 25–75 mg are in line with oral risperidone doses of 2–6 mg
(48).
In summary, the PET findings reported here support available clinical evidence indicating that dosing long-acting risperidone at 25–50 mg every 2 weeks is sufficient in attaining clinical response with minimal risk of extrapyramidal symptoms. In addition, they provide further data regarding the relationship between plasma drug levels and D2 occupancy. Having this information may assist clinicians as they familiarize themselves with long-acting injectable risperidone and incorporate it into their clinical practice.