The large-scale involvement of people with mental disorders in the criminal justice system is an important national problem. The proportion of people entering U.S. jails who have severe mental disorders has been estimated to be between 6% and 15%
(1,
2), and the number of jail admissions involving people who have severe mental disorders has been estimated to be around 804,000 annually
(3) . People with mental disorders who are incarcerated tend to stay longer in jail than others charged with similar crimes and to cycle through the criminal justice system, the mental health system, and substance abuse treatment programs
(4,
5) . The President’s New Freedom Commission on Mental Health identified reducing unnecessary criminalization of people with mental disorders as a priority
(6) .
To reduce recidivism among people with mental disorders, many communities have created specialized mental health courts in recent years. In contrast to traditional courts, mental health courts have therapeutic goals, such as increasing adherence to treatment and decreasing involvement in the criminal justice system. Nationwide, mental health courts have proliferated rapidly, from two in operation in 1997 to about 90 in 2005, operating in 34 states
(7) . Despite the widespread implementation of mental health courts, few studies have evaluated whether they can reduce criminal recidivism among people with mental disorders
(8 –
12) .
Although the structure of mental health courts varies across jurisdictions, common features include a separate docket for defendants with mental disorders; a designated judge (and typically also designated prosecution and defense counsel); and a nonadversarial team approach involving cooperation and joint decision making between criminal justice and mental health professionals
(13,
14) . Participation is voluntary, with defendants agreeing to follow a treatment plan and be monitored by the court with the expectation of a reduction in charge or sentencing. The court team attempts to find treatment and services and to provide supervision aimed at each client’s specific clinical problems while protecting the public. Access to the earliest mental health courts was restricted to persons charged with nonviolent misdemeanors
(10) . A recent survey
(15) identified the advent of a second generation of mental health courts that include or even emphasize mentally ill offenders charged with felonies. Few data are available, however, on whether courts that accept people with more serious charges can function without compromising public safety. In this article, we describe an evaluation of the criminal justice outcomes of the San Francisco mental health court, in which a substantial proportion of defendants were charged with felony offenses.
The San Francisco mental health court, called the Behavioral Health Court, was established in early 2003. Its mission is to connect criminal defendants who have serious mental illness to treatment services, to find dispositions to their criminal charges that take mental illness into consideration, and to decrease their chances of returning to the criminal justice system. The court aims to intensely monitor a subset of mentally ill offenders whose criminal behavior is directly linked to their mental illness. Criminal proceedings are not dismissed while defendants are in the program, nor are they dismissed automatically if defendants successfully complete it. To qualify for mental health court, defendants must be diagnosed as having a DSM-IV axis I mental disorder or, in some circumstances, developmental disabilities, and they must be amenable to treatment in the community mental health system. The court anticipates that relapses may occur, and it emphasizes positive reinforcement for successes rather than sanctions for failures. Participants who successfully maintain a sustained period of stability “graduate” from the mental health court.
The design of this study was affected by the fact that in evaluating programs in criminal justice settings, randomized controlled trials are often precluded by the concern that withholding enhanced services is unfair to those not selected for the active treatment. A method that can attenuate the biasing effects of nonrandom assignment to treatment versus comparison groups is propensity score weighting
(16,
17) . The propensity score refers to the probability, given a set of observed characteristics or covariates (such as demographic, clinical, and criminal history variables), that an individual will be selected for treatment. Under certain assumptions
(18), propensity weighting can reduce confounding between treatment effects and pretreatment risk factors when comparing groups in an observational study
(19 –
22) .
In this study we compared the criminal justice outcomes of individuals who entered the San Francisco mental health court during its first 22 months of operation with outcomes of others who were concurrently potentially eligible for consideration for selection into the mental health court—that is, other individuals with mental disorders who entered the San Francisco jail during the same period. We used propensity weighting to correct for baseline differences between defendants who did and did not participate in mental health court. Our primary research question was: To what extent does participation in the mental health court reduce the probability of recidivism? We hypothesized that participation in the mental health court would be associated with a longer time without any charges for new crimes and without charges for new violent crimes compared with nonparticipation. We also hypothesized that individuals who graduated from the mental health court would have a longer time without new charges after successfully completing the program than comparable persons whose cases had been adjudicated in regular court.
Method
The study involved review of deidentified administrative databases associated with the San Francisco county court and jail systems. The protocol was approved by the relevant institutional review boards. Since the project used deidentified data, the institutional review boards affirmed that informed consent was not necessary.
Study Population
Between January 14, 2003, and November 19, 2004, a total of 8,325 individuals 18 years of age or older who were diagnosed as having a mental disorder entered the San Francisco jail. Of these, 172 persons entered the mental health court; we studied the 170 individuals among them for whom complete data, including at least 6 months of follow-up, were available. Our comparison or treatment as usual group consisted of the 8,067 persons with complete data among the remaining 8,153 persons.
Variables
For the mental health court group, we defined the baseline period as the 12 months before the date of entry to the program. For the treatment as usual group, we defined the baseline period as 12 months before the date of the first arrest that occurred between January 14, 2003, and November 19, 2004 (we designated this arrest as the index arrest). Follow-up data for both groups were obtained through May 27, 2005.
We extracted data on age, gender, ethnicity, and homelessness from the databases. For criminal charges, we classified charges as violent or not violent. Following Naples and Steadman
(23), we categorized charges according to concepts developed by the MacArthur Study of Mental Disorder and Violence
(24) . We defined violence as a charge involving an act of physical aggression against other people, threatening others with a lethal weapon, or a sexual assault. In cases of multiple charges, we categorized arrests according to the most severe charge related to the arrest.
We obtained diagnostic information for all persons diagnosed as having a mental disorder by the jail’s psychiatric services during the study period. On entry into jail, every detainee undergoes an initial medical screening by a registered nurse, followed by a more detailed medical screening 1–2 hours later by another nurse. Individuals identified as having a possible psychiatric problem are referred for evaluation by mental health staff. Psychiatric diagnoses are based on DSM-IV.
Our outcome variables were measures of recidivism. We operationalized recidivism as rearrest for two categories of new charges: any offense and violent crimes.
Statistical Analysis
Our primary research objective was to determine whether participation in mental health court was associated with a longer time without recidivism compared with treatment as usual. Our general statistical approach involved time-to-event analysis (i.e., survival analysis) using the Cox proportional hazards model
(25) .
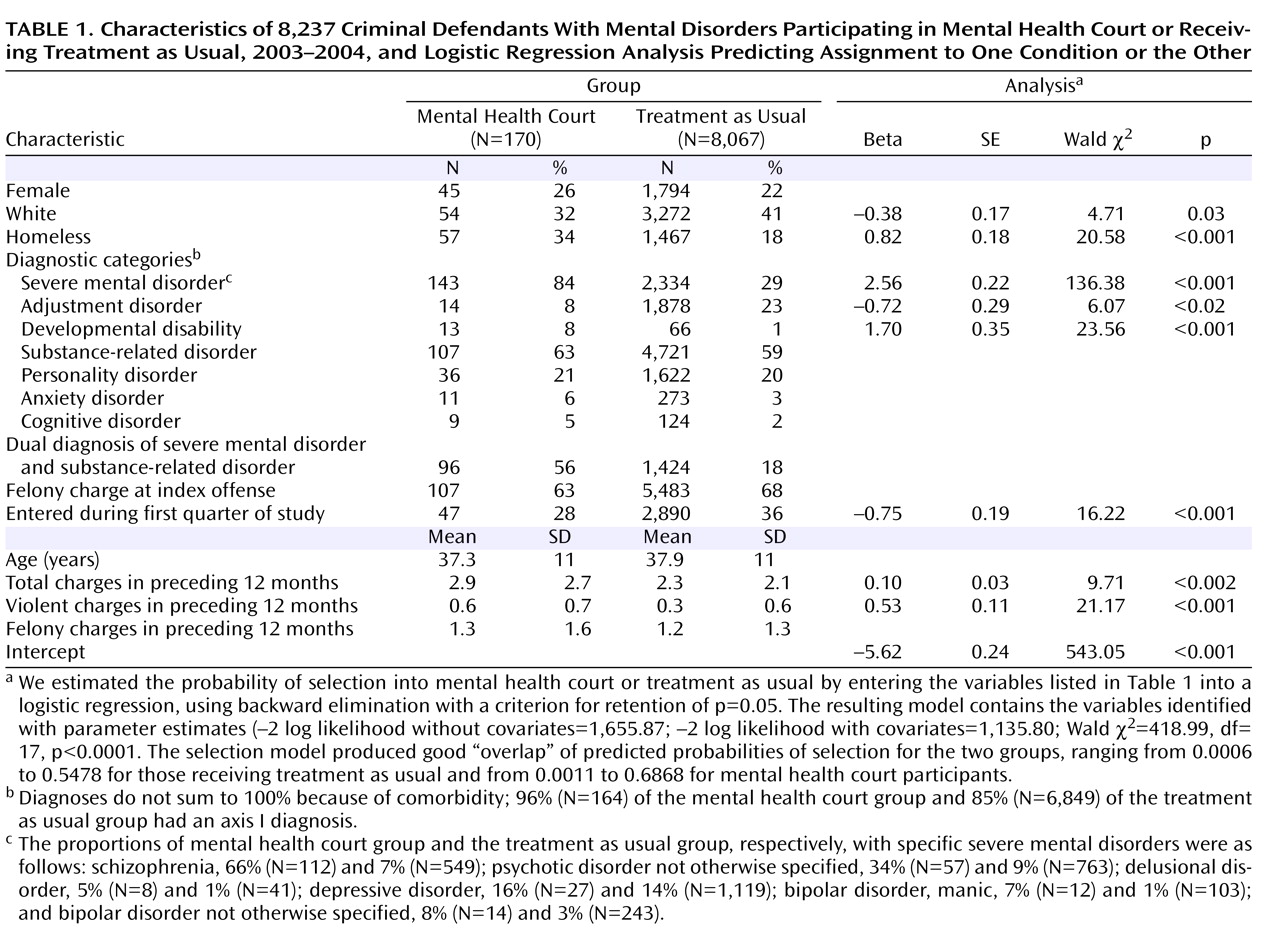
Potential Confounding Variables
Since the risk of recidivism may be affected by pretreatment variables, it was necessary to control for them statistically to estimate the reduction in risk of recidivism that was attributable to participation in the mental health court. We considered a variety of variables related to baseline demographic characteristics, criminal history, and psychiatric diagnosis as control variables (see
Table 1, including its footnote on diagnoses). Given the possibility that these variables could have a different relationship with recidivism depending on whether or not individuals received active treatment, our Cox models also evaluated for interactions between them and mental health court participation.
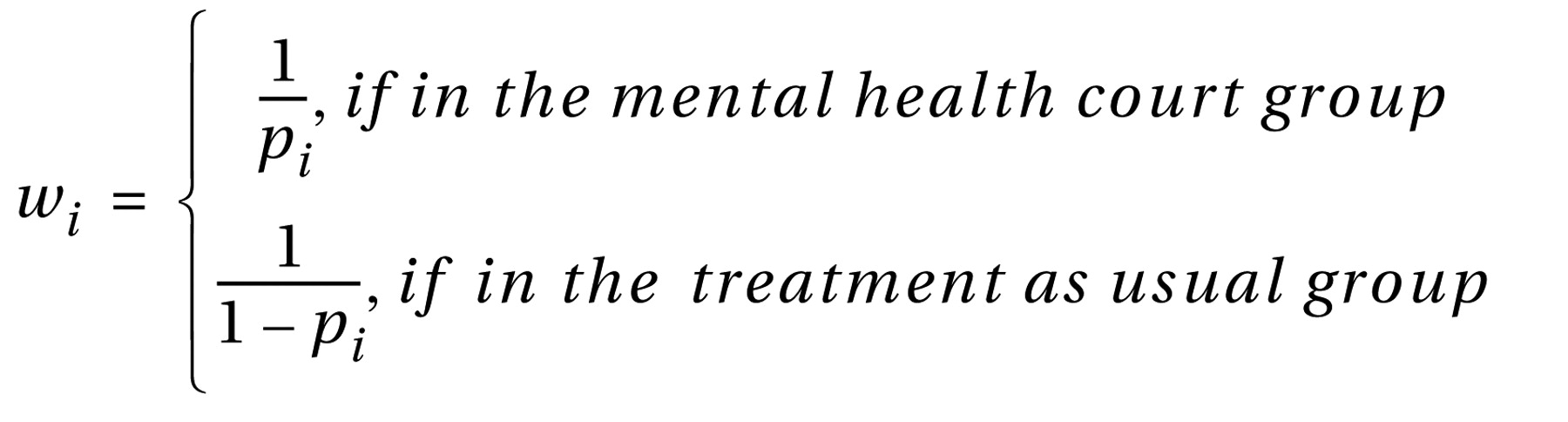
Controlling for Nonrandom Assignment
Because this was an observational study with nonrandom assignment, simple comparisons between the mental health court and treatment as usual groups could produce misleading results as a result of selection bias. Individuals in these groups may differ in baseline characteristics that are associated with both selection to mental health court and future arrest. To address this issue, our comparison of the mental health court and treatment as usual groups used a method of propensity weighting following the general two-step approach recommended by Hirano and Imbens
(26) . First, using logistic regression, we modeled the probability of being selected for mental health court as a function of a set of demographic variables, clinical variables, and criminal charges during the 12 months before entering the program. We used backward elimination with a criterion for retention of p=0.05 to determine the subset of variables for the selection model. From this model, we estimated the probability of selection into mental health court,
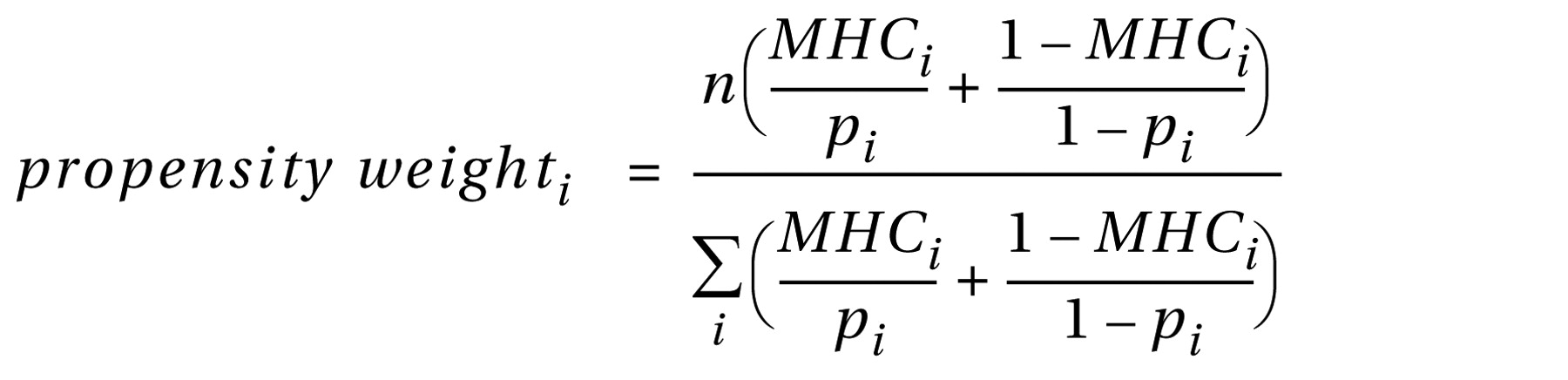
p i , for each individual in the sample. We then formed a propensity weight,
w i , for each individual using the inverse of the estimated probability of selection, according to the rule:
Second, to estimate the specific reduction in risk of recidivism that was associated with mental health court participation while concurrently taking into account the presence of other risk factors, we used a weighted Cox regression model, with weights equal to normalized versions of the propensity weights—normalized so that the weights sum to the sample size:
where
n indicates the sample size and
MHC i indicates whether or not the
i th individual was in the mental health court group (
MHC i =0 if the individual was in the treatment as usual group, and
MHC i =1 if the individual was a mental health court participant). This represents an application of the Hirano and Imbens
(26) propensity-weighted regression approach to the Cox model. Essentially, this procedure downweights cases with very low or very high estimated probabilities of selection to mental health court and matches cases according to their estimated propensity scores. As long as there is overlap in the values of observed covariates related to selection, this procedure minimizes the effect of imbalance due to these covariates and can be shown to yield results that are asymptotically equivalent to those that would be obtained with balanced data from a randomized design
(16,
18,
26) . Our propensity weighting procedure effectively creates a sample with cases matched by similar likelihoods of being selected for mental health court.
This procedure was carried out separately for analyses of time to any new charge and time to a new violent charge. Both Cox regression models included an indicator for mental health court participation; control variables consisting of demographic characteristics, diagnosis, and baseline criminal history; and interactions between the control variables and mental health court participation, centered on their respective sample mean values. This centering was done so that the coefficient of the main effect of mental health court participation could be interpreted as the average individual treatment effect of mental health court participation on the logarithm of the hazard function. Backward elimination, using a p value of 0.05 for retention, was used for selection of control variables for inclusion in the Cox models.
Based on the Cox regression models, we estimated the probability of recidivism as a function of time since baseline—the so-called failure function (1 – survival function). Specifically, we estimated the average treatment effect due to mental health court participation on the failure function while controlling for the above-mentioned confounding variables. To estimate the average treatment effect and its standard error, we followed the approach developed independently by Terza
(27,
28) and Basu and Rathouz
(29) . (Details are presented in the data supplement accompanying the online version of this article.)
Intent-to-Treat Analyses
Our primary survival analyses compared all those in the mental health court group with those in the treatment as usual group, from the time of enrollment to the end of the follow-up period, without distinguishing whether individuals successfully completed the mental health court program.
Outcomes Associated With Completion of the Mental Health Court Program
To determine whether changes associated with mental health court participation were maintained after successful completion of the program, we conducted survival analyses comparing recidivism after graduation for those who successfully completed the program with recidivism in the treatment as usual group. We analyzed the data using SAS, version 9.1.3 (SAS Institute, Cary, N.C.).
Results
Sample Characteristics
As shown in
Table 1, the index offense was a felony for about two-thirds of both the mental health court group and the treatment as usual group.
Twelve-month follow-up data were available for 139 mental health court participants and 6,606 individuals in the treatment as usual group. The median time that mental health court participants spent in the program was 8.3 months. By the end of the follow-up period, of the 170 individuals who had enrolled in the mental health court program, 81 (48%) had graduated, 45 (26%) were still in the program, and 44 (26%) had left the court for other reasons: 11 voluntarily opted out, five were removed by the court because of arrests for new charges, 11 were removed by the court for noncompliance, and 17 left for other reasons. (Although five people were removed by the mental health court because of arrests for new charges, rearrest did not necessarily result in removal from the program.)
Controlling for Nonrandom Assignment
As described above, to reduce the impact of nonrandom assignment to mental health court on analyses of the effect of mental health court participation on recidivism, we first estimated propensity scores by entering the baseline clinical, demographic, and criminal history variables listed in
Table 1 into a logistic regression model of assignment to mental health court or treatment as usual. The resulting model contains the eight variables identified with parameter estimates in
Table 1 . Selection for mental health court was associated with the presence of severe mental disorders (e.g., schizophrenia, delusional disorder, psychotic disorder not otherwise specified, bipolar disorder, and depressive disorders) and developmental disabilities; persons with adjustment disorders were less likely than others to be selected for mental health court. Selection for mental health court was also associated with homelessness, nonwhite ethnicity, and a larger number of any charges and of charges for violent crimes during the previous 12 months.
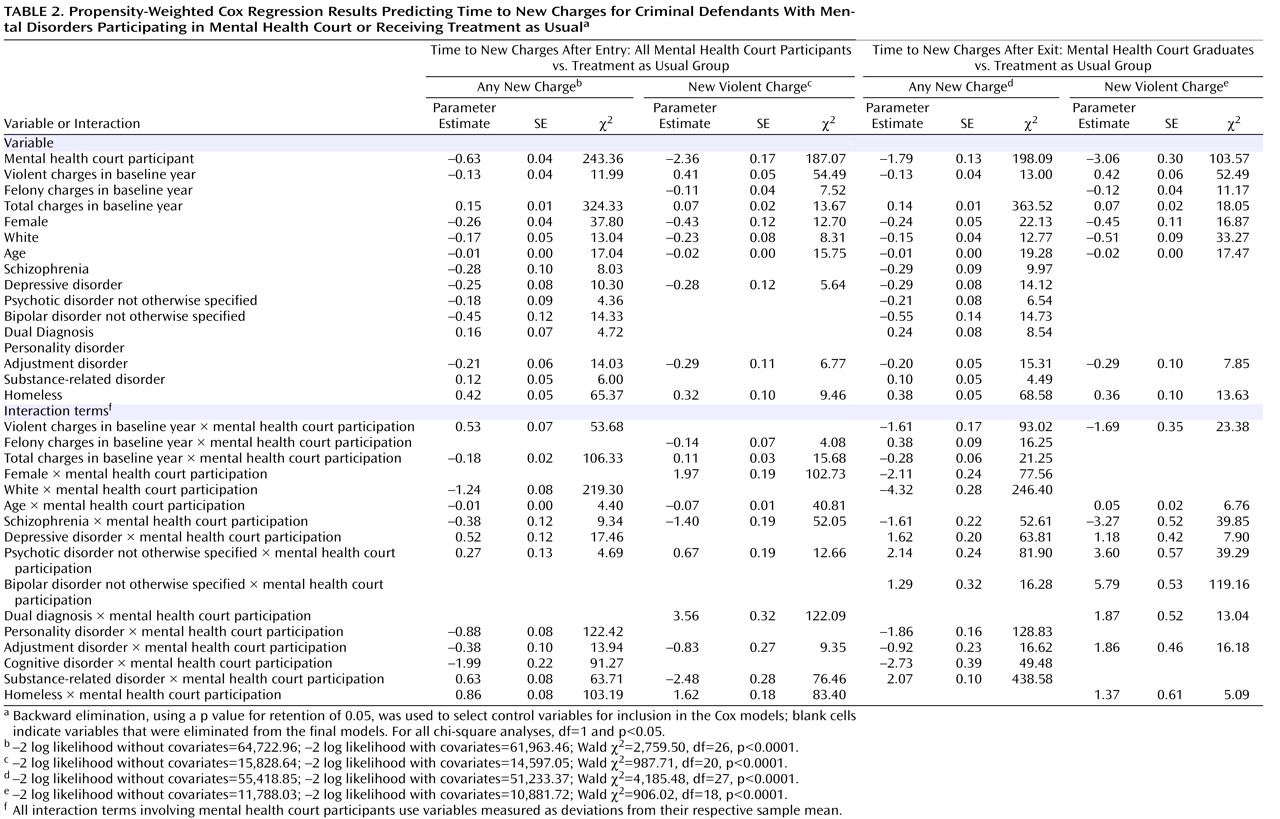
Intent-to-Treat Analyses
To assess whether participation in mental health court was associated with an increase in time to new charges, we conducted survival analyses comparing the mental health court and treatment as usual groups. After controlling for the propensity scores, demographic variables, diagnosis, and number and type of charges during the 12-month baseline period, the Cox proportional hazards models showed that mental health court participation predicted a longer time to any new charge (B=–0.63, p<0.0001) and longer time to a new violent charge (B=–2.36, p<0.0001) (see
Table 2 ).
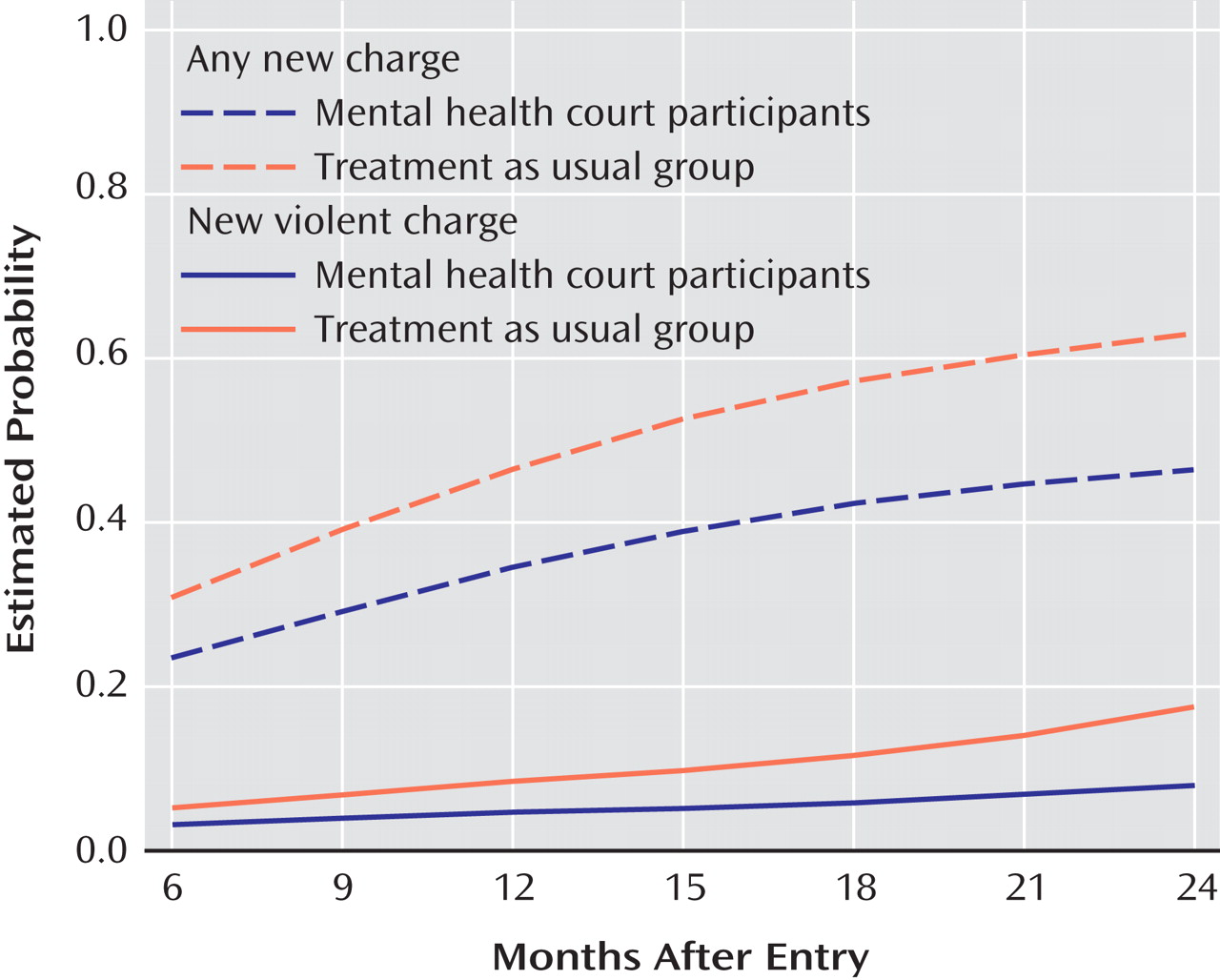
Figure 1 plots the estimated average cumulative probability of a new charge, conditional on the covariates, as a function of months after entry to mental health court or treatment as usual based on the Cox model. The vertical distance between the two curves is the estimated effect of mental health court participation. (
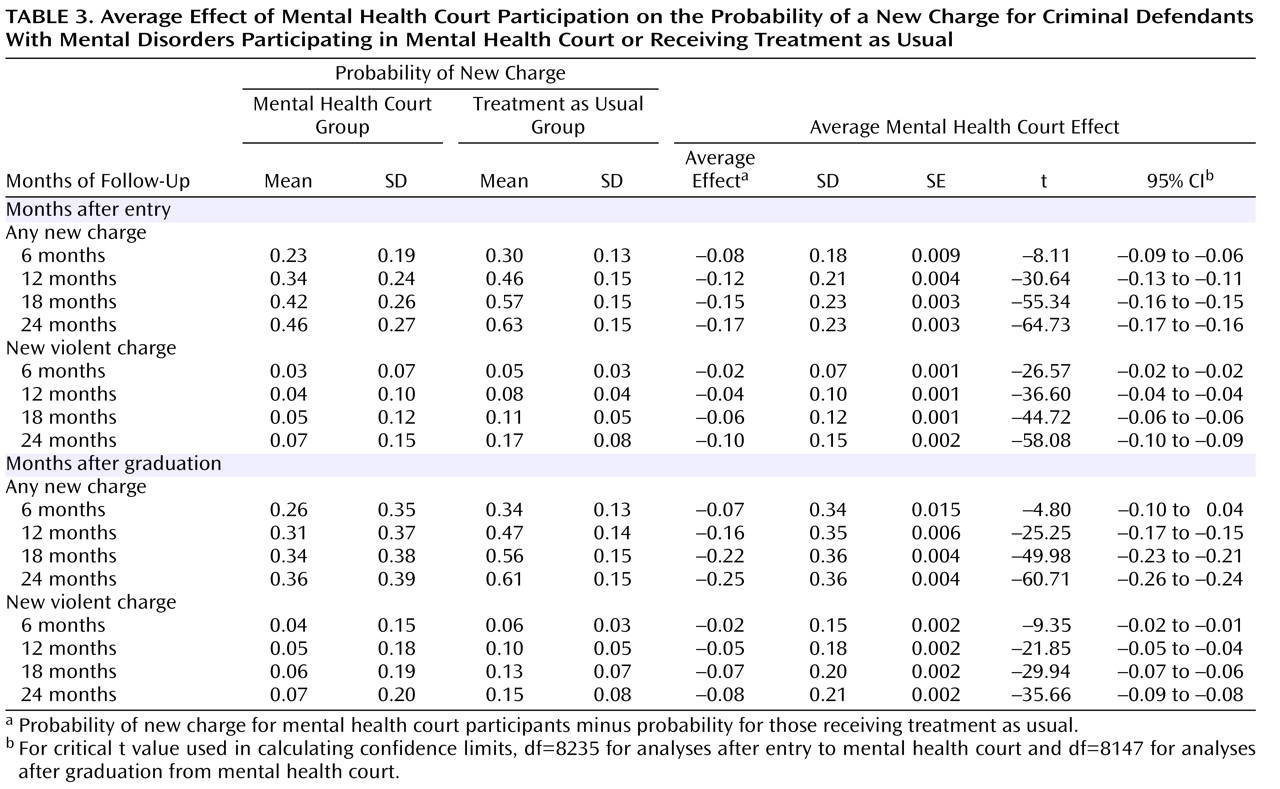
Table 3 summarizes the plots at 6-month intervals and reports the 95% confidence intervals [CIs] for the effect of mental health court participation on the probability of a new charge.)
Figure 1 shows that the average effect of mental health court participation on reducing the probability of new charges becomes more evident over time. By 18 months, the cumulative probability of any new charge for the mental health court and treatment as usual groups, respectively, was 0.42 and 0.57; the average change in the probability of a new charge due to mental health court participation was –0.15 (95% CI=–0.16 to –0.15), which represents a 26% (0.15/0.57) reduction. Similar patterns were evident in new violent charges, although violence was uncommon in both groups. At 18 months, the cumulative probability of a new violent charge for the mental health court and treatment as usual groups, respectively, was 0.05 and 0.11; the average effect of mental health court participation on the probability of a new violent charge was –0.06 (95% CI=–0.06 to –0.06), which represents a 55% (0.06/0.11) reduction.
Outcomes Associated With Completion of the Mental Health Court Program
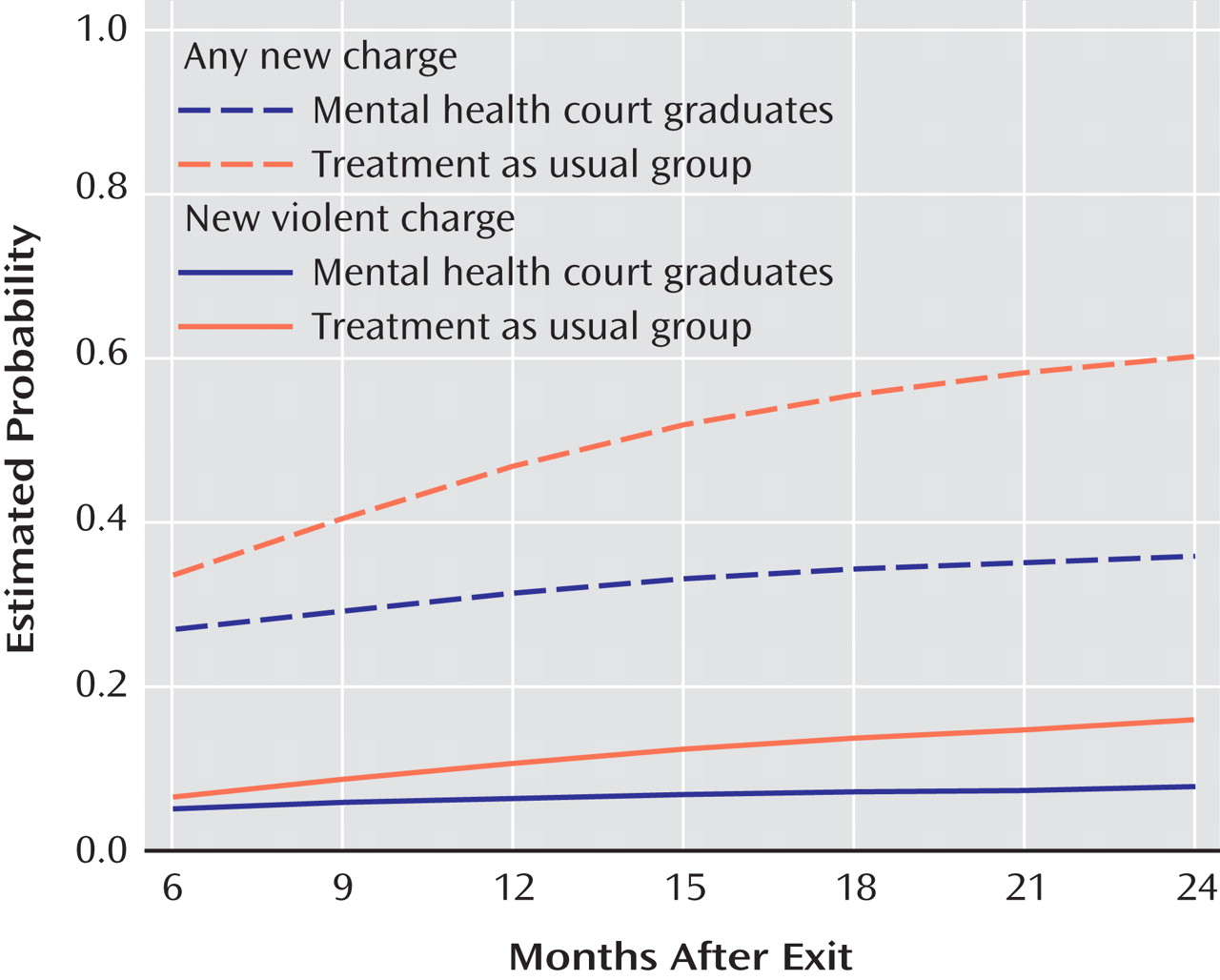
To assess the extent to which completion of the mental health court program was associated with maintenance of reduced recidivism after graduation, we conducted survival analyses with Cox proportional hazards models that compared mental health court graduates and individuals who received treatment as usual (see
Table 2 ). Mental health court graduates continued to show longer time before any new charges (B=–1.79, p<0.0001) and new violent charges (B=–3.06, p<0.0001) after graduating compared with those who received treatment as usual.
Figure 2 illustrates these findings. For example, at 18 months, the cumulative probability of any new charge for mental health court graduates and individuals who received treatment as usual, respectively, was 0.34 and 0.56. The average effect of mental health court on the probability of any new charge was a change of –0.22 (95% CI=–0.23 to –0.21) at 18 months, which represents a 39% (0.22/0.56) reduction (see
Table 3 ). Similar patterns were evident for new violent charges, although violence was uncommon in both groups. The cumulative probability of a new violent charge for mental health court graduates and individuals who received treatment as usual, respectively, was 0.06 and 0.13 at 18 months (average mental health court effect=–0.07, 95% CI=–0.07 to –0.06), a reduction of 54% (0.07/0.13).
Discussion
These results support the effectiveness of a mental health court in reducing the involvement of persons with mental disorders in the criminal justice system. Based on an intent-to-treat sample (i.e., all of those who enrolled in mental health court, regardless of whether they successfully completed the program), mental health court participants showed a longer time without any new charges or new charges for violent crimes compared with similar individuals who did not participate in the program. Survival analysis showed that the reductions in the likelihood of new charges were more substantial with follow-up of more than 1 year after enrollment in mental health court; for example, at 18 months, the likelihood of mental health court participants being charged with any new crimes was about 26% lower than that of comparable individuals who received treatment as usual, and the likelihood of mental health court participants being charged with new violent crimes was 55% lower than that of individuals who received treatment as usual. Additional analyses showed that persons who graduated from the mental health court program maintained reduced recidivism after they were no longer under supervision of the court, in contrast to comparable persons who received treatment as usual. By 18 months, the risk of mental health court graduates being charged with any new offense was about 34 out of 100, compared with about 56 out of 100 for comparable persons who received treatment as usual, and the risk of mental health court graduates being charged with a new violent crime was about half that of the treatment as usual group (6 out of 100 compared with 13 out of 100).
These findings provide evidence of the potential for mental health courts to achieve their goal of reducing recidivism among people with mental disorders who are in the criminal justice system. Moreover, since the mental health court participants in this study included a substantial proportion of individuals who had been charged with felonies or violent offenses, it appears possible to expand the mental health court model beyond its original clientele of persons charged with nonviolent misdemeanors in a way that public safety is enhanced rather than compromised.
One of the limitations of this study was nonrandom assignment to mental health court. Although propensity weighting helps control for nonrandom assignment, it can only adjust for observed covariates, and it may not have adequately adjusted for unobserved variables that may have influenced selection into mental health court (e.g., as participants who entered mental health court voluntarily agreed to have their cases handled in mental health court rather than traditional court, it is possible that they differed in unobserved variables such as treatment motivation). Although the effectiveness of our propensity score analysis in predicting selection to mental health court reduces this risk, the design does not preclude the possibility that selection bias affected the results. Another limitation is that our arrest data included arrests only in San Francisco and was not sensitive to possible arrests of the study and comparison subjects in other jurisdictions. However, since the mental health court participants were under the supervision of the court and therefore located in San Francisco for much of the study period, any bias toward underdetection of recidivism because of out-of-county arrests would be unlikely to have favored the mental health court group. Finally, because the structure of mental health courts varies across jurisdictions, the generalizability of the findings of this study may be affected by the extent to which a given mental health court is similar to the San Francisco mental health court; future multisite studies may help clarify this issue.
Mental health courts have been less controversial than other mechanisms for leveraging adherence to community treatment, such as outpatient commitment
(30,
31), possibly because rather than applying the leverage on the basis of a prediction of future deterioration, these courts aim to reduce criminal involvement of people already in the criminal justice system. Findings supporting the effectiveness of mental health courts in reducing recidivism suggest the need for additional research on the mechanisms that account for such outcomes. Research is needed on the extent to which mental health courts achieve goals such as treatment linkage and symptom reduction and whether these variables account for reducing recidivism. Research also is needed to determine what client characteristics are associated with more or less favorable outcomes and what structural characteristics of mental health courts (e.g., the extent to which sanctions are used) lead to better or worse outcomes.