Controversy surrounds the diagnosis of pediatric bipolar disorder. Specifically, the nosological status of children with irritability and hyperarousal, designated here as severe mood dysregulation, is debated
(1) . Prior work demonstrates that relatives of youth with bipolar disorder are more likely to be diagnosed with bipolar disorder than are relatives of youth without bipolar disorder
(2,
3) . However, there are no data regarding parental diagnoses of youth with severe mood dysregulation. If severe mood dysregulation is a phenotype of bipolar disorder, then the parents of youth with severe mood dysregulation should have bipolar disorder as often as the parents of youth with narrow phenotype bipolar disorder.
Researchers have established a strong heritability for bipolar disorder. The concordance of bipolar disorder in monozygotic twins is 0.67–0.85, reflecting substantially greater concordance than in dizygotic twins or siblings
(4) . Childhood-onset bipolar disorder tends to be associated with a particularly strong family history
(5) . Faraone and colleagues
(2) found a fivefold elevated risk for bipolar disorder in the relatives of children with comorbid attention deficit hyperactivity disorder (ADHD) and bipolar disorder compared to ADHD youth without bipolar disorder, suggesting that ADHD with bipolar disorder is familially distinct from ADHD presenting alone. Similarly, bipolar disorder is significantly more common in the relatives of youth with bipolar disorder compared to the relatives of children with anxiety or comparison subjects
(3) .
However, controversy surrounding the diagnosis of bipolar disorder in children complicates the interpretation of findings regarding the heritability and familiality of pediatric bipolar disorder
(1) . Specifically, some suggest that children with nonepisodic impairing irritability and hyperarousal symptoms, or severe mood dysregulation, constitute the “broad phenotype” of pediatric bipolar disorder
(1), although this is only one of several ways to operationalize “broad phenotype.” Others contend that pediatric bipolar disorder, like adult bipolar disorder, presents with an episodic pattern
(1) . Comparing diagnoses in the parents of youth with severe mood dysregulation to diagnoses in the parents of children meeting strict DSM-IV criteria for bipolar disorder, or narrow phenotype bipolar disorder, may help to elucidate the nosologic status of severe mood dysregulation.
Researchers have yet to compare DSM-IV diagnoses in parents of youth with narrow phenotype bipolar disorder versus parents of youth with severe mood dysregulation. However, studies using the criteria for severe mood dysregulation used here suggest that severe mood dysregulation and narrow phenotype bipolar disorder differ in their pathophysiology and clinical correlates
(6 –
8) . Children with severe mood dysregulation have an earlier age of onset and higher rates of ADHD and oppositional defiant disorder than children with narrow phenotype bipolar disorder, whereas youth with narrow phenotype bipolar disorder have more psychiatric hospitalizations and suicide attempts
(7) . Also, while both children with severe mood dysregulation and those with narrow phenotype bipolar disorder show attentional deficits during a frustration-inducing task, the nature of those deficits differs, with children with severe mood dysregulation demonstrating early information-processing deficits and youth with narrow phenotype bipolar disorder showing impairments in later executive attention
(6) .
We tested the hypothesis that bipolar disorder would be significantly more common in the parents of youth with narrow phenotype bipolar disorder than in the parents of youth with severe mood dysregulation. Our hypothesis was based on the strong clinical resemblance between narrow phenotype bipolar disorder and adult DSM-IV bipolar disorder and prior preliminary work suggesting a higher rate of bipolar disorder in the parents of children with episodic, as opposed to nonepisodic, irritability
(9) .
Method
The biological parents of patients with narrow phenotype bipolar disorder (proband N=33, parent N=42) and youth with severe mood dysregulation (proband N=30, parent N=37) gave written informed consent for this institutional review board-approved study at the National Institute of Mental Health (NIMH). The children gave written assent. The parents were interviewed by clinicians trained in the use of the Diagnostic Interview for Genetic Studies Version 3.0, which has been shown to generate a reliable (0.73–0.95) lifetime diagnosis of axis I disorders
(10) . The interviewing clinicians were blind to the child’s diagnostic status, and the parents were counseled not to discuss their child during the interview.
Child diagnoses were made with the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL)
(11), a semistructured diagnostic interview administered to parents and children separately. The interviewers were graduate-level clinicians with excellent interrater reliability (kappa >0.9, including differentiating severe mood dysregulation from narrow phenotype bipolar disorder). Different clinicians interviewed the children and parents, and diagnoses were based on best-estimate procedures. The clinicians also reviewed children’s medical records and consulted with treating psychiatrists and/or therapists.
Youth with narrow phenotype bipolar disorder met strict DSM-IV criteria for bipolar disorder, with at least one full-duration hypomanic or manic episode with an abnormally elevated or expansive mood and/or grandiosity and at least three “B” mania symptoms
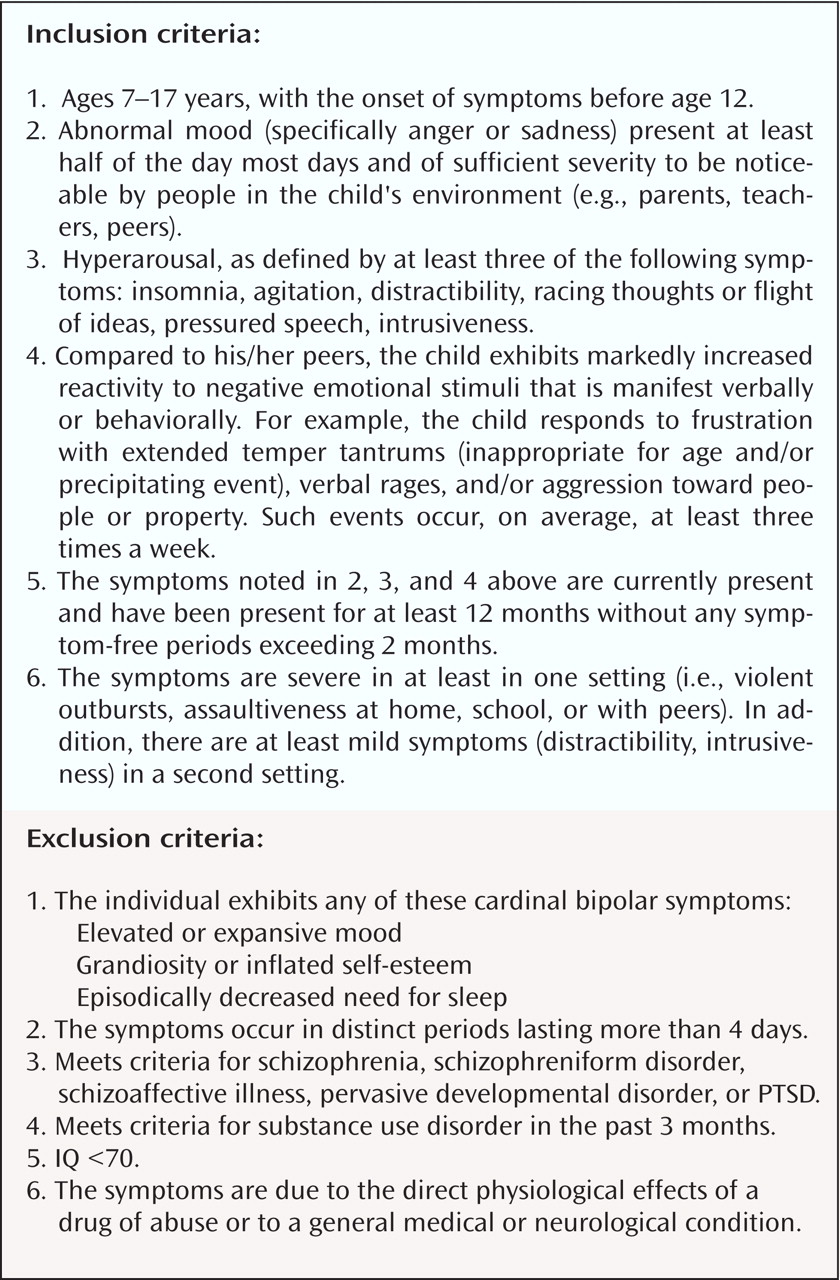
(1) . Briefly, children with severe mood dysregulation had 1) an abnormal baseline mood (i.e., irritability, anger, and/or sadness), 2) hyperarousal symptoms (i.e., at least three: insomnia, agitation, distractibility, racing thoughts or flight of ideas, pressured speech, intrusiveness), 3) increased reactivity to negative emotional stimuli (e.g., temper outbursts) at least three times per week, 4) symptom onset before age 12, 5) symptoms for at least a year without symptom-free periods lasting more than 2 months, and 6) functional impairment in at least two of three domains (i.e., home, school, peer relationships) (for complete criteria, see
Figure 1 ). Severe mood dysregulation diagnoses were made by using a module of questions in K-SADS-PL format operationalizing the criteria for severe mood dysregulation defined in Leibenluft et al.
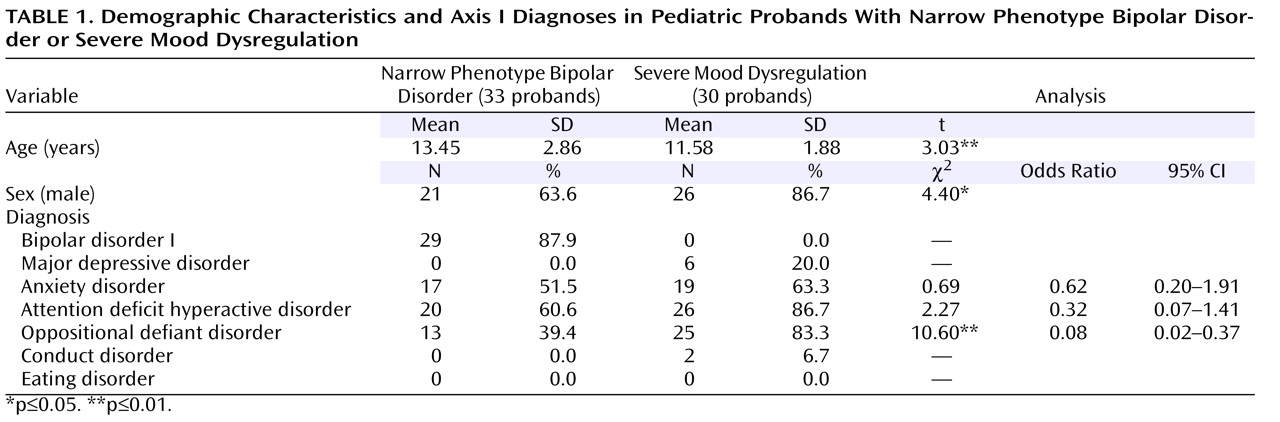
(1) . Children with an IQ <70, pervasive developmental disorder, or substance use were excluded from both groups. (For demographic and clinical information on the child probands, see
Table 1 ).
Because some observations were nonindependent (i.e., more than one parent per child), we used a mixed-model approach for binary/categorical data following SAS GENMOD statistical analysis procedures
(12) . Of the 42 parents of children with narrow phenotype bipolar disorder, 24 were derived from independent child probands, and the remaining 18 were derived from nine child probands. Of the 37 parents of children with severe mood dysregulation, 23 were derived from independent child probands, and the remaining 14 were derived from seven child probands. Logistic regressions were used to compute odds ratios comparing the rate of axis I diagnoses in the parents of probands with narrow phenotype bipolar disorder or severe mood dysregulation, with age covaried because the parents of narrow phenotype bipolar disorder youth were significantly older than the parents of youth with severe mood dysregulation. Odds ratios were also used to compare the rate of axis I diagnoses in the probands. Here, child age and gender were covaried because youth with narrow phenotype bipolar disorder were older than youth with severe mood dysregulation and there were more boys in the severe mood dysregulation group compared to the narrow phenotype bipolar disorder group. Significance was set at p<0.05.
Results
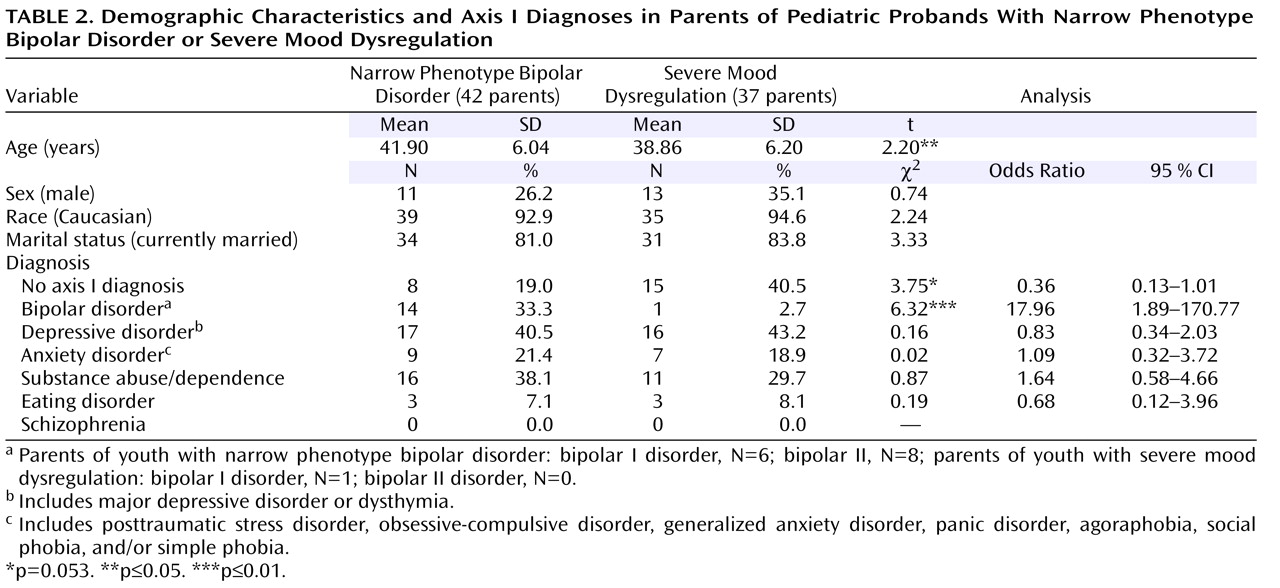
The parents of youth with narrow phenotype bipolar disorder and youth with severe mood dysregulation did not differ on race, marital status, or sex; however, the parents of youth with narrow phenotype bipolar disorder were significantly older than the parents of youth with severe mood dysregulation, so age was included as a covariate (
Table 2 ). Compared to the parents of children with severe mood dysregulation, the parents of children with narrow phenotype bipolar disorder were significantly more likely to be diagnosed with bipolar disorder (odds ratio=17.96, CI=1.89–170.77, p=0.01) (
Table 2 ). Overall, 19.0% of the parents with narrow phenotype bipolar disorder and 40.5% of the parents with severe mood dysregulation had no axis I diagnosis (odds ratio=0.36, CI=0.13–1.01, p=0.053). Parental diagnoses of major depressive disorder, anxiety disorder, substance abuse or dependence, eating disorder, or schizophrenia did not differ by group (all p>0.50). The rate of oppositional defiant disorder differed between youth with severe mood dysregulation and narrow phenotype bipolar disorder (see
Table 1 ). There were no associations between parental diagnoses (e.g., substance abuse/dependence) and child proband comorbidities (e.g., ADHD).
Discussion
The diagnosis of pediatric bipolar disorder has generated substantial debate, focusing on children with nonepisodic, impairing irritability and hyperarousal, or severe mood dysregulation. Although severe mood dysregulation has been referred to as a broad bipolar disorder phenotype
(1), its nosologic relationship to bipolar disorder remains an unanswered empirical question. The purpose of this study was to assess diagnoses in the parents of probands with narrow phenotype bipolar disorder or severe mood dysregulation systematically, with a particular focus on the prevalence of parental bipolar disorder.
Of note, bipolar disorder was the only diagnosis whose prevalence differed between parent groups; 33.3% (N=14) of youth with narrow phenotype bipolar disorder had a parent with bipolar disorder, compared to 2.7% (N=1) of the parents of youth with severe mood dysregulation. Our rate of bipolar disorder in the parents of youth with narrow phenotype bipolar disorder was similar to that of Birmaher et al.
(13), in which 29.5% of first-degree relatives of children with bipolar disorder I had a history of mania, and Strober et al.
(14), in which 29.4% of the first-degree relatives of children with prepubertal-onset bipolar disorder had a bipolar disorder diagnosis. Taken together, these data confirm reports that the familiality of pediatric bipolar disorder is high
(4) . Our data extend these results by suggesting that narrow phenotype bipolar disorder and severe mood dysregulation are distinct in terms of familial aggregation.
There are five important limitations to this work. Our data may be subject to ascertainment bias; parents with bipolar disorder may be more likely to bring their child to NIMH, inflating the rate of parental bipolar disorder. However, the same bias should influence parents with bipolar disorder whether their child had severe mood dysregulation or narrow phenotype bipolar disorder. Second, our group was small. Third, second-degree relatives were not assessed. Fourth, because the purpose of the study was to compare bipolar disorder in the parents of children with narrow phenotype bipolar disorder versus those with severe mood dysregulation
(1), we did not include a comparison group of parents with unaffected offspring. Of note, the rate of bipolar disorder in the parents of youth with severe mood dysregulation resembles a recent 3.9% estimate of lifetime prevalence of bipolar disorder in the adult population
(15) . Fifth, given the structure and focus of the Diagnostic Interview for Genetic Studies Version 3.0, ADHD and other disruptive behavior disorders were not assessed in the parents; these might have differentiated the two parent groups. Future research could address the limitations of this study.
In sum, we found that the familial aggregation of narrow phenotype bipolar disorder with adult DSM-IV bipolar disorder is high, and the rate of bipolar disorder is significantly higher in parents of youth with narrow phenotype bipolar disorder than in parents of youth with severe mood dysregulation. These data suggest that severe mood dysregulation and narrow phenotype bipolar disorder are distinct entities and that it may not be warranted to diagnose children with nonepisodic irritability as having bipolar disorder. Future research should continue to examine the nosological status of severe mood disorder by comparing the pathophysiology, longitudinal course, and clinical correlates of youth with narrow phenotype bipolar disorder and youth with severe mood dysregulation.