“It makes me so upset I can’t stop myself.”
Individuals with borderline personality disorder have a notoriously difficult time with impulse control
(1), particularly in the context of stressors or negative emotional events. Due in part to the influences of uncontrolled emotion on their everyday decisions and behaviors, individuals with borderline personality disorder are difficult to treat. Brain mechanisms of this phenomenon are not well understood, possibly because they involve subtle influences of an emotional state or context on decisions that are not always inherently emotional. The increasing potential for using information about brain mechanisms of psychiatric conditions clinically has made understanding them a national priority
(2) . Yet identifying such mechanisms rigorously would entail forcing individuals with borderline personality disorder to repeatedly make hasty cognitive decisions during exposure to emotional contexts.
Despite the difficulties of arranging such a scenario, Silbersweig et al., in this issue of the Journal, have done so in individuals with and without borderline personality disorder during assessment using functional magnetic resonance imaging (fMRI). Subjects were asked to push a button for words printed in a standard font but not for italicized words. There were very few italicized words, and thus subjects quickly achieved a habit of pressing the button—impulse control was required in order for them not to press. Sometimes the words were positive or neutral, but sometimes they were negative. As might be expected, subjects with borderline personality disorder pushed the button more when they were not supposed to, particularly when the italicized words were negative.
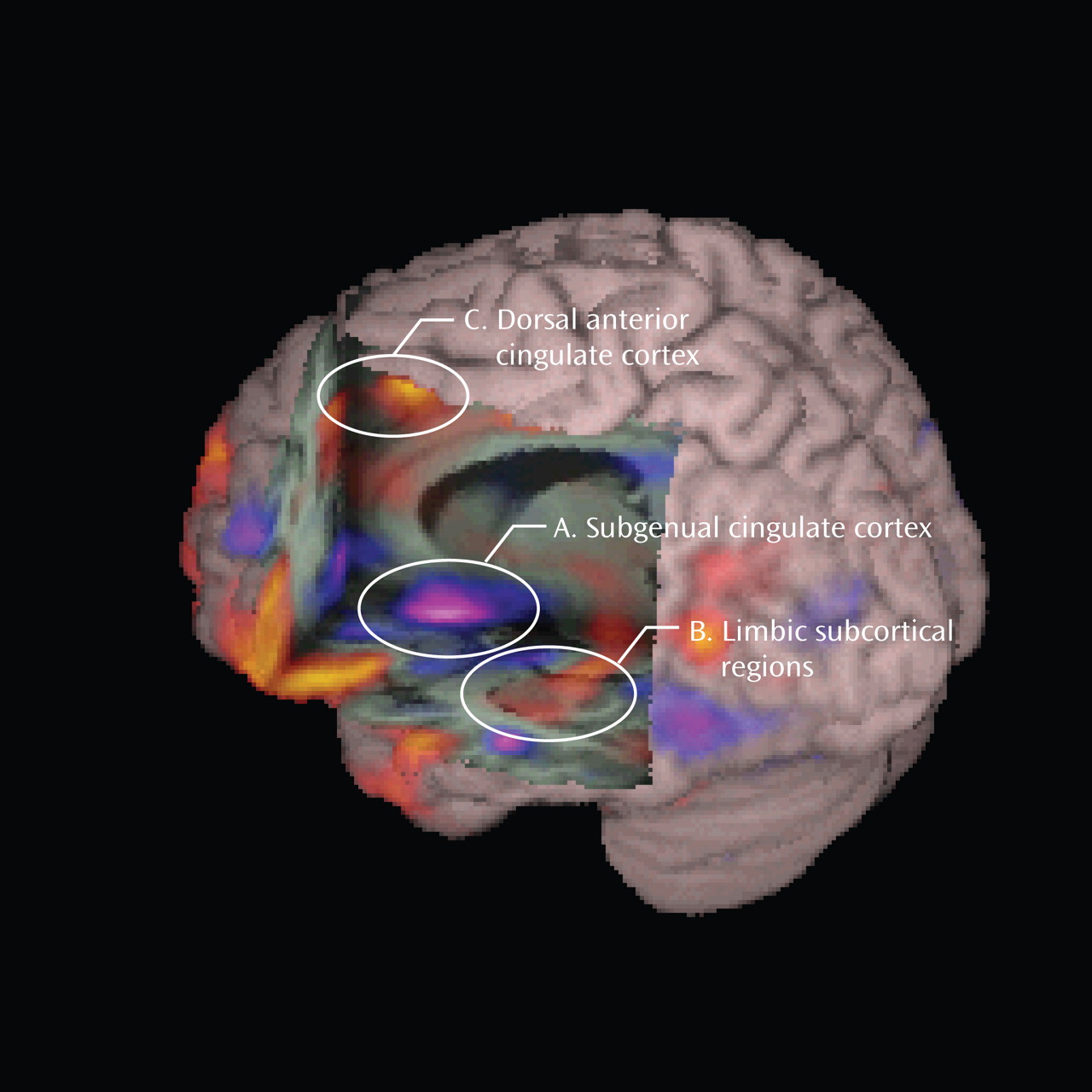
The authors’ fMRI data help to explain this behavioral result. When confronted with negative words on trials in which they were not supposed to push a button, healthy subjects displayed increased activity in the orbitofrontal and subgenual cingulate cortices, brain regions associated with emotion regulation
(3) and inhibition of limbic regions, including the amygdala
(4) . As shown in
Figure 1, which depicts differences in brain activity between individuals with borderline personality disorder and healthy comparison subjects, these increases did not occur in subjects with borderline personality disorder (e.g.,
Figure 1, section A illustrates the decreased change in subgenual cingulate activity), who instead experienced increased limbic activity (
Figure 1, section B). Thus, subjects with borderline personality disorder displayed brain responses associated with automatic emotional reactions; they may not have flexibly used brain mechanisms that would appropriately regulate these emotions.
In addition, in response to negative words, subjects with borderline personality disorder also showed increased activity in the dorsal anterior cingulate cortex (
Figure 1, section C), a region associated with detection of conflict in deciding what response to make
(5) . This activity suggests that although they were not able to exercise impulse control, they were very aware that they had to devote other resources to monitoring this situation.
The study has a number of strengths that facilitate translation of its results to the clinic. In particular, the design was carefully tuned to the specific pathology the authors were investigating. Clearly, such applicability to understanding contextual impulse control in borderline personality disorder would not have occurred were they to have employed a more conventional imaging design, such as simply contrasting negative and neutral stimuli or conditions in which button presses were or were not required. Rather, as borderline personality disorder sits at the intersection of cognition and emotion, the confluence of cognitive and emotional tasks revealed fundamental mechanisms of emotional influences during the cognitive task. The work was systematic. The authors piloted the task and reported on its behavior in healthy comparison subjects before moving to a patient population (e.g.,
6 ). Thus, the study becomes one of the first to probe this interaction of cognition and emotion in borderline personality disorder (a central disruption of the disorder) using neuroimaging. The design is rigorous, and the clinical sample is comparable with other clinical neuroimaging studies. The results are consistent with existing theories regarding disruptions in limbic, ventromedial, and orbitofrontal regions in borderline personality disorder.
Moving forward, it will be important to show that the apparent specificity of this finding actually reflects the loss of impulse control in borderline personality disorder. For example, it would be interesting to show that similar brain responses do not occur in individuals with another psychopathology (but not difficulty in impulse control), e.g., depressed individuals. Similarly, it would be important to understand whether the observed abnormalities only occur during decision making tasks or whether they would also occur when individuals with borderline personality disorder are passively exposed to any negative information. Also, causal relationships between the amygdala, subgenual cingulate, and behavioral performance could not be gleaned from these results. Thus, whether the observed increased amygdala activity and decreased subgenual cingulate activity following negative words arose because of fundamental deficits in the ability of individuals with borderline personality disorder to recruit regulatory resources, or whether inhibition of these regions by the amygdala itself (e.g., because of its hyper-activity) caused the failure to regulate, is left for another study that could pick up where this one leaves off. Relating behavioral deficits to brain imaging data in future studies and more closely inspecting the nature of covariation between the amygdala and subgenual cingulate could also help to bolster a causal story.
These future directions notwithstanding, with the data from just this study, we can begin to infer that when individuals with borderline personality disorder display decreased impulse control, this loss of impulse control may reflect a deficit in recruitment of brain mechanisms of emotion regulation, and this process may be potentiated by context. Particularly stressful or negative contexts could lead to more impaired impulse control.
An implication for psychotherapy process might be that it is important to address contextual factors when considering impulse control in borderline personality disorder. Moreover, the fMRI results implicate brain regions that have been shown to be increasingly associated with treatment of affective disorder, a frequent comorbidity of borderline personality disorder. Stimulation of the subgenual cingulate region is effective for treatment-resistant depression
(7), and depressed individuals with increased amygdala and decreased subgenual cingulate reactivity respond to cognitive therapy
(8), suggesting a possible similar mechanism of action for cognitive therapy in borderline personality disorder. Together, results from this study suggest that the specific behavioral and brain mechanisms implicated in decreased impulse control in borderline personality disorder could be addressed by known treatments.
Ideally, these insights gathered at the crossroads of cognitive and affective neuroscience will contribute to the growing tendency of translating neuroimaging data to the clinic. In the past, basic neuroimaging findings have often remained separate from clinical practice. But with designs such as that used by Silbersweig et al., which so closely reflects the observed clinical phenomena, and results that appear so closely aligned with clinical studies, it is increasingly easy to recommend that clinicians read this study carefully and begin to apply its lessons, ideally to better design and monitor cognitive and pharmacological treatments by addressing the underlying neurobiology of borderline personality disorder.