Bipolar disorder is the sixth leading cause of disability worldwide
(1) . Although the severity of mood episodes is the major determinant of patients’ ability to work or have relationships, many patients experience functional impairments, even during euthymic periods
(2 –
5) . For example, across a 12-month follow-up of hospitalized patients with mania, 48% recovered clinically, but only 24% recovered functionally
(6) .
Randomized controlled trials have established the efficacy of manual-based, disorder-specific psychosocial treatments in conjunction with pharmacotherapy in preventing recurrences of bipolar illness over 1–2 years
(7) . Surprisingly, few of these studies report on functional outcomes (but see references
8 and
9 ). Thus, it is unclear whether the symptomatic benefits associated with psychosocial interventions translate into improvements in functioning, and if so, what the time course of such improvements might be.
This study compared the effectiveness of three forms of intensive psychotherapy (30 sessions over 9 months) with a brief psychoeducational treatment (three sessions over 6 weeks) in combination with pharmacotherapy in enhancing functioning following a bipolar depressive episode. Participants were treated within the randomized acute depression pathway of the multisite Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD
[10] ). Previously, we reported that the three intensive psychosocial treatments in STEP-BD—cognitive behavior therapy (CBT), family-focused therapy, and interpersonal and social rhythm therapy—were superior to brief psychoeducation in hastening recovery from depression and increasing the number of months well during a 1-year period
(11) . In the present study, we undertook a particularly conservative approach to examining the effects of psychotherapy on functional outcomes (relationships, satisfaction with activities, work/role functioning, and recreation) by examining whether intensive psychotherapy affects functioning above and beyond its effects on depression.
Method
Patients
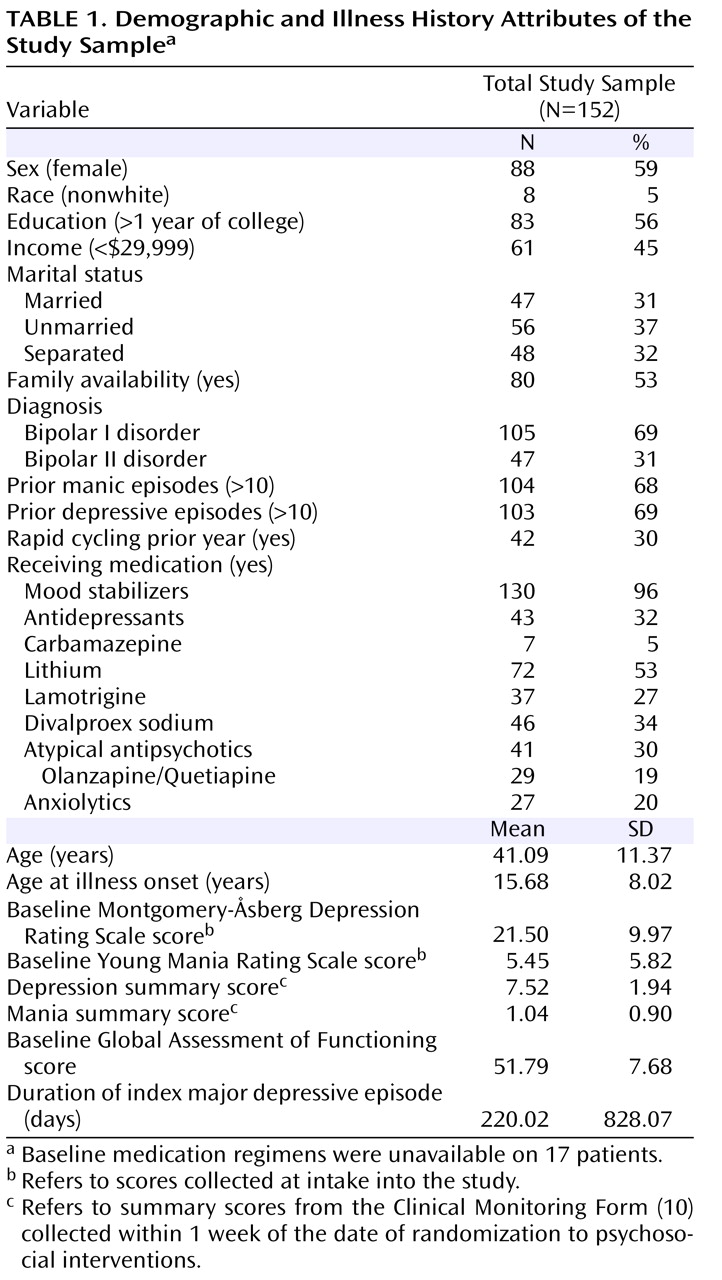
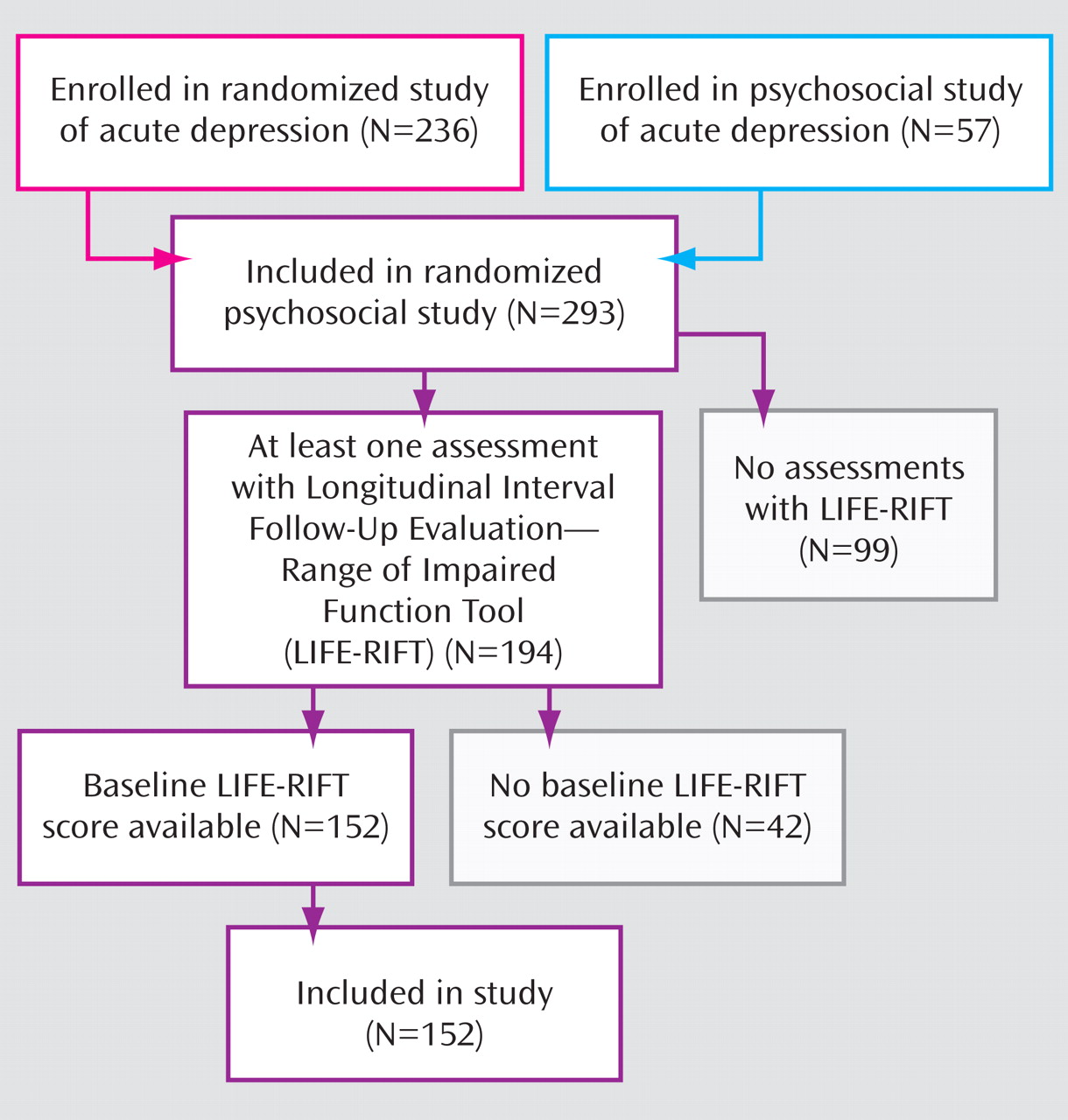
Participants were 152 patients with bipolar I disorder (N=105) or bipolar II disorder (N=47) (
Table 1 ). Details of the sampling procedures are given elsewhere
(11,
12) . Patients were recruited in one of 15 STEP-BD sites for one of two studies of psychosocial intervention in combination with pharmacotherapy in the depressive phase of bipolar disorder: the randomized acute depression study (N=236) or the psychosocial acute depression study (N=57). Of these 293 patients, 194 had at least one follow-up assessment in which the Longitudinal Interval Follow-Up Evaluation–Range of Impaired Functioning Tool (LIFE-RIFT)
(13,
14) was completed, but only 152 had baseline LIFE-RIFT scores (
Figure 1 ). These 152 patients composed the sample for this study.
The randomized acute depression and psychosocial acute depression studies had identical eligibility criteria, with the exception that patients in the randomized acute depression study were eligible for and agreed to participate in a 26-week trial of mood stabilizers plus antidepressants (paroxetine or bupropion) versus mood stabilizers plus placebo and were also willing to accept random assignment to psychosocial treatments. The psychosocial acute depression trial was initiated to accommodate participants who were eligible for psychotherapy but ineligible for the randomized acute depression trial because of a history of poor response or intolerance to bupropion and paroxetine. Participants also met the following inclusion criteria: 1) age ≥18 years, 2) meeting DSM-IV criteria for bipolar I or II disorder with a current major depressive episode, 3) concurrently treated with a mood stabilizer or willing to initiate mood stabilizer treatment, 4) not currently in weekly or biweekly psychotherapy, and 5) English-speaking. Exclusion criteria were 1) DSM-IV substance misuse disorders (excluding nicotine), 2) pregnancy or planning pregnancy in the next year (randomized acute depression study only), or 3) requiring initiating or changing the dose of an antipsychotic medication (randomized acute depression study only).
All 15 study sites received approval through their respective human subject review boards. After receiving a thorough description of the study from research staff members, participants provided written informed consent.
Diagnosis
Study physicians confirmed the presence of bipolar I or II disorder based on the Affective Disorders Evaluation, a structured interview that included adaptations of the mood modules of DSM-IV
(15,
16) . A second clinician confirmed the diagnosis and associated comorbid disorders using the Mini-International Neuropsychiatric Interview, version 5.0
(17) . Disagreements were resolved by consensus agreement.
Study Design
Once patients met study eligibility criteria, they were randomly assigned to 30 1-hour sessions (21 weekly and nine biweekly) of intensive psychosocial treatment (interpersonal and social rhythm therapy, family-focused therapy, or CBT) or three 1-hour sessions of collaborative care treatment over 6 weeks. Stratification variables included study site, bipolar I or bipolar II status, and, if simultaneously in the randomized acute depression study, pharmacological treatment (mood stabilizer with or without an antidepressant). Patients were assigned to intensive psychotherapy or collaborative care within each stratum using a 60:40 randomization formula, which resulted in 163 patients being assigned to intensive psychotherapy and 130 to collaborative care. Of the 152 participants with all baseline LIFE-RIFT scores, 84 were randomly assigned to intensive psychosocial treatment and 68 to collaborative care.
Each of the study sites chose to administer one type of intensive psychotherapy (e.g., CBT) based on its preferences and clinical expertise. A second modality (e.g., interpersonal and social rhythm therapy) was randomly assigned to the site. Of the 15 sites, 10 offered CBT, nine offered family-focused therapy, and 11 offered interpersonal and social rhythm therapy
(11) . All 15 sites offered the collaborative care condition. At the sites offering family-focused therapy, randomization was stratified further by whether family members (spouses, parents, or siblings) were available and willing to participate (80/152 [53%] of the sample). Patients without family members (72/152 [47%] of the sample) could only be randomly assigned to interpersonal and social rhythm therapy, CBT, or collaborative care. As a result, the number of patients assigned to family-focused therapy (N=13) was smaller than the number assigned to CBT (N=38) or interpersonal and social rhythm therapy (N=33).
Pharmacological Intervention
The 236 patients in the randomized acute depression protocol were randomly assigned to double-blind pharmacotherapy with mood stabilizers (lithium, valproate, carbamazepine, or another Food and Drug Administration-approved antimanic agent) plus placebo or mood stabilizers plus antidepressants. The 57 patients in the psychosocial acute depression trial received pharmacotherapy based on STEP-BD guidelines for evidence-based practice and in accordance with physician-patient agreement
(10) .
Psychosocial Intervention
CBT
Individual CBT consisted of four components: psychoeducation about bipolar disorder, including strategies for detecting and intervening with early signs of recurrence; behavioral activation exercises; problem solving; and cognitive restructuring
(18) . In the early treatment phases, clinicians challenged patients’ negative self-statements and encouraged balanced interpretations of life events. During later phases, clinicians and patients evaluated the validity of core dysfunctional beliefs.
Interpersonal and social rhythm therapy
Individual interpersonal and social rhythm therapy emphasized the regularity of sleep/wake rhythms to maintain mood stability
(19) . Early sessions focused on identifying a key interpersonal problem area (in the areas of grief, role disputes, role transitions, or interpersonal deficits
[20] ). Patients were encouraged to record the timing of various daily and nightly activities, levels of social stimulation, sleep, and mood using the Social Rhythm Metric
(21) . Later in treatment, patients set targets for regulating social rhythms (e.g., when to sleep, exercise, and eat) and developed plans for continued rhythm stability when facing potentially disruptive events (e.g., loss of a job). In the final phase, clinicians and patients collaborated in developing preventive strategies related to the selected interpersonal problem area
(19) .
Family-focused treatment
Family-focused therapy involved patients and at least one family member (spouse, partner, parent, or sibling) and was implemented in three modules. Psychoeducation focused on recognizing early warning signs of recurrence and developing relapse prevention plans that involved multiple family members
(22) . Patients and relatives developed a shared understanding of environmental factors that increased the patients’ vulnerability to recurrences and addressed barriers to medication adherence. Families were acquainted with the role of stress—notably, high expressed emotion interchanges—as both a cause and consequence of mood symptoms
(23) . The intermediate and later treatment phases focused on training in effective family communication (behavioral rehearsal of effective speaking and listening skills) and problem solving skills.
Collaborative care
Patients received a self-care workbook and an educational videotape, which included information about the diagnosis, course, treatment, and self-management of bipolar disorder. The three collaborative care sessions focused on implementing self-management tools (e.g., mood and sleep monitoring) and developing an individualized relapse prevention plan.
Treatment Integrity
Details of the therapist training and monitoring procedures are reported elsewhere
(11) . Rates of therapist fidelity, defined as sessions rated above a predetermined adherence threshold, were 86% for CBT (167 sessions), 86% for family-focused therapy (66 sessions), 82% for interpersonal and social rhythm therapy (139 sessions), and 89% for collaborative care (89 sessions). These rates did not differ across modalities (χ
2 =2.12, df=3, p=0.55).
Measures
Clinical evaluators who were not involved in the psychosocial treatments assessed patients’ levels of depression (using the Montgomery-Åsberg Depression Rating Scale
[24] ) and LIFE-RIFT role functioning at entry into the randomized study and then every 3 months for the 9-month period of active psychosocial treatment. Each interview covered the final week of the prior interval.
The LIFE-RIFT was validated previously on samples of individuals with unipolar and bipolar disorder, with adequate internal consistency and interrater agreement
(13,
14) . The measure assigns scores from 1 (no impairment/very good functioning) to 5 (very poor/severe impairment) to each of the following four domains: relationships (family, children, or friends), satisfaction (contentment and fulfillment from activities with family and friends, job, and finances), work/role performance (employment, household, or student roles), and recreational activities/hobbies. In cases in which the domain subscales yielded different functioning scores (e.g., relations with spouse were poorer than with children), the more impaired score was used to characterize the domain. A total score was calculated as the sum of the individual subscales.
Data Analysis
Mixed-effects regression models with random subject effects
(25), using PROC MIXED in SAS
(26), were used to test the relations between treatment condition (coded as intensive treatment versus collaborative care) and LIFE-RIFT total scores and scores for relationship, satisfaction, work, and recreation at the 3-, 6-, and 9-month evaluations (considered simultaneously). Covariates in these models included baseline LIFE-RIFT scores, bipolar I or bipolar II disorder status, whether the patient received pharmacotherapy through random assignment (randomized acute depression study) or best practices agreement (psychosocial acute depression study), and study site. To determine whether psychosocial treatments affected life functioning scores independently of their effects on depression, we covaried Montgomery-Åsberg Depression Rating Scale depression scores at each point of follow-up. All statistical comparisons were two-tailed.
Results
Sample Characteristics
All patients who entered into the STEP-BD acute depression studies between September 1999 and July 2005 were included. The fact that only 152 of the 293 participants in the randomized acute depression or psychosocial acute depression psychosocial studies had all baseline LIFE-RIFT scores reflected site-to-site variability in the completion of the study’s intake battery (
Figure 1 ). Patients with baseline LIFE-RIFT scores did not differ from patients without baseline scores (N=141) on demographic, diagnostic (e.g., bipolar I versus bipolar II disorder), illness severity (e.g., baseline Montgomery-Åsberg Depression Rating Scale scores), or treatment variables, with the following exceptions. Global Assessment of Functioning Scale scores
(27) at the time of randomization were lower among patients with (51.8 [SD=7.7]) than without (54.3 [SD=7.9]) baseline LIFE-RIFT scores (χ
2 =4.59, df=1, p=0.03), and patients with baseline LIFE-RIFT scores were more likely (53%) to be receiving lithium at study entry than patients without baseline LIFE-RIFT scores (38%) (χ
2 =6.07, df=1, p=0.01).
Comparison of Treatment Groups at Baseline
Patients in the intensive and collaborative care conditions did not differ at the time of randomization on any demographic, diagnostic, illness history, or current clinical state variable or the proportion of patients being treated with lithium, divalproex sodium, carbamazepine, lamotrigine, atypical/typical antipsychotics, antidepressants, or anxiolytics (all p values>0.10). There were no differences between patients in the intensive psychotherapy and collaborative care conditions (or between patients in any of the three intensive treatments) on baseline LIFE-RIFT total scores and scores on relationship, satisfaction, work, or recreation ([N=152] all p values>0.10).
Psychosocial Treatments and Functional Outcomes
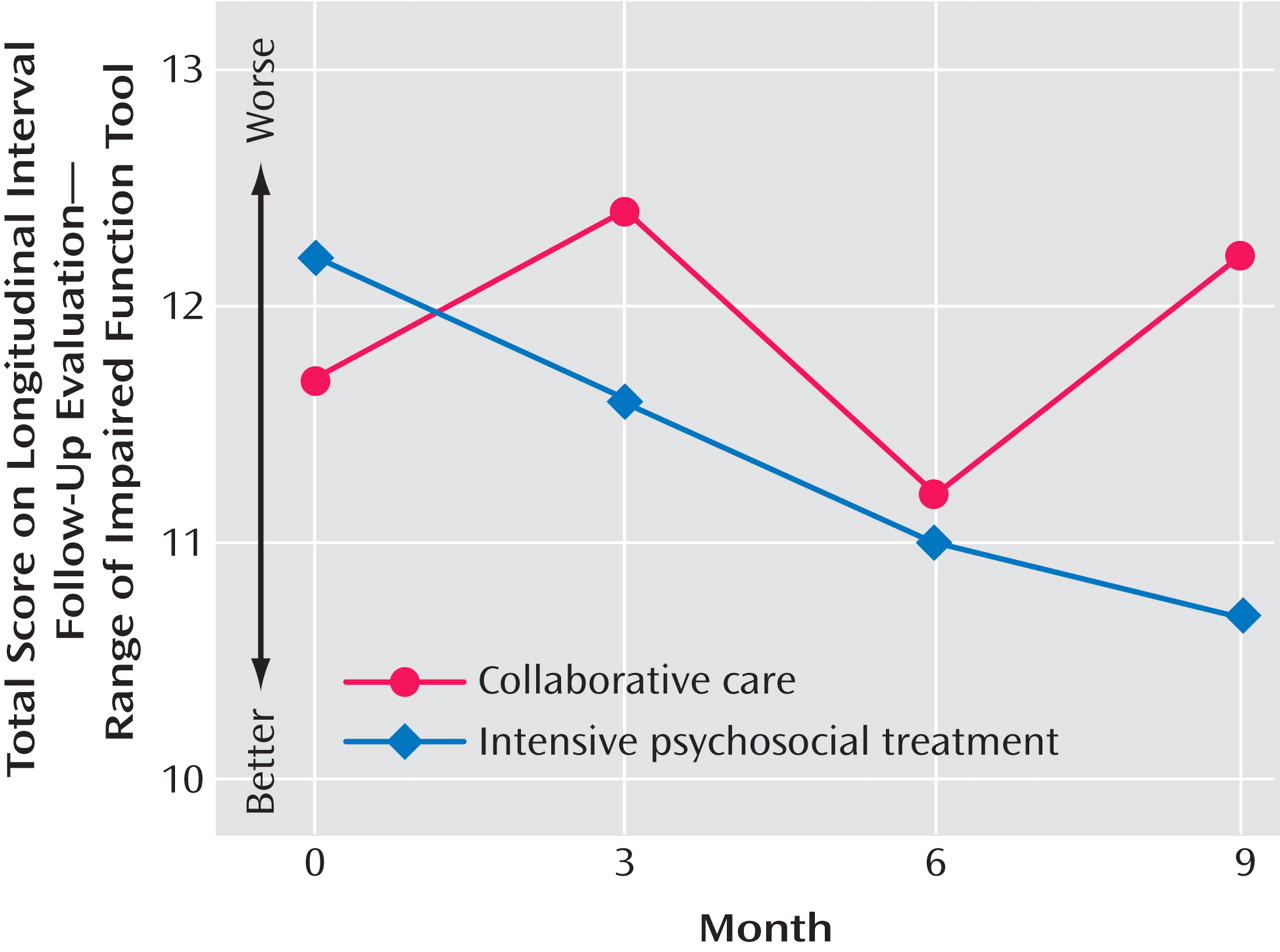
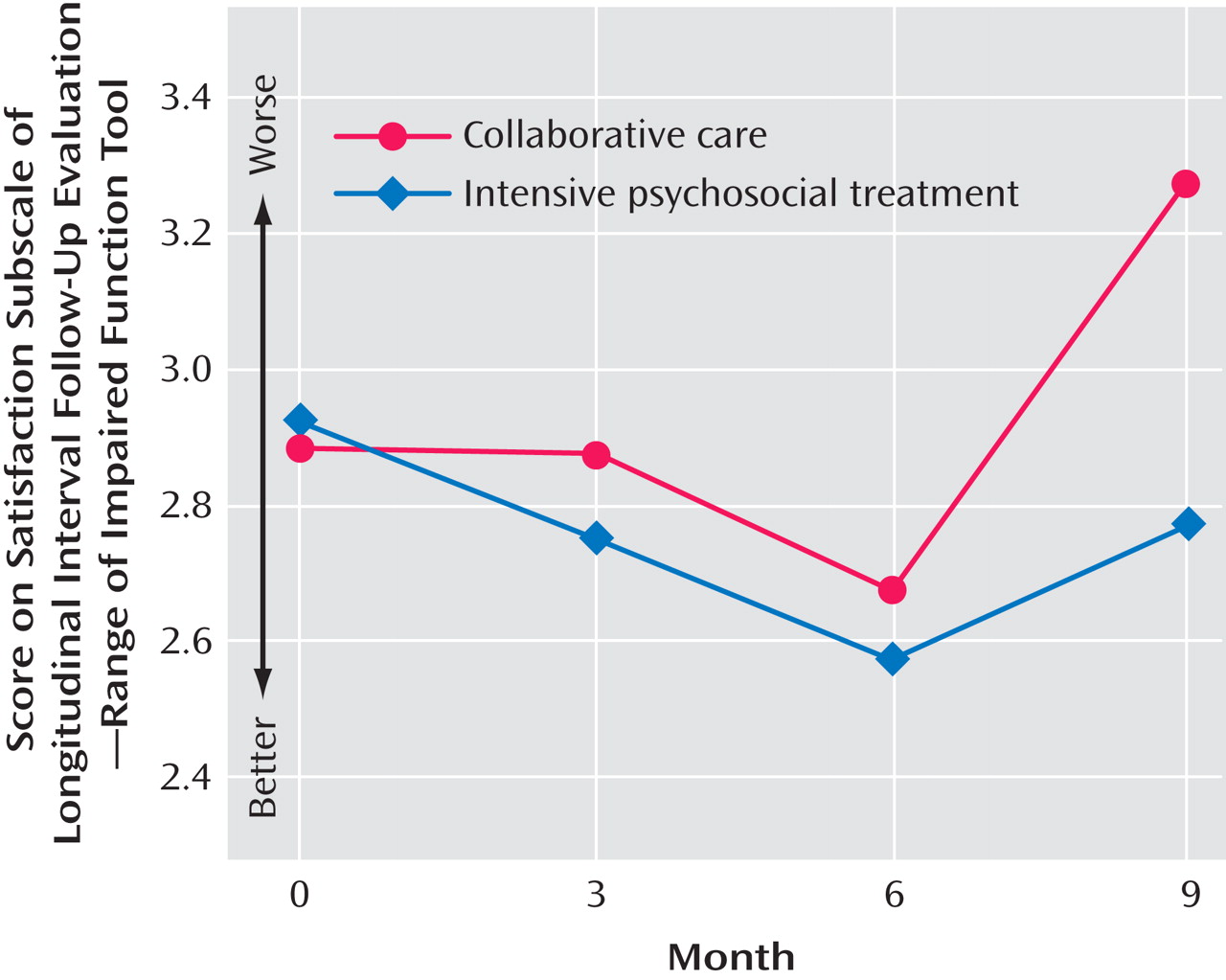
Baseline LIFE-RIFT total scores (F=13.60, df=1, 135, p=0.0003) and contemporaneous Montgomery-Åsberg Depression Rating Scale scores (F=154.60, df=1, 135, p<0.0001) were each significant predictors of LIFE-RIFT total scores over the 9-month study. When baseline LIFE-RIFT scores and concurrent Montgomery-Åsberg Depression Rating Scale scores were included in a mixed-effects regression model, a main effect of treatment condition was observed: patients in intensive psychosocial treatments had better LIFE-RIFT total scores over the 9-month study than patients in collaborative care (F=4.32, df=1, 135, p=0.04 [
Figure 2 ]). The treatment effect was independent of bipolar I disorder versus bipolar II disorder status, randomized acute depression versus psychosocial acute depression assignment, and study site; none of these variables were associated with follow-up functioning scores (all p values>0.10). Changes in LIFE-RIFT total scores, calculated as the difference between 9-month and baseline scores (range: –10.0 to 12.0), were –3.17 [SD=3.06] in the family-focused therapy group, –1.63 [SD=4.35] in the interpersonal and social rhythm therapy group, –1.05 [SD=4.77] in the CBT group, and –0.94 [SD=3.5] in the collaborative care group (more negative scores indicate greater improvement).
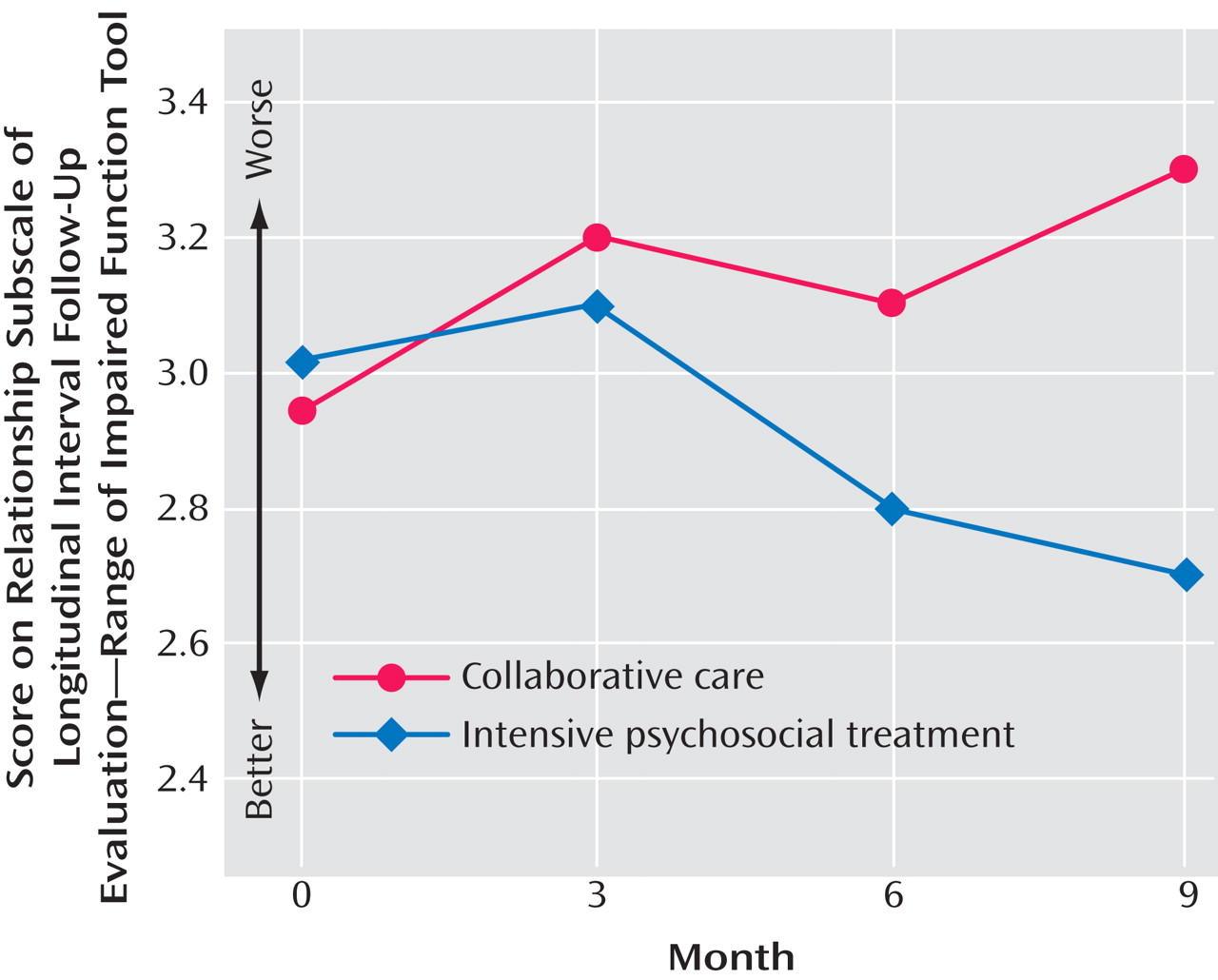
Next, we examined the effects of psychosocial treatment on each domain of functioning. Independent of the effects of baseline relationship scores (F=46.3, df=1, 141, p<0.0001) and concurrent Montgomery-Åsberg Depression Rating Scale scores (F=18.41, df=1, 141, p<0.0001) on follow-up LIFE-RIFT scores, patients in intensive treatment had better relationship functioning over 9 months than patients in collaborative care (F=5.26, df=1, 141, p=0.02) (
Figure 3 ). No effects of bipolar I versus bipolar II disorder status, randomized acute versus psychosocial acute depression, or site were found. Greater improvements in relationship functioning (the difference between 9-month and baseline scores; range: –4.0 to 4.0) were observed in all three intensive treatments (CBT: –0.45 [SD=1.64]; family-focused therapy: –0.29 [SD=2.06]; interpersonal and social rhythm therapy: –0.24 [SD=1.25]) relative to collaborative care (0.09 [SD=1.51]).
Treatment group (intensive treatment versus collaborative care) was significantly associated with LIFE-RIFT satisfaction scores over 9 months, even after all covariates were considered (F=3.98, df=1, 140, p=0.048 [
Figure 4 ]). Mean change scores in the treatment subgroups for satisfaction scores (range: –3.0 to 2.0) were as follows: family-focused therapy, –0.86 [SD=0.90]; interpersonal and social rhythm therapy, –0.29 [SD=1.40]; CBT, –0.10 [SD=1.17], and collaborative care, 0.0 [SD=1.25]. Baseline LIFE-RIFT satisfaction scores were not associated with follow-up satisfaction scores, nor was bipolar I or bipolar II disorder status, randomized acute depression or psychosocial acute depression assignment, or study site (p>0.10). However, concurrent Montgomery-Åsberg Depression Rating Scale scores were strongly related to satisfaction scores across the 9-month study (F=187.8, df=1, 140, p<0.001).
The intensive and collaborative care groups did not differ on LIFE-RIFT work/role functioning scores over the 9 months (F=0.30, df=1, 137, p=0.58). These scores were strongly associated with work functioning at baseline (F=12.34, df=1, 137, p=0.0006) and concurrent Montgomery-Åsberg Depression Rating Scale scores (F=76.04, df=1, 137, p<0.0001), but not with bipolar I versus bipolar II disorder, randomized acute versus psychosocial acute depression, or study site. Finally, there was no main effect of treatment on LIFE-RIFT recreation scores (F=1.29, df=1, 140, p=0.26). These scores were uniquely associated with concurrent Montgomery-Åsberg Depression Rating Scale scores (F=73.91, df=1, 140, p<0.0001), but not with any of the other terms in the model.
Discussion
This study examined questions that have received limited attention in treatment trials involving patients with bipolar disorder: Do psychosocial interventions improve social or vocational role functioning, and do the interventions achieve these improvements independently of their effects on depression severity? We compared three intensive (30-session) psychosocial treatments for bipolar depression (CBT, family-focused therapy, and interpersonal and social rhythm therapy) in combination with pharmacotherapy to three sessions of psychoeducation and pharmacotherapy over a 9-month period. The primary finding is that when compared with collaborative care, intensive psychosocial intervention significantly improved patients’ relationship functioning and satisfaction with life beyond the level of improvements expected from changes in depressed mood. The psychosocial interventions had no independent effects on work/role functioning or recreation scores.
Each of the intensive treatments studied addresses relationship functioning and life satisfaction in different ways. CBT encourages patients to challenge assumptions about interpersonal relationships, carry out behavioral experiments to test these assumptions, and increase engagement with others. In interpersonal and social rhythm therapy, patients learn about the bidirectional relationship between depressed mood and relationship problems and examine alternative ways of responding to interpersonal conflicts. Family-focused therapy addresses relationships with family members or close friends through direct rehearsal of effective communication skills and problem solving, and homework assignments to maximize the use of these skills in everyday interactions. All three treatments include problem solving to improve upon unsatisfactory life conditions (e.g., troubles with living situation, job, or finances) and strategies to manage mood states that interfere with the enjoyment of activities. As the case examples illustrate, changes in life conditions, self-esteem, mood, and functioning often occur among bipolar disorder patients undergoing intensive treatments, although these changes do not necessarily occur at the same time or as a direct result of each other.
This study had several limitations. First, the 9-month period of observation may not have been long enough to observe the full impact of intensive psychosocial treatments on role functioning, particularly for employment-related changes. Impaired vocational functioning may be a more stable attribute of bipolar disorder than mood symptoms. It may require several months of full remission from depression before patients feel ready even to contemplate a change in their employment status or to expand their recreational activities. Two of the studies that demonstrated effects of psychosocial interventions on the vocational functioning of bipolar patients followed patients for at least 18 months
(8,
9) . Furthermore, a subset of individuals with bipolar disorder experience significant deficits in neuropsychological functioning, even when euthymic
(28,
29) . These deficits are more likely to affect work functioning than relational functioning and were not addressed in the forms of psychotherapy tested within this study.
A second study limitation is that pharmacotherapy was not uniform among participants. Within the randomized acute depression protocol, medications given on entry (aside from study antidepressants) were generally not limited and could be changed at any point after patients recovered or left the protocol. Patients who received pharmacotherapy by random assignment (randomized acute depression study) did not differ in functional outcome scores from patients whose pharmacotherapy was determined by physician/patient agreement (psychosocial acute depression study). Nonetheless, patients with significant functional deterioration may have received higher doses or different medications than patients whose functioning was stable or improving. Thus, changes in pharmacotherapy during the study may have attenuated differences in outcomes that might otherwise have been observed between those who did and did not receive intensive psychosocial treatment.
Because this study did not include an attention control, we cannot determine whether the intensive treatments were associated with greater improvements in functioning because of their content or simply because more sessions were offered in the intensive than the collaborative care condition. Our earlier report from STEP-BD
(11) found no main effect of the number of sessions or interaction between treatment modality and the number of sessions in predicting recovery time. Future studies that include attention controls may be able to determine whether the level of therapist attention (up to 30 sessions) required in this trial is necessary to observe gains in psychosocial functioning.
This study, in combination with our prior report from STEP-BD, suggests that intensive psychosocial treatment is more effective than brief psychoeducation in stabilizing depressive symptoms and enhancing functioning following a bipolar depressive episode. These results are consistent with the broader literature indicating that combining psychosocial interventions with pharmacotherapy is more effective than pharmacotherapy alone for a variety of outcome domains relevant to bipolar disorder
(7) . Nonetheless, the study also points to the limitations of our existing treatment methods. Many of the patients in this study showed highly variable functioning scores in one or more domains and little overall improvement in functioning over 9 months, despite aggressively delivered psychosocial and pharmacological treatment regimens. Functioning scores during the treatment period were highly related to concurrent levels of depression in all analyses, and for most domains, baseline functioning scores accounted for a significant proportion of the outcome variance during treatment.
In addition to the psychoeducational therapies described in the present study, it may be that the cognitive remediation, social skills, or vocational rehabilitation programs found successful in schizophrenia
(30,
31) could be adapted to the treatment of individuals suffering from bipolar disorder, taking into account their generally higher levels of premorbid functioning. Such programs may be especially useful following remission from an episode of depression, when functional recovery would ordinarily be delayed.